Can the distribution of fast food outlets be obtained and effectively used to identify if there is a relationship between the placement of these and the prevalence and severity of asthma, rhinoconjunctivitis and eczema (ARE) in children and adolescents?
MethodFast food restaurant location data was obtained for seven countries. Data from the International Study of Asthma and Allergies in Childhood (ISAAC) was used from 53 centres in the same seven countries. Each ISAAC centre provided a detailed map of the study area. The location of restaurants and ISAAC centres were overlaid using the ArcMap software, and the number of restaurants within each ISAAC centre counted. Bivariate regression analysis was used to compare outlet density with ARE prevalence and severity.
ResultsThe results from the analyses showed a positive (non-significant) trend on a regression plot between outlet density and ARE severity.
This project has shown that it is practical to systematically obtain and map fast food outlets and compare their distribution worldwide with the prevalence and severity of diseases, in this case ARE. The devised methodology has proven to be an efficient way to obtain restaurant distribution data in a form that is manageable and suitable to compare with area based disease prevalences. This project has shown that a larger scale investigation is both feasible and warranted.
Fast food consumption and the symptom prevalences of asthma, rhinoconjunctivitis and eczema were found to be positively correlated in a cross-sectional survey by the International Study of Asthma and Allergies in Children. This showed significantly higher levels of severe forms of the three conditions with fast food intake ≥3 times per week, after adjustment. Additionally there has been research at biological level showing how fast food intake can hypersensitise the airway and immune system, giving possible explanations for the association. However, to date a causal relationship between fast food and asthma has not been determined.
What this study addsThis study has shown that it is feasible to determine fast food outlet distribution on an international scale using geodata software, and then correlate this data with asthma, rhinoconjunctivitis and eczema prevalence in school children. The methodology proposed gives a practical and effective means of investigating the effects of fast food on various outcomes in the form of an ecological study. In the future this can be used to help determine the impact of the rise in fast food availability on various health outcomes, such as the prevalence and severity of asthma, rhinoconjunctivitis and eczema.
Asthma, rhinoconjunctivitis and eczema (ARE) are a complex set of diseases whose exact causal mechanisms are yet to be uncovered. They are known to be multifactorial, with both a combination of genetic and environmental factors playing a role. A range of research pertaining to the link between some of the environmental factors involved has been carried out by the International Study of Asthma and Allergies in Children (ISAAC), particularly the effect of diet.1,2 Over the past 20 years the prevalence of these diseases has increased in many areas around the world, including New Zealand, which has one of the highest rates of asthma in the world.3 The recent increase in these diseases over the past two decades indicates that changes in environmental factors are likely to play a key role, perhaps more so than genetics. This is further supported by the vast variation in prevalence of the diseases between and within countries, suggesting that potentially avoidable causes may be present. Among these environmental factors, recent research has suggested that diet may be important in the development and severity of ARE, with certain foods such as fruit and vegetables playing a protective role, while others such as fast food acting as risk and/or exacerbating factors.2,5–21 The consumption of fast food is on the rise globally,2 and the significance of understanding the health implications of this increase in consumption is becoming increasingly critical for many chronic conditions. This study aimed to demonstrate a suitable methodology for investigating a possible correlation between fast food consumption and the prevalence and severity of ARE in school children, using distribution and density of fast food restaurants in the same centres that participated in the ISAAC studies (listed in Appendix A) as a surrogate measure for fast food consumption.
No large scale study using multiple fast food chains has been conducted comparing the distribution of fast food outlets and ARE prevalence. A study in 1998 using ISAAC data was conducted using McDonalds restaurants per 100,000 population in each country, as a surrogate measure for diet, and compared this to the prevalence of current wheeze in 13–14-year-old children, and found a significant correlation after accounting for Gross National Product as a confounder.20 Another study used ISAAC data and food frequency questionnaires and found that frequent consumption of hamburgers showed a dose-dependent association with asthma symptoms, and frequent takeaway consumption showed a similar association with bronchial hyper-responsiveness.16
A major epidemiological study investigating fast food and ARE was conducted using ISAAC Phase Three data and found that an increased risk of ARE in adolescents and children was correlated with high consumption of fast food (>3 times per week).2 Although the study showed promising results that a correlation between fast food and ARE (particularly severe asthma) exists, more work is required to establish a causal relationship. The current study has identified a new methodology to investigate this area.
