To the Editor:
Lyme disease is due to infection with a spirochete, Borrelia burgdoferi. It is transmitted from host to host by the Ixodes or deer tick. Approximately 20000 cases of Lyme disease are reported every year in the United States. Each of the three stages of the disease is associated with specific clinical features: early localised infection (with erythema migrans, fever, malaise, fatigue, headache and myalgias); early disseminated infection (days or weeks later, with neurological, musculoskeletal or cardiovascular symptoms, and multiple erythema migrans lesions); and late disseminated infection (with articular involvement)1. Lyme disease is mainly a clinical diagnosis and laboratory results may or may not support it. Antibiotic therapy is curative in most patients. The treatment of choice includes doxycycline or amoxicillin, cefuroxime axetil or erythromycin. However, severe or neurological disease with parenchymal involvement requires intravenous treatment with ceftriaxone or penicillin G1.
The authors present the case of a 60year old woman, with Lyme disease with neurological involvement in which first doxycicline treatment had failed. Third generation cephalosporins are currently the most effective treatment because of their very low minimum bactericidal concentration (MBC ≤ 0.4μg/mL for ceftriaxone) and have been shown to be effective in penicillin and tetracycline failures2. Alternative treatment with ceftriaxone 1g/day intravenous (iv) for thirty days was started.
On the 8th day, the patient referred itching which evolved into a rash on the palms, feet and neck, resolving spontaneously after the iv infusion was stopped. Treatment was re-started the day after and by the 16th day, she developed immediate pharyngeal, plantar and palmar pruritus, cutaneous rash, nausea and abdominal cramps with no other symptoms or signs. Emergency treatment for anaphylaxis was performed, with intramuscular epinephrine, systemic corticosteroids and antihistamines.
The patient was referred to our Allergy Division for study and management, as no alternative drug was appropriate at this point. According to the European Network for Drug Allergy (ENDA) group recommendations 3, cutaneous testing (prick and intradermal tests) were not reasonable as the patient was critically ill, and immediate treatment for neurological Lyme disease was mandatory.
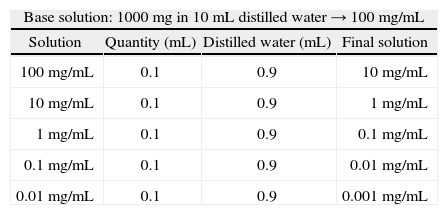
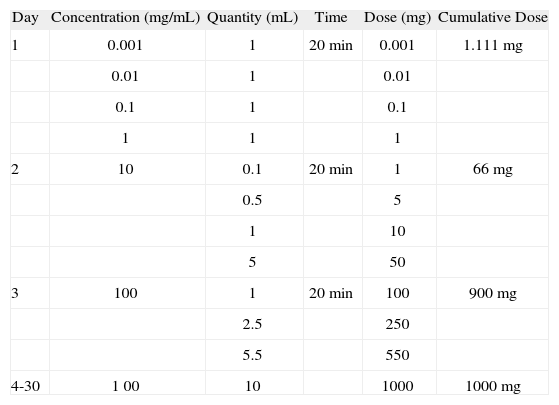
The patient began a desensitisation protocol to ceftriaxone starting with 0.001mg on the first day, with 10 fold increase every 20 minutes; 1mg as the first dose on the second, 100mg as the first dose on the third and 1000mg thereafter until the end of the treatment (Tables 1 and 2). The total dose (1g/ day) was achieved on the third day of treatment, after an eleven step protocol, without any adverse reactions.
The study of hypersensitivity drug reactions is based on a thorough clinical history, skin testing, in some cases (i.e. β-lactams) determination of drug specific IgE and provocation tests. According to the publication of Brockow et al.3, cutaneous testing should not be performed in the acute phase of reaction, due to its inherent risks, and an interval of at least 4weeks should be respected until cutaneous testing is performed.
When available, drug specific IgE should be determined, since it is of great value for diagnostic purposes in the work up of drug allergy. However, in our centre the only available specific IgEs are for amoxicillin, penicilloyl G, penicilloyl V, ampicillin and cefaclor (Phadia® catalogue), so, no specific IgE to ceftriaxone was determined in this patient, although it would have been of great importance.
Desensitisation for drug allergy is the induction of temporary clinical unresponsiveness to drug antigens. The main purpose of developing rapid desensitisation protocols for the treatment of drug hypersensitivity is to provide essential medications to patients avoiding severe reactions4. The administration of small doses of a drug until achieving the full therapeutic dose can be safely performed in allergic patients, allowing the treatment of severe diseases. These procedures should only be performed in the hospital setting and by fully trained medical personnel. There has been increasing interest in developing more rapid desensitisation protocols to antibiotics, mainly β-lactams, regarding its essential role in a wide number of infections, like syphilis in pregnant women.
There are several protocols for intravenous cephalosporin desensitisation, which range from hours to 14days. A typical protocol for desensitisation to intravenous penicillin or cephalosporins starts at 1/10000 to 1/100 target dose, doubling the dose every 15–20 minutes, until reaching the full therapeutical dose5.
Because this patient was seriously ill, it was decided to proceed with a drug desensitisation protocol with close observation and monitoring of the patient, starting with a very small initial dose (0.001mg) of ceftriaxone. The total dose (1g/ day) was achieved after 3days and effective treatment was completed until total recovery of the patient (30days).
Although more recent and rapid desensitisation protocols to cephalosporins are described in literature, the authors applied a 3-day protocol, because of the severity of the illness, and the patient could have more risks with a faster protocol.
No work up study was done to confirm the drug allergy diagnosis since the patient missed the scheduled appointment. However, the clinical history and the response to drug withdrawal clearly points to the diagnosis of drug allergy.