Atopic dermatitis (AD) is one of the most common chronic inflammatory skin diseases during childhood and the prevalence is increasing worldwide.1 Although effective treatment options exist, absolute clinical improvement is unachievable: this might lead to search for alternative methods to cure disease especially by parents of children with AD. Fear of side effects of long term use of corticosteroids might also contribute to this attitude of parents. Limited data are available about alternative medicine (AM) use in AD during childhood.2 Our aim was to establish the prevalence and diversity of alternative medicines and to demonstrate risk factors associated with their use in children with AD.
Children aged 6 months to 18 years with at least three month-duration of AD admitted to the pediatric allergy outpatient department of Ankara Education and Research Hospital were enrolled in the study. The diagnosis of AD was based on United Kingdom (UK) Working Party's Diagnostic Criteria3 and severity was assessed by SCORAD index.4 We administered a questionnaire to parents designated to evaluate the varieties of AM used, the reasons for trying AM, who recommended AM, whether the child had any benefit or adverse event due to AM utilisation, impact of AD on quality of life of child and opinion about the control level of AD according to parents. The physicians also noted demographic characteristics and disease related features. The study was approved by the Ethics Committee of Ministry of Health, Ankara Education and Research Hospital and parents provided written informed consent.
All parents invited to study, agreed to participate. During February–August 2010, 68 patients [60.3% male, median 1.33 year (interquartile range; 0.79–5 years) were included. The median age at onset of AD symptoms was 9.5 (1.5–26.75) months. In the last year, the patients had been admitted for medical care with a median of three (2–4) times because of AD. The median of patients’ SCORAD index was 20 (16.1–28.8), and 23 (33.8%) of them had atopy. Thirty parents (44.1%) agreed with the proposal that “AD affects quality of life of my child” and 27 parents (39.7%) with “My child's AD is not under control”.
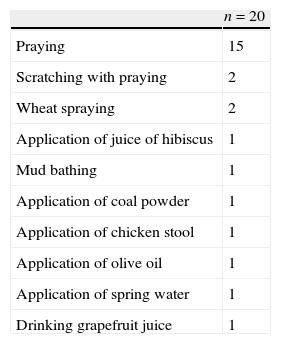
Alternative treatment recommendations were done mainly by relatives (26.5%) and friends (19.1%) to 33 parents and used by 20 (29.4%) patients. Praying was the most commonly tried alternative method (n=15). However, five patients used two or more types of AM for AD (Table 1). The other advised but not accomplished alternative treatment modalities were praying (n=8), application of barley juice (n=1), wrapping with wet bran (n=1), peeling of diseased skin (n=1) and cauterisation with hot metal (n=1). The most common reason cited by parents for application of AM was unresponsiveness to medical treatment (80%). Three children who utilised AM [praying (n=2), application of olive oil (n=1)] had a somewhat improvement as reported by their parents but two children had cutaneous infection after the application of chicken stool and juice of hibiscus. Logistic regression analysis revealed no relation between use of AM and gender, age, family history of AD, atopy, total number of admittance to health care due to AD, impact of AD on quality of life, parental educational background, SCORAD index, and serum IgE levels.
Types of alternative treatments used in patients with AD.
| n=20 | |
| Praying | 15 |
| Scratching with praying | 2 |
| Wheat spraying | 2 |
| Application of juice of hibiscus | 1 |
| Mud bathing | 1 |
| Application of coal powder | 1 |
| Application of chicken stool | 1 |
| Application of olive oil | 1 |
| Application of spring water | 1 |
| Drinking grapefruit juice | 1 |
Alternative treatment modalities change in different cultures and countries. Herbal medicine and homeopathy were the most commonly reported alternative treatments in UK for management of AD in children, whereas in our population, we found that praying was the most commonly used AM. The lack of satisfactory improvement by conventional medicine was the most decisive factor for AM use.2,5 Because of the chronic nature of the disease, prolonged treatment durations might compel parents to use alternative methods in AD. However, preference for AM was not associated with severity of disease, parental education level and impairment in quality of life due to AD. Also, the physicians should be aware of use of alternative methods in patients with a sudden worsening of AD.
Ethical disclosuresPatients’ data protectionConfidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentRight to privacy and informed consent. The authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
This study was presented at European Academy of Allergy and Clinical Immunology Congress in 2011 in Istanbul, Turkey and awarded as best poster presentation.