Fast foods lack many of the nutrients found in fruits and vegetables and are high in omega-6 PUFAs (trans-fats), sodium, and added sugars.4 Hypotheses regarding the effect of the diet on asthma relate to both antioxidants and immunomodulatory mechanisms.7,10,14 The complex aetiology of allergic disease has led to a variety of theories regarding the impact of diet on ARE, such as fat and salt consumption leading to hypersensitisation of the airway.8,22 Links between consumption of fast food, or high intake of dietary components commonly found in fast food (such as trans-fats, saturated fat, sugar and salt) and symptoms of ARE have been shown by various studies.8,11,22–27 Symptoms of asthma have also been attributed to high sugar intake, particularly in children. A high sucrose diet has been thought to impair the pulmonary innate immune system and increase susceptibility to airway inflammation.24
Materials and methodsISAAC dataISAAC is a multicentre, multi-country, multiphase cross-sectional study, which effectively ‘mapped’ the prevalence of asthma, rhinoconjunctivitis and eczema in 237 centres across 98 countries.28 ISAAC Phase Three involved 1,187,496 6–7-year-old children and 13–14-year-old adolescents and was undertaken between 2001 and 2003. Schools were chosen randomly from defined geographical areas and each centre provided a detailed map of the study area to the ISAAC International Data Centre located in Auckland, New Zealand for archive. ISAAC Phase Three used standardised core written questionnaires as well as an optional environmental questionnaire, which asked questions about diet, height, weight, truck traffic, heating and cooking fuels, exercise, pets, farm animals, family size and birth order, birth weight, breastfeeding, socioeconomic status, paracetamol and antibiotic use, immigration status and tobacco smoke exposure. A non-verbal video with scenes of young people with clinical symptoms and signs of asthma was shown to the adolescent group. Written questionnaires on the symptom prevalence of asthma, rhinoconjunctivitis and eczema were completed by the adolescents at school and by the parents/guardians of children at their homes.
For this study, seven countries were used (Brazil, China, Italy, New Zealand, Portugal, Spain and the United Kingdom) to obtain information on fast food outlets. Data on the prevalence and severity of ARE from 53 ISAAC centres from these seven countries was used for the analyses.
Ethics approval was not required for this study, however in ISAAC Phase Three, where the disease data was obtained, each centre obtained ethics approval from their local Ethics Committee.
The following points are the detailed methods developed for this project for mapping the fast food outlets and ISAAC centres, written as instructions.
- 1.
Open ArcMap (this trial was conducted on version 10.2). To create a basemap, download the map file from http://www.naturalearthdata.com>downloads>Large scale data, 1:10m>Cultural>download countries. Extract entire contents of downloaded zip file into a separate folder.
- 2.
In ArcMap, click File>Add Data and locate and click on the .shp file previously extracted from the zip file. This will present as a world map within the ArcMap software.
- 3.
Obtain a list of the addresses of all restaurants of a particular restaurant chain in the country using the store location information from each restaurant's website.
- 4.
Reformat the information to include just the addresses, one line per address. All addresses must be formatted to a street number and street name, suburb name and city. Google maps can be used to verify street addresses of restaurants which are not in the correct format.
- 5.
Use http://batchgeo.com/ and copy over the address data from the Word document into the area as shown on home page of the website.
- 6.
Use the “Map Now” function and allow the addresses to be geocoded into a map. Any addresses that could not be found will be listed. These are likely not in the correct format and need to be adjusted in the spreadsheet above.
- 7.
Save and Continue once all address have been located. On the following page a map with all restaurants plotted will be shown. Scroll down and the option to download a KML version of the map will be available. Download the KML file and save it to a known location.
- 8.
From ArcMap, go to Geoprocessing>Arc Toolbox>Conversion Tools>From KML>KML to Layer. Choose the downloaded KML file with the restaurant address data as your input KML file, choose desired output location and data name. This will import the restaurant locations into ArcMap.
- 9.
Repeat steps 2–8 for each desired restaurant chain, and for each country. The countries included for this study are New Zealand, Spain, Italy, Brazil, China, Portugal and the United Kingdom.
- 10.
Import the .shp file for ISAAC centres into ArcMap. This will allow the restaurant location data and ISAAC centre areas to be overlayed, and the number of restaurants within each ISAAC centre can be generated onto a spreadsheet.
- 11.
Export the spreadsheet and using the COUNTIF function on Excel the number of outlets in each centre can be obtained.
- 12.
For each geographic centre divide the number of total outlets by the total population of 13–14 year olds×1000 to obtain number of outlets per 1000 children (outlet density).
Multiple linear regressions were performed to compare fast food outlet density to the percentage of children and adolescents with symptoms of current asthma, severe asthma, current rhinoconjunctivitis, severe rhinoconjunctivitis, current eczema, and severe eczema.
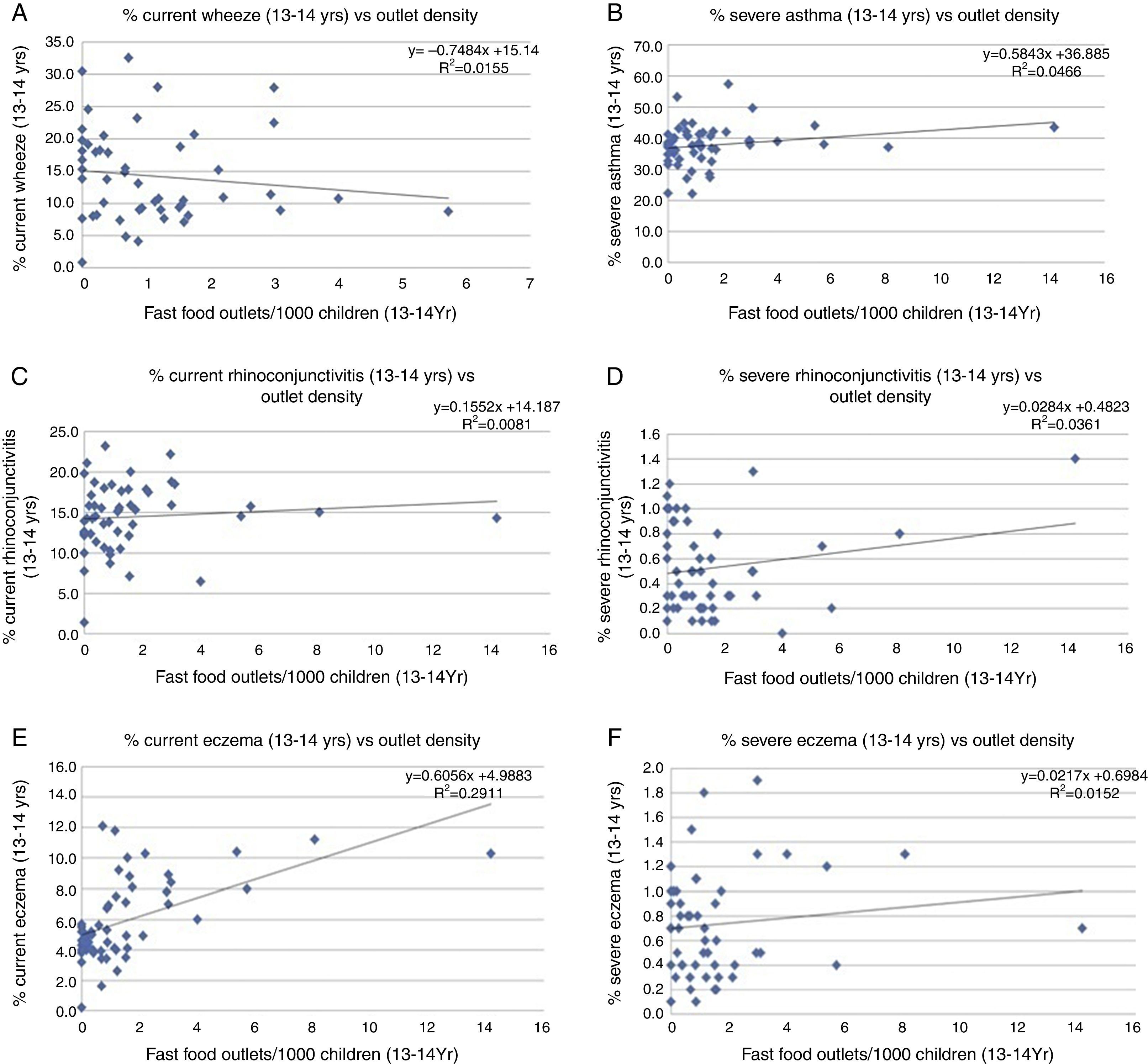
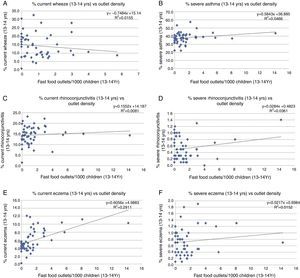
ResultsAs McDonald's and Burger King were the only two fast food restaurants which were in common across all seven countries that were surveyed, the study was restricted to the use of these two restaurant chains in the analysis. A number of centres were excluded from the analysis due to inaccurate population values either due to a reporting error or not all schools in the area being included in the sampling frame. The results from the analysis are summarised in Fig. 1(A–F).
The ‘Current’ category (A, C and E) for each of the three diseases included all adolescents who exhibited symptoms in the past 12 months of that particular disease. The ‘Severe’ category for asthma (B) used the percentage of Adolescents with wheeze in the past 12 months who also exhibited severe symptoms such as sleep disturbance, wheeze affecting speech, four or more acute attacks, exercise wheeze and night cough. ‘Severe’ rhinoconjunctivitis (D) was a combination of current nose symptoms, current nose symptoms and itchy-watery eyes and the answer “A lot” to having this nose problem interfere with daily activities. ‘Severe’ eczema (F) used a combination of those with current symptoms and those with sleep disturbance one or more nights per week.
All linear regressions showed a positive trend except for A, which showed a negative trend. The most significant of these was the relationship between current eczema and outlet density (E).
DiscussionThis project has shown that it is practical to systematically obtain and map fast food outlets and compare their distribution worldwide with the prevalence and severity of diseases, in this case ARE. However, none of the analyses showed statistical significance, which may be due to the small sample size, or may mean that a correlation does not actually exist.
The devised methodology has proven to be an efficient way to obtain and map large amounts of restaurant distribution data in a form that is manageable and suitable for additional analysis such as to compare with area-based disease prevalence. Thus the project has proven to be feasible and successful in indicating a larger scale investigation. A future study should include a systematic and documented process to obtain restaurant data for all possible countries included in ISAAC Phase Three, and perhaps a more thorough investigation of fast food outlets in each country, as the types of fast food available differ greatly from country to country. It may be valuable to compare an analysis using only common restaurants and an analysis using all available restaurants, and observing whether results differ. In this study, after exclusions were applied, 6 of the 53 centres (11%) had neither a McDonald's nor a Burger King restaurant within the region, and therefore had an outlet density of 0. These areas may well have had a number of local chains of similar fast food type restaurants which have not been accounted for in this study, which may bias the data. However, obtaining outlet distribution data for small, local chains would not only be time consuming and challenging, but may introduce a bias of its own if data for local chains were more easily obtainable for some areas rather than others. This study also only looked at ISAAC data for 13–14 year olds, as this was available for a higher proportion of the investigated centres, but a future study with a larger sample of centres should also utilise the ISAAC data for 6–7 year olds. It may also be of use to compare analyses between the two age groups as there are likely to be differences in the consumption of fast food between these two age groups.
In terms of validity, there are a number of measures that would need to be addressed in future studies to ensure minimisation of bias in the results. Correlations found in this study may in part be a result of lifestyle, other environmental cofactors, culture, or economy. Adjustment of potential confounders is an important part of the analysis and ISAAC has individual data of numerous covariates such as television watching, maternal smoking, maternal education, language, exercise and GNI. Ecological studies tend to be susceptible to confounding in general, and in this particular case, as we are dealing with the multifactorial diseases of asthma, rhinoconjunctivitis and eczema accounting for confounding is especially important. Other potential confounders to adjust for may include socioeconomic position and obesity (BMI). The nature of this study (the timescale for a summer studentship) did impose limitations on the ability to accurately gauge and adjust for confounders, particularly when dealing with differences within individual centres. ISAAC centres are geographical areas which vary vastly in size, ranging from small rural towns to large, diverse cities. For example, the Auckland region is accounted for as a single ISAAC centre, but has a wide range of difference within it for variables such as socioeconomic position, which makes accounting for some confounders challenging. For this methodology the confounders would need to be converted from individual-based measures to area-based means (or medians), which was not practical for this study given the timescale, but would definitely be achievable for a future study. In addition, the inclusion of more low and middle income countries would strengthen the results.
It is interesting to note that the only variable in this study which seemed to show a clearly observable positive association was between outlet density and current eczema, more so than for severe categories of any of the diseases. This is in contrast with the ISAAC study2 using individual data, which found greatest correlation with severity of ARE and the consumption of fast food, rather than prevalence, however the number of centres and numbers of participants in the ISAAC diet analysis was far greater than those used in this study and would have had more power to detect associations. The inference that fast food may worsen the severity of ARE in individuals with one of the diseases, rather than affecting the prevalence of said disease, is only supported for asthma in this study.
ConclusionAs the significance of all results is quite low and the sample size quite limited, all the above inferences are made with caution. The main aim of this project, for a summer studentship, was to determine the feasibility of the methodology of investigating fast food and ARE in this way, and this project has achieved that aim. With the growing fast food industry and increasing consumption of fast food in New Zealand and internationally, and with an increasing burden of non-communicable diseases, the significance of understanding the health implications of these changes is becoming increasingly relevant for healthcare both at a population health level and for individual care. The methods devised from this project for obtaining and analysing the distribution of fast food outlets may be useful in future for determining relationships between diet and disease. The methodology used is not necessarily restricted in scope to asthma, rhinoconjunctivitis and eczema as used in this project, and may be applied to a more expansive list of diseases potentially related to nutrition. Information from future studies using this methodology may be highly relevant to the health sector in terms of highlighting the need for a healthy diet, and providing reasons to decrease consumption of fast food, especially for those children and adults affected by chronic diseases.
FundingThe studentship was funded by the University of Auckland Faculty of Medical and Health Sciences, which had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestNone.
| Brazil | |
| Belo Horizonte | Assoc. Prof. Paulo Augusto M. Camargos |
| Brasília | Dr. Wellington G. Borges |
| Caruaru | Assis. Prof. Almerinda Silva |
| Feira de Santana | Assoc. Prof. Leda de Freitas Souza |
| Maceió | Prof. Francisco José Passos |
| Manaus Amazonas | Dr. Maria do Socorro Cardoso |
| Passo Fundo | Dr. Arnaldo Porto Neto |
| Porto Alegre | Dr. Gilberto B. Fischer |
| Recife | Dr. Murilo de Britto |
| Rural Santa Maria | Prof. Dirceu Soléa |
| Salvador | Assoc. Prof. Leda de Freitas Souza |
| Santa Maria | Prof. Dirceu Soléa |
| Santo Andre | Assoc. Prof. Neusa Wandalsen |
| São Paulo | Prof. Dirceu Soléa |
| Vitória da Conquista | Assoc. Prof. Leda de Freitas Souza |
| China | |
| Guangzhou | Prof. Nan-Shan Zhong |
| Tibet | Assis. Prof. Osamu Kunii |
| Italy | |
| Bari | Dr. Lucio Armenio |
| Emilia-Romagna | Dr. Claudia Galassi |
| Empoli | Dr. M.G. Petronio |
| Firenze | Dr. Elisabetta Chellini |
| Mantova | Dr. Gabriele Giannella |
| Milano | Dr. Luigi Bisanti |
| Palermo | Dr. Stefania La Grutta |
| Roma | Dr. Francesco Forastierea |
| Siena | Dr. Piersante Sestini |
| Torino | Dr. Giovannino Ciccone |
| Trento | Dr. Silvano Piffer |
| New Zealand | |
| Auckland | Prof. Innes Ashera |
| Bay of Plenty | Dr. Chris Moyes |
| Christchurch | Assoc. Prof. Philip Pattemore |
| Nelson | Dr. Richard MacKay |
| Wellington | Prof. Neil Pearce |
| Portugal | |
| Coimbra | Dr. M. Lourdes Chiera |
| Funchal | Dr. Rita Câmara |
| Portimao | Dr. Carlos Nunes |
| Porto | Dr. José M. Lopes dos Santos |
| Spain | |
| A Coruña | Dr. Angel López-Silvarrey Varela |
| Almeria | Dr. José Batlles Garrido |
| Asturias | Dr. Ignacio Carvajal Urueña |
| Barcelona | Dr. Rosa M. Busquets |
| Bilbao | Dr. Carlos González Díaz |
| Cartagena | Prof. Luis García-Marcosa |
| Castellón | Dr. Alberto Arnedo-Pena |
| Madrid | Dr. Gloria Garcia-Hernández |
| Pamplona | Prof. Francisco Guillén-Grima |
| San Sebastián | Prof. Eduardo G. Pérez-Yarza |
| Valencia | Prof. Maria M. Morales Suárez-Varela |
| Valladolid | Prof. Alfredo Blanco Quirós |
| United Kingdom | |
| North Thames | Prof. H. Ross Andersona |
| Scotland | Dr. Jane B. Austin |
| South Thames | Prof. H. Ross Andersona |
| Sunderland | Dr. Mohammad H. Shamssain |