The present paper reviews the process by which the accreditation for the Paediatric Allergy specialty has been implemented in Europe according to the Section of Pediatrics Assembly of the European Academy of Allergy and Clinical Immunology. The itinerary by which the members of the Spanish Society of Pediatric Allergy and Clinical Immunology (SEICAP) have gained this accreditation and how it can be applied for in the future is also explained. Prospects for the future are also analysed.
In recent years, progress in scientific knowledge and the possibilities for improvement in biomedical technology have made it possible to advance in the diagnosis and treatment of allergological diseases in the paediatric population.
In this context, the diagnoses have been extended, the identification of allergenic proteins has improved, respiratory function can be evaluated, and inflammatory mediators can be measured in exhaled air, in small children. This in turn contributes to secure an improved and earlier diagnosis.
In addition, there have been parallel improvements in the therapeutic techniques, oral and sublingual immunotherapy, or in grouped and rapid treatment regimens. The perfecting of antigens, offering increased purity and better adjuvants, helps secure a better treatment response, making it possible to apply immunotherapy earlier and with increased safety.
The increase in food allergy in children, knowledge of the immunological mechanisms involved, and the identification of food allergy disorders not mediated by IgE – such as eosinophilic oesophagitis – have led to attempts to improve the quality of life of these children through the adoption of therapeutic measures such as the induction of tolerance or immunotherapy with foods such as cow's milk, egg or nuts. