Food protein-induced enterocolitis syndrome (FPIES) is a non IgE-mediated gastrointestinal food allergic disorder. Some diagnostic criteria have been published for acute FPIES. Of course, they are not all the same, so the clinician must choose which ones to adopt for his/her clinical practice. We present here a brief review of these criteria and, through two clinical cases, show how the choice of one or the other can change the diagnostic destiny of a child with suspect FPIES.
Food protein-induced enterocolitis syndrome (FPIES) is a non IgE-mediated gastrointestinal food allergic disorder.1 Acute and chronic FPIES are described. Often, acute FPIES presents by 4–6 months of age, with profuse and repetitive vomiting, pallor and lethargy 2–4h after ingesting a newly introduced food protein.1 In “Food allergy: A practice parameter update-2014”,2 we can read: “The physician should use the patient's medical history, response to a trial of elimination of the suspected food, and oral food challenge (OFC) to establish a diagnosis of FPIES. However, when the history indicates that infants or children have experienced multiple episodes or hypotensive reactions to the same food, a diagnosis can be based on a convincing history and absence of symptoms when the causative food is eliminated from the diet”. For over forty years, and particularly over the past five years, researchers have tried to define the diagnostic criteria that could make history as convincing as possible, allowing the clinicians to avoid a diagnostic OFC. However, the various diagnostic criteria panels available, although similar, differ in some not irrelevant aspects and the choice of one or the other affects the definitive diagnosis. Using the stories of two cases of probable FPIES, we made a brief review of the published diagnostic criteria for acute FPIES and analyzed the different outcomes obtainable depending on the application of one or the other.
History n.1When Robert was nine months old, he ate about 50 grams of boiled cod and after 2h he repeatedly vomited for 3–4h. He did not present pallor, nor lethargy nor diarrhea. After finishing to vomit the child was back to normal. In the previous two months, he had eaten boiled cod in the same amount for 3–4 times, without presenting adverse reactions. After about a month he ate about 50 grams of boiled sole and after 2h he had repetitive vomiting, but no pallor, nor lethargy, nor diarrhea. At the age of 14 months, Robert ate twice very small amounts (5 grams) of canned tuna and clams with no adverse reactions. Three months later, the prick tests with cod commercial extract (Lofarma, Milan, Italy) and with raw and cooked cod and sole were negative.
History n.2At the age of eight months, Rebecca ate a soft-boiled egg yolk (boiled for five minutes) and then fell asleep. After about one hour her parents heard her crying: the baby had just vomited. Rebecca then vomited three times and had pallor, lethargy, and diarrhea. Her parents took her to hospital. The baby vomited a last time and started endovenous rehydration. Blood tests were performed, and documented neutrophilic leukocytosis (28,990/mm3, 65% neutrophils, 22% lymphocytes) and thrombocytosis (605,000/mm3), lowering the next day (white blood cells 10,470/mm3, platelets 531,000/mm3). After about 6h, Rebecca no longer vomited, and her general condition returned to normal. In the previous month, Rebecca had eaten smaller amounts of soft-boiled egg yolk at least three times without adverse reactions. In the following months, the girl ate small bits of omelette, as large as a half teaspoon twice, with no adverse reactions happening. After five months from the critical episode, prick tests with commercial extracts (Lofarma, Milan Italy) of egg white and egg yolk and raw egg were performed, and resulted negative.
Are Robert and Rebecca's histories convincing enough? Can we formulate a definitive diagnosis of FPIES without performing an OFC? It depends.
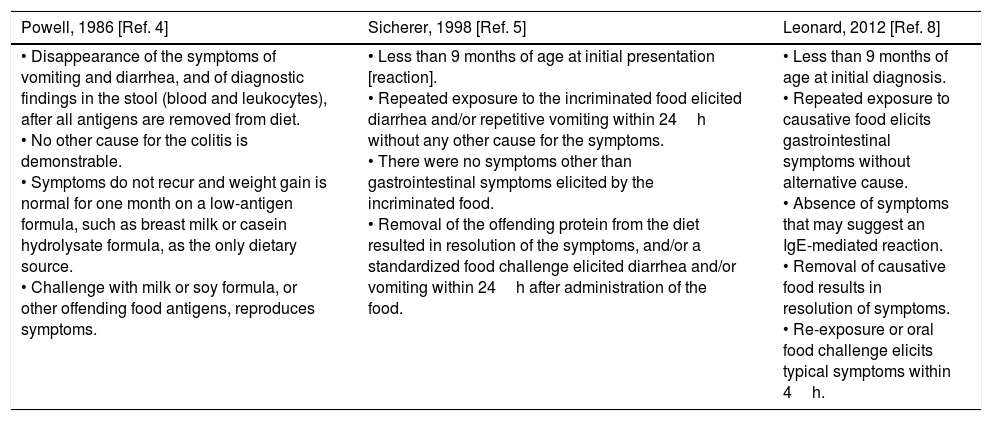
Geraldine Powell, first, defined criteria for the diagnosis of FPIES3: (1) onset of symptoms at less than two months of age; infant less than nine months at time of study; (2) while receiving the offending formula, the infant has watery stools with mucus, blood and leukocytes, and a peripheral polymorphonuclear leukocytosis; (3) diarrhea ceases and normal growth resumes when the offending antigen is eliminated; (4) the response to challenge meets the criteria described. A second version, slightly modified, was published in 19864 (Table 1). Powell, however, described children of few months of life, whose main feature was protracted diarrhea, her criteria best describe the chronic form of FPIES, now rarely seen. To August 30, 2017, by typing the word “FPIES” in Pubmed search string, 102 titles could be found. The oldest is Sicherer et al.’s study,5 dated 1998. Over the next 12 years only another 15 papers have been published, while from 2011 to today, in little more than 6 years, 87 papers, of which 62 correspond to the last three years, have been published. In short, interest in FPIES is relatively recent, perhaps for this reason Powell's criteria3 had poor circulation, while Sicherer et al.’s criteria5 have been adopted by many of the published studies until today.
Diagnostic criteria for FPIES published since 1978–2017.
| Powell, 1986 [Ref. 4] | Sicherer, 1998 [Ref. 5] | Leonard, 2012 [Ref. 8] |
|---|---|---|
| • Disappearance of the symptoms of vomiting and diarrhea, and of diagnostic findings in the stool (blood and leukocytes), after all antigens are removed from diet. • No other cause for the colitis is demonstrable. • Symptoms do not recur and weight gain is normal for one month on a low-antigen formula, such as breast milk or casein hydrolysate formula, as the only dietary source. • Challenge with milk or soy formula, or other offending food antigens, reproduces symptoms. | • Less than 9 months of age at initial presentation [reaction]. • Repeated exposure to the incriminated food elicited diarrhea and/or repetitive vomiting within 24h without any other cause for the symptoms. • There were no symptoms other than gastrointestinal symptoms elicited by the incriminated food. • Removal of the offending protein from the diet resulted in resolution of the symptoms, and/or a standardized food challenge elicited diarrhea and/or vomiting within 24h after administration of the food. | • Less than 9 months of age at initial diagnosis. • Repeated exposure to causative food elicits gastrointestinal symptoms without alternative cause. • Absence of symptoms that may suggest an IgE-mediated reaction. • Removal of causative food results in resolution of symptoms. • Re-exposure or oral food challenge elicits typical symptoms within 4h. |
| Miceli Sopo, 2013 [Ref. 9] | Leonard, 2015 [Ref. 7] | Nowak-Węgrzyn, 2017 [Ref. 13] |
|---|---|---|
| • Less than 2 years of age at first presentation [frequent feature but not mandatory]. • Exposure to the incriminated food elicits repetitive and important vomiting, pallor, hyporeactivity and lethargy within 2–4h. • Diarrhea may be present, much less frequently and later. The symptoms last a few hours, usually fewer than 6h. • Absence of symptoms that may suggest an IgE-mediated reaction. • Avoidance of the offending protein from the diet results in resolution of symptoms. • Re-exposure or oral food challenge elicits typical symptoms within 2–4h. Two typical episodes are needed to deliver the definitive diagnosis. | Major criteria • Repetitive vomiting or diarrhea within 6h of food ingestion. • Absence of cutaneous and respiratory symptoms suggestive of an IgE-mediated allergy. • Removal of causative food results in resolution of symptoms. • Reexposure or a food challenge elicits the typical symptoms. Minor criteria • Hypotension. • Lethargy, pallor, or hypotonia. • Negative skin-prick test and undetectable specific IgE level. • Absence of fever or hypothermia [<36°C]. | Major criterion • Vomiting in the 1–4 hour period after ingestion of the suspect food and the absence of classic IgE-mediated allergic skin or respiratory symptoms. Minor criteria • A second [or more] episode of repetitive vomiting after eating the same suspect food. • Repetitive vomiting episode 1–4h after eating a different food. • Extreme lethargy with any suspected reaction. • Marked pallor with any suspected reaction. • Need for emergency room visit with any suspected reaction. • Need for intravenous fluid support with any suspected reaction. • Diarrhea in 24h [usually 5–10h]. • Hypotension. • Hypothermia. |
Furthermore, Powell's criteria3,4 have been presented in recent years in different versions, for some aspects substantially different versions, compared to the original draft.
For example, in 2014 Caubet et al.,6 describing their case series, reported that “The diagnosis of FPIES was based on Powell's clinical criteria: (1) exposure to the incriminated food elicits repetitive vomiting, diarrhea, or both within 4h without any other causes for the symptoms; (2) symptoms are limited to the gastrointestinal tract; (3) avoidance of the offending protein from the diet results in resolution of symptoms; and (4) a standardized OFC isolated or re-exposure elicits the typical symptoms”. Clearly, those adopted by Caubet et al.6 are not the criteria suggested by Geraldine Powell in 1986,4 we call them Powell-modified criteria. Repetitive vomiting is brought out, the latency of symptoms is shortened, the criterion about weight gain (important for chronic FPIES) is absent. The necessity of at least one relapse, by re-exposure or during of an OFC is instead maintained. In 2015, also Leonard et al.7 reported that “the most commonly used criteria for diagnosing FPIES [Powell's criteria]” are those described by Caubet et al.6
Leonard et al.8 in 2012 (Table 1) proposed criteria similar to Powell-modified ones. Here, age limit is present, in fact the first episode of FPIES must have occurred before the completion of nine months, as well as in Sicherer et al.’s criteria.5 Symptoms are not otherwise specified if not for their gastrointestinal origin and it is specified that there must be no symptoms that may suggest an IgE-mediated reaction. Also Leonard et al.’s criteria8 require at least two episodes, as well as Powell's criteria, both the original3,4 and the modified ones,6 and as Sicherer et al.’s criteria.5
In 2013, Miceli Sopo et al.9 proposed their criteria for the diagnosis of acute FPIES (Table 1), which were not very different from those described above, except in a few details, such as the one regarding the severity of episodes. According to Miceli Sopo et al.,9 repetitive vomiting is not enough to let the child avoid an OFC for diagnostic purposes: the child must exhibit pallor and lethargy, too. The importance of the presence of diarrhea is reduced, repetitive and projectile vomiting is the dominant symptom. The duration of symptoms is explicit: the acute episode of FPIES lasts a few hours, then the child regains his normal conditions, this is a characteristic feature of acute FPIES. As in previous criteria,3–6,8 at least two episodes are necessary to enable the physician to formulate a definitive diagnosis of FPIES without applying to an OFC. The minimum age of the first episode is increased to two years (instead of nine months as in previous criteria), and the importance of this criterion is reduced, in accordance to later onset of FPIES from solid foods: the onset of FPIES is related to time of ingestion of guilty food and can also occur in adulthood.10–12
In line with this consideration, the age limit was eliminated in the diagnostic criteria for acute FPIES that Leonard et al.7 proposed and published in 2015 (Table 1). For the first time, a subdivision of the criteria into major and minor is presented. Major criteria, apart from age limit, are similar to those proposed by Leonard et al. in 2012,8 which in turn were similar to Powell-modified ones.6 The presence of isolated diarrhea without vomiting is accepted as possible; the latency of symptoms is lengthened up to 6h from the ingestion of guilty food; the need for at least two episodes remains unchanged. In the major criteria there is no mention of the severity of the episodes, but this aspect is addressed in the minor criteria where the possibility to have pallor, lethargy, hypotension, hypothermia is contemplated. But it is not clear how we should take into account the division between major and minor criteria.
This is instead fully solved in the last published diagnostic criteria, which are the result of an international consensus. Nowak-Węgrzyn et al.13 identify only one major criterion, vomiting after 1–4h from the ingestion of the culprit food (together with the absence of symptoms that may suggest an IgE-mediated reaction), and nine minor criteria (Table 1). According to the authors, the diagnosis of FPIES requires that a patient meets the major criterion and at least three minor criteria. In addition, aside from criteria, in a note, it is specified that “If only a single episode has occurred, a diagnostic oral food challenge should be strongly considered to confirm the diagnosis, especially since viral gastroenteritis is so common in this age group. Further, while not a criterion for diagnosis, it is important to recognize that acute FPIES reactions will typically completely resolve over a matter of hours, compared to the usual several day time course of gastroenteritis. The patient should be asymptomatic and growing normally when the offending food is eliminated from the diet.”
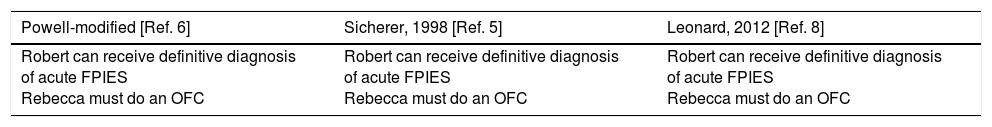
Can Robert and Rebecca receive diagnosis of acute FPIES without OFC? It depends. Robert and Rebecca's destiny changes depending on the diagnostic criteria we choose (Table 2). We replaced the original Powell's criteria3,4 with those modified5 because the first are not well applicable to acute FPIES and the second were the most applied for many years. Three are the possible outcomes for the two children, the most represented is the one identified by Powell-modified,6 Sicherer's,5 Leonard-2012's8 and Leonard-2015's criteria.7
Diagnosing acute FPIES to Robert and Rebecca according to the various published diagnostic criteria.
| Powell-modified [Ref. 6] | Sicherer, 1998 [Ref. 5] | Leonard, 2012 [Ref. 8] |
|---|---|---|
| Robert can receive definitive diagnosis of acute FPIES Rebecca must do an OFC | Robert can receive definitive diagnosis of acute FPIES Rebecca must do an OFC | Robert can receive definitive diagnosis of acute FPIES Rebecca must do an OFC |
Robert presented two episodes of repetitive vomiting in the last two occasions he ate the fish. This is sufficient to fulfill Powell-modified,6 Sicherer's,5 Leonard-2012's8 and Leonard-2015's criteria.7 It does not fulfill Miceli Sopo's criteria,9 because they require pallor and lethargy, neither Nowak-Węgrzyn et al.’s ones,13 because it meets only the first of the minor criteria.
On the contrary Rebecca, in addition to Nowak-Węgrzyn et al.’s13 major criterion, also presents the minor criteria n. 5, 6 and 7: Rebecca only according to these criteria can receive a definitive diagnosis of acute FPIES without making an OFC. Instead, for all the others,5–9 which require at least two typical episodes, Rebecca's history is not sufficiently convincing, and she must perform an OFC.
Both Robert Rebecca ate the suspected food both before and after the adverse reactions. It is unanimously admitted that acute FPIES may arise after a limited number of harmless ingestions. As regards the subsequent ingestions, they were very small quantitatively. We do not think that the harmless ingestions, both earlier and later than the adverse reactions, can influence the diagnosis for Robert and Rebecca. However, it is true that this aspect is not clear in all the diagnostic criteria for acute FPIES available today.
How did it end up for Robert and Rebecca? Consistent with the diagnostic criteria we defined ourselves,9 both Robert and Rebecca were submitted to an OFC with the suspected food and passed it. Robert did it at the age of 20 months (11 months after the last adverse reaction), and Rebecca at the age of 14 months (six months after her only adverse reaction). Did the two children pass the OFC because they had already acquired tolerance to the culprit food? It is possible, but unlikely. Tolerance in cases of acute FPIES from egg and fish is achieved in the majority of cases after the age of five years.14–17 Of course, the fact that Robert and Rebecca passed the OFC does not mean that Miceli Sopo et al.’s criteria9 are the most valuable. Instead, the most relevant aspect of these considerations is that Robert and Rebecca would have had a different destiny depending on which of the various diagnostic criteria we had chosen to adopt.
So what to choose in the future? The last proposed criteria, those by Nowak-Węgrzyn et al.,13 have certainly the advantage of having been chosen by a collective evaluation of experts on this argument, and of being more innovative. If we closely followed them, without considering the notes added beyond, the risk would be to formulate, in a formally unexceptionable way, diagnosis of acute FPIES even for patients with moderate to severe acute gastroenteritis which require access to emergency room and intravenous hydration. On the other hand, if we chose the more conservative criteria, as those of Miceli Sopo et al.,9 the risk would be to submit many children to OFCs, before assigning them a definitive diagnosis of acute FPIES. However, the choice to make an OFC in suspected acute FPIES could be more easily approachable nowadays, because we have a probably effective and safe drug therapy, the parenterally administered ondansetron.18
We have no solid reasons for choosing one particular diagnostic criteria panel for acute FPIES among those just examined, none of them has been validated. They were created basing on personal experience and retrospective case series. Ideally, it would be necessary to perform a study in which all children strongly or mildly suspected to have an acute FPIES were submitted to OFC. So it would be necessary to preliminarily define the minimum suspicious criteria for acute FPIES, that we do not have yet. A similar study would not be easy to rate. In fact, many allergists would not be easily available to propose OFC to children for whom they would definitely make diagnosis of acute FPIES only basing on history.
However, a choice has to be made, although not validated. We believe that international consensus criteria13 are the ones to choose, but absolutely considering also the suggestions contained in the notes. i.e., that there must be at least two episodes and that the duration of symptoms must be measured in hours, not in days. Moreover, it would be better if the episodes were at least of moderate severity, and if, together with repetitive vomiting, pallor and lethargy were present too.
Finally, we must be ready to change our mind, because of knowledge advances and, for example, in the future the absence of classic IgE-mediated allergic skin symptoms19 may not be included anymore among the criteria for the diagnosis of acute FPIES.
Ethic statementWe declared that the authorship of the paper “DIAGNOSTIC CRITERIA FOR ACUTE FOOD PROTEIN-INDUCED ENTEROCOLITIS SYNDROME. IS THE WORK IN PROGRESS?” is limited to those who have made a significant contribution to the conception, design, execution, or interpretation of the reported study.
We ensure that we wrote entirely original works, and if we used the work and/or words of others, this has been appropriately cited or quoted.
We declare that the work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
All authors approved the final version.
We declare we did not undergo studies on patients. We simply reported what happened during normal clinical activity without carrying out experimental studies.
Author contributionsSMS and GB designed the study and wrote the manuscript. CF and AR contributed to data collection. SMS and SM performed the interpretation of the results. All authors read and approved the final manuscript.
Conflict of interestAll authors have no conflicts of interest to declare.