Some studies have showed that seasonality is an important determinant of vitamin D (vitD) status.
ObjectiveWe evaluated whether there are differences in individual trends of serum vitD level over one year in asthmatic and rhinitic children.
Materials and methodsNinety-two asthmatic and rhinitic paediatric patients were followed up for one year and their serum vitD level was detected at three-month intervals, once in each season.
ResultsWe observed higher vitD levels at the end of summer and lower at the end of winter. However, the individual seasonal trend was very variable and unpredictable. If it is true that in a given season the majority of patients followed one direction (increase or decrease of serum vitD levels), nevertheless a substantial percentage behaved differently and unpredictably. For example, at the end of spring, 70% of patients showed an increase in serum vitD levels, but 30% showed a decrease. In addition, five individuals had a value ≥50ng/ml in September and showed serum vitD levels ≥30ng/ml throughout the year; 16 patients presented vitD value ≥40ng/ml in September and always had ≥20ng/ml in the other months.
ConclusionsThe wide and unpredictable variability of the individual trend of serum vitD levels should be taken into account before deciding whether or not a drug supplementation is appropriate.
Vitamin D (vitD) is a potent immunomodulator capable of dampening inflammatory signals in several cell types involved in the asthmatic response.1 Its deficiency has been associated with increased inflammation, exacerbations, and overall poor outcomes in patients with asthma.1–3 However, other authors4 did not show strong evidence that, among adults with asthma, having a low serum vitD or being a non-user of vitamin D supplement was associated with an increased risk of poorly controlled asthma. Consequentially, findings obtained from clinical trials are controversial and do not unequivocally support a beneficial role of vitD in asthma.1
Steroid use, age, body mass index, gender, and season are major confounding factors in investigating the association between allergic diseases and vitD levels: these factors can produce different results among studies that examine vitD levels.5 In particular, some studies showed that seasonal variation is an important determinant of vitD status: a lower concentration of this molecule has been observed during the months of the year with the shortest daylight period.6,7 It has been suggested that to achieve a correct diagnosis of vitD deficiency, blood sampling seasonality should be regarded as an important pre-analytical factor8 and that the use of a single vitD measurement may misclassify yearlong vitD exposure.9
Batmaz et al.10 first measured serum vitD levels in each season of the year in asthmatic children and investigated the seasonal relationship between vitD levels and asthma control, lung function tests and cytokines during a one-year period, among thirty 7–17-year-old asthmatic children. These authors10 reported that asthma control measures, lung function tests and IgE levels in asthmatic children were significantly related to serum vitD levels, independently from age, body mass index, inhaled corticosteroid use, sun exposure and season.
The aim of our study was to evaluate whether in asthmatic and rhinitic children, in addition to differences in seasonal means, there are also differences in individual trends of serum vitD levels over one year.
Materials and methodsAsthmatic and rhinitic patients aged 6–16 years admitted to the Paediatric Allergy Unit of Policlinico Gemelli Universitary Foundation in Rome between February 2015 and June 2016 were included. All patients were diagnosed and classified according to the asthma11,12 and rhinitis13 guidelines.Patients who had persistent asthma or rhinitis for the last 12 months were recruited. Patients with chronic lung diseases other than asthma, with diseases that affect the vitD levels (liver or kidney diseases, malabsorption), and who used drugs containing vitD or affecting the vitD levels (systemic steroids, antiepileptic drugs) were excluded.
Recruited patients were followed up for one year and were evaluated at three-month intervals, once in each season, performing: (a) serum vitD level (see later for measurement techniques); (b) total IgE level analyzed by the nephelometric method; (c) eosinophil count analyzed by flow cytometry. All blood was drawn at the same time in the morning, i.e. at 9 a.m., after an eight-hour fasting period.
Written and oral consents from the patients and their parents were obtained, and the study was approved by the local ethical committee.
Measurement of serum vitDVitD measurement was performed using two different methods (for organizational reasons related to the analysis laboratory): up to December 2015 using DiaSorin Liaison Total method, and from January 2016 using Siemens ADVIA Centaur method, both CLIA immunoluminescence tests. To normalize the data coming from the two different methods, similarly to what has already been done in the literature,14 a linear regression model was used built on a sample of 20 patients for whom measurement was available with both methods. All the measurements obtained with the Siemens method were converted to the predicted Diasorin values using the following equation: Diasorin=Siemens×1.07–11.
Serum vitD was measured in March (vitD1), June (vitD2), September (vitD3), December (vitD4): it respectively reflects the amount of vitD in the winter, spring, summer and autumn seasons. Individual longitudinal trends of serum vitD levels were analyzed.
Patients were asked not to change their usual lifestyle, especially about sun exposure, and not to take vitD, except for that contained in foods of their usual diet, for all the duration of the study.
At the end of the study the children's parents were asked to answer a short survey about sun exposure of their children.
Statistical analysisThe collected data were inserted into an Excel spreadsheet (Microsoft, Redmond, WA, USA), and were re-encoded so that they could be analyzed ensuring the patients’ anonymity. The distribution of numerical variables was analyzed by the Shapiro–Wilk normality test. The demographic and clinical characteristics of the patients were reported as mean and standard deviation or median and range, as appropriate, for continuous variables, and as relative and absolute frequencies for categorical variables. VitD assays were ‘tracked’ with respect to the day of the year in which they were measured, and curves were built reflecting the seasonal trend during the year. Serial measurements of the serum vitD levels were evaluated using an ANOVA model for one-way repeated measurements. The vitD variable for each season was dichotomized, creating three variables using the following values as cut-off: <10; <20; <30.15 The seasonal comparison between dichotomous variables was made by the McNemar test. The post hoc comparison for the single seasons was made through t tests for data matched with Bonferroni correction. The difference in seasonal vitD values in relation to the underlying pathological condition (asthmatic vs. rhinitic) and sex (males vs. females) was tested by the t test for independent samples. Finally, the seasonal trend of serum vitD levels was correlated with serum levels of total IgE and eosinophils through the Spearman test.
The significance value was set a priori at 0.05. Statistical analyses were conducted using the IC STATA 12 software for Mac.
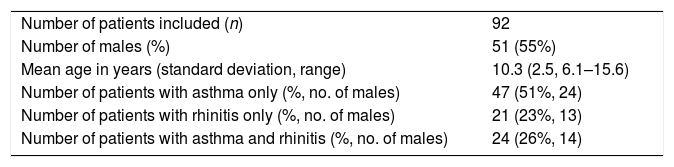
ResultsOne hundred and eleven patients were enrolled. Nineteen (17%) of them were excluded from the final analysis of the data because they did not perform all the planned controls or because they took vitD supplement during the study. Patient demographics are described in Table 1.
Demographic characteristics of patients included in the final analysis of the data.
| Number of patients included (n) | 92 |
| Number of males (%) | 51 (55%) |
| Mean age in years (standard deviation, range) | 10.3 (2.5, 6.1–15.6) |
| Number of patients with asthma only (%, no. of males) | 47 (51%, 24) |
| Number of patients with rhinitis only (%, no. of males) | 21 (23%, 13) |
| Number of patients with asthma and rhinitis (%, no. of males) | 24 (26%, 14) |
All patients were living in Rome or in its province, central area of Lazio, Central Italy (latitude between 41°N and 42°N).
A total of 368 measurements of serum vitD were performed. 94/368 (30.4%) measurements were performed with the Siemens method, 76 (82.6%) in March and 18 (19.1%) in June. Eighteen (19.1%) patients had two Siemens measurements; 57 (60.6%) patients had only one Siemens measurement; 17 (18.3%) patients only had Diasorin measurements.
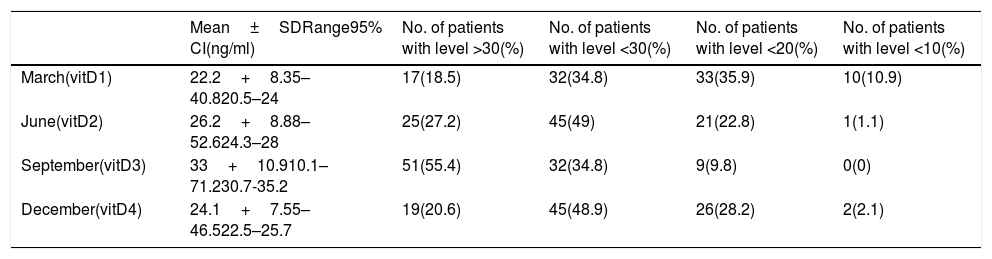
Seasonal variability of serum vitD levelsWe observed 87 patients (94.5%) with at least one determination <30ng/ml; 41 patients (44.5%) with at least one determination <20ng/ml; nine patients (9.7%) with at least one determination <10ng/ml. Only five patients always had levels ≥30ng/ml. All comparisons between the pairs of seasonal values were statistically significant (see Table 2).
Serum vitamin D levels in children with asthma and/or rhinitis in the four seasons of a year.
| Mean±SDRange95% CI(ng/ml) | No. of patients with level >30(%) | No. of patients with level <30(%) | No. of patients with level <20(%) | No. of patients with level <10(%) | |
|---|---|---|---|---|---|
| March(vitD1) | 22.2+8.35–40.820.5–24 | 17(18.5) | 32(34.8) | 33(35.9) | 10(10.9) |
| June(vitD2) | 26.2+8.88–52.624.3–28 | 25(27.2) | 45(49) | 21(22.8) | 1(1.1) |
| September(vitD3) | 33+10.910.1–71.230.7-35.2 | 51(55.4) | 32(34.8) | 9(9.8) | 0(0) |
| December(vitD4) | 24.1+7.55–46.522.5–25.7 | 19(20.6) | 45(48.9) | 26(28.2) | 2(2.1) |
CI, confidence interval; vitD, vitamin D.
All comparisons between the pairs of seasonal values were statistically significant.
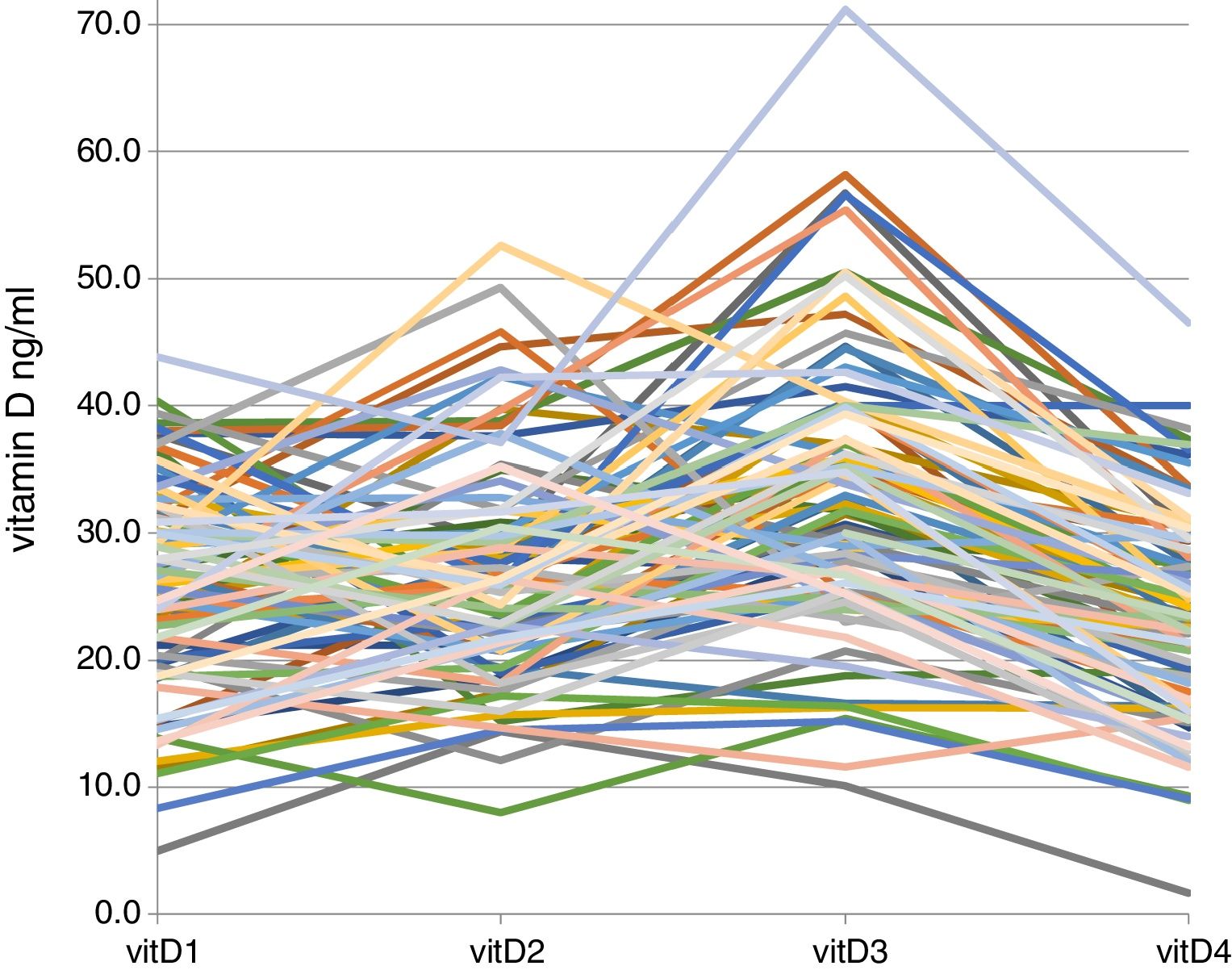
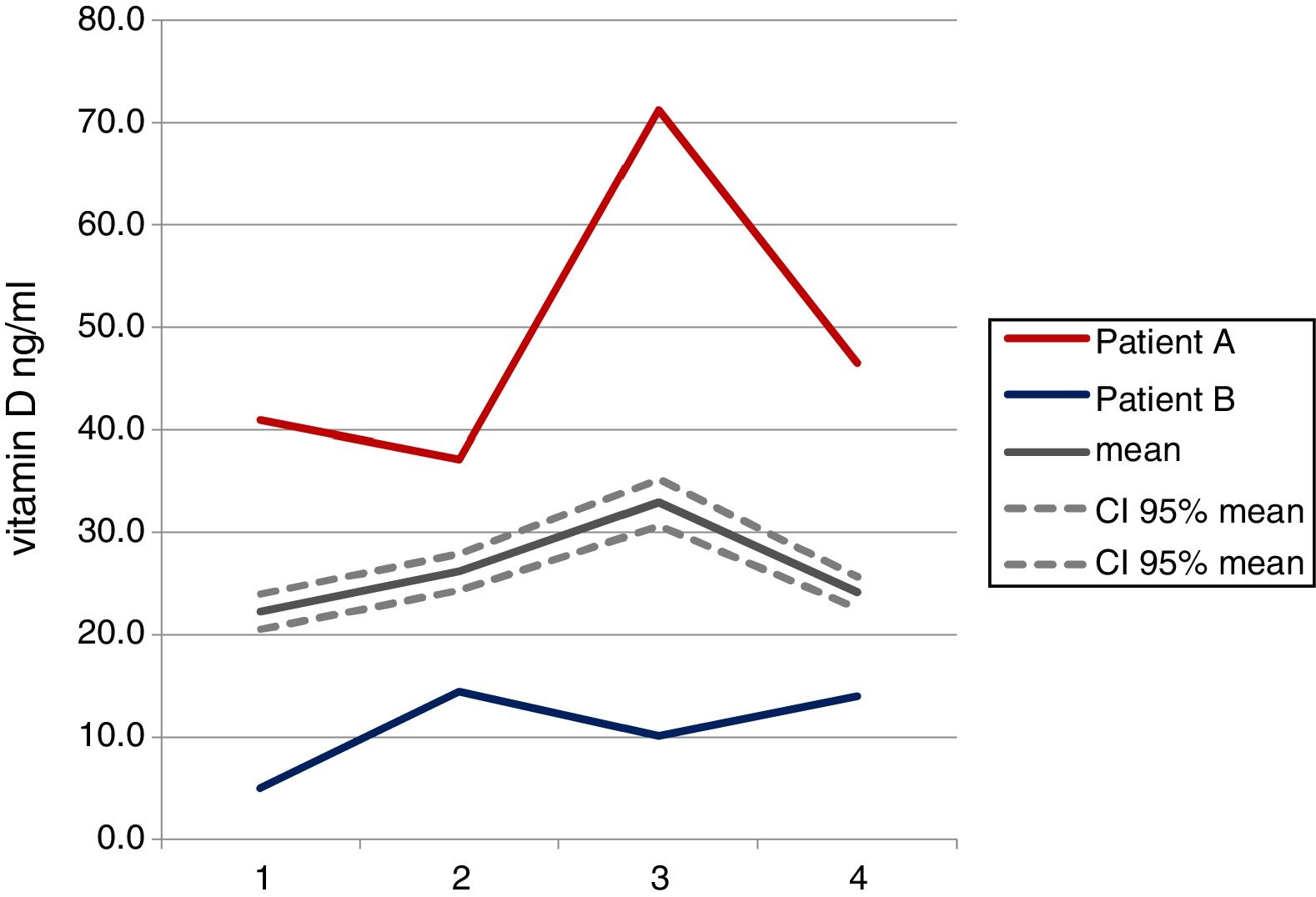
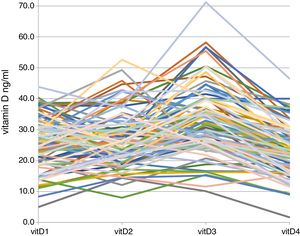
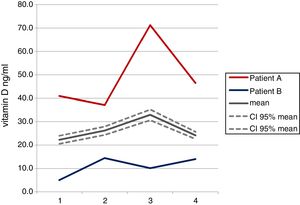
Fig. 1 shows the individual trends of serum vitD levels in the four determinations carried out in the 92 patients enrolled. A great variability is evident, which has been better exemplified in Fig. 2 where we represented the trends of two patients very different from each other, comparing them with the mean trend of all patients.
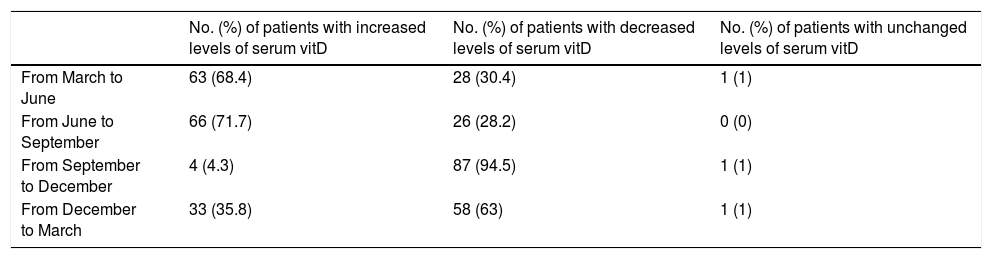
The variability of the individual seasonal trends is also proved by the data shown in Table 3: if it is true that in a given season the majority of patients follow a direction (increase or decrease of serum vitD levels), however, a substantial percentage behave differently and unpredictably. For example, at the end of spring (“from March to June”), 70% of patients showed increased serum vitD levels, but 30% showed a decrease.
Percentages of patients with serum vitamin D level increased, decreased or unchanged depending on the season.
| No. (%) of patients with increased levels of serum vitD | No. (%) of patients with decreased levels of serum vitD | No. (%) of patients with unchanged levels of serum vitD | |
|---|---|---|---|
| From March to June | 63 (68.4) | 28 (30.4) | 1 (1) |
| From June to September | 66 (71.7) | 26 (28.2) | 0 (0) |
| From September to December | 4 (4.3) | 87 (94.5) | 1 (1) |
| From December to March | 33 (35.8) | 58 (63) | 1 (1) |
vitD, vitamin D.
Five patients had values ≥50ng/ml in September and ≥30ng/ml throughout the year; 16 patients presented values ≥40ng/ml in September and always had ≥20ng/ml in the other months.
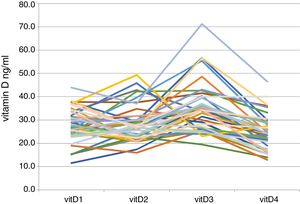
Survey on solar exposureThe parents of 50 (54.3%) of the 92 patients answered the survey. In particular, 40 out of 50 parents replied that the exposure of uncovered arms and legs was limited to the summer season (three months a year); three of them replied that, in addition to the summer exposure, their sons had an exposure twice a week in the remaining months (all for outdoor sports and all males); three parents answered only in summer for two months; three answered only in summer for a month; only one patient exposed himself more than three times a week throughout the year (and this was not associated with particularly high vitD values). Even among the 40 patients who probably had a similar summer sun exposure, the trends of serum vitD levels differed significantly, with a situation very similar to that observed in the entire population we studied (Fig. 3). The five patients who had a value ≥50ng/ml in September and showed serum vitD levels ≥30ng/ml throughout the year did not report a particularly high sun exposure in the survey, except in one case (patient A of Fig. 2). This latter case was a nine-year-old boy, suffering from persistent rhinitis, living in a seaside town; he told us he spent many hours a day on the beach, all summer long. His serum vitD levels were permanently and extensively >30ng/ml in all four determinations; in particular in September vitD was equal to 71.2ng/ml, which is the highest value we found in this our study.
Correlations between serum vitD levels and some parametersSerum vitD levels were significantly lower in patients with asthma (with or without rhinitis) than in patients with only rhinitis in September (p=0.04), with a trend towards statistical significance in December (p=0.06). Asthmatic patients with rhinitis and asthmatic patients without rhinitis showed a similar pattern of vitD values.
Males presented higher values than females in all periods (p<0.05), except in December where a trend towards statistical significance was observed (p=0.06).
A statistically significant correlation between the serum vitD levels and the circulating eosinophil count was observed only in December: as the vitD increased, circulating eosinophils increased (p=0.04). A correlation between total IgE and serum vitD levels has never been observed.
DiscussionThere are poor data about trends of serum vitD levels related to seasons in paediatric patients. We have prospectively evaluated them in the same group of patients over one year, with measurements performed in four periods (the end of the four seasons). Yu et al.16 also evaluated the seasonal trends of serum vitD levels, but did it retrospectively and with a single sample for each individual. The greatest value of their study lies in the huge sample size, as many as 95,137 subjects, all in adulthood (>19 years). Those authors predictably reported that vitD levels are higher in the summer months, peaking between August and September, and are lower in the winter months, particularly in February. Karaguzel et al.17 evaluated the seasonality of serum vitD levels in paediatric age, even if only concerning spring and autumn and not in the same individual. The authors measured, in a cross-sectional study, the vitD levels in 746 paediatric patients, finding that the prevalence of deficiency (<20ng/ml) was 93% during spring and 71% during autumn. Andersen et al.18 performed a one-year longitudinal observational study of 54 girls (11–13 years) and 52 women (70–75 years). The participants were examined three times (winter–summer–winter). Serum 25-hydroxyvitamin D concentration and vitD intake were measured at each visit. Sun exposure was measured during the summer. The authors reported that the usual sun habits were determinant (p=0.002) for change in vitD status from winter to summer. Batmaz et al.10 measured serum vitD levels every three months in 30 paediatric patients with asthma with house dust mite monosensitization. Those authors reported that asthma control measures, lung function test and IgE levels were significantly related to serum vitD levels, independently from age, body mass index, inhaled corticosteroid use, sun exposure and season.
We found, as other authors had previously done,10,16–18 that, on average, the serum vitD levels reach their maximum at the end of the summer and, conversely, the value recorded in December is significantly lower than the one detected in other periods. However, the most original and interesting finding of our study is the important difference in the individual trends of the serum vitD levels. The great variability of the aforementioned trends is evident from the observation of Fig. 1, where it is clear that for some individuals the vitD level increases from one period to another, for others it remains almost stationary and for others it decreases. We searched for a relationship only with exposure to sunlight, considered one of the most incisive factors, through the use of a survey. Most of the children (among the ones who answered the survey) were exposed to the sun especially during summer months. However, this does not explain the variability of the trends we observed, even among the 40 children who declared a similar exposure to sunlight. Of course, the survey we used was very simple and cannot be considered exhaustive for the purposes of a correct measurement of sun exposure. In addition, in fact, we did not look for relationships with the weather conditions which may have affected, in addition to clothing and hours spent outdoors, exposure to sunlight, or diet and income of parents, as Karaguzel et al.17 had done. However, despite the greater deepening, these authors did not find any relationship between the serum vitD levels they detected and all the aforesaid factors either.
Bolland et al.14 identified a value of at least 40–48ng/ml for men and 36–40ng/ml for women during the summer months as necessary to guarantee at least 20ng/ml throughout the year. Also in our population, five individuals had a value of ≥50ng/ml in September and showed serum vitD levels ≥30ng/ml throughout the year. According to the survey we gave to their parents, they were not more exposed to sunlight than others, except for patient A of Fig. 2. Still, observing the values of the month of September, we found that patients (16 patients in our study) who had values ≥40ng/ml always had ≥20ng/ml in the other months.
A clinical consequence of these considerations could be the practice of measuring serum vitD levels in candidates for drug supplementation (for example, asthmatic and/or rhinitic children) at the end of September, and to supplement those with serum vitD level <40ng/ml.
The finding, in our study, of higher mean values of vitD levels in males than in females had already been reported by Karaguzel et al.17 The authors hypothesized that the difference may be related to the number of hours spent outdoors for physical activity and dressing habits.
Finally, in our study we found lower mean values of vitD levels in asthmatic patients than in rhinitics. In this regard, Kim et al.19 conjectured that lifestyles (asthmatics, more than rhinitis, would shy away from activities to be carried out externally) and steroid therapies, particularly those taken orally, are determinant.
ConclusionsOur study demonstrated a wide and unpredictable variability of trends of serum vitD levels during the year in a group of paediatric patients with asthma and/or rhinitis, in the absence of pharmacological supplements. This should deter from approaching a pharmacological supplementation based on a single determination.
Conflict of interestThe authors have no conflict of interest to declare.
Author contributionsStefano Miceli Sopo conceived the design of the study and drafted the article. Giuseppe Cerchiara, Giulia Bersani, Serena Monaco, and Alberto Romano acquired the data. Andrea Poscia and Giuseppe Cerchiara analyzed the data and interpreted them. All authors revised the article and gave final approval of the version to be published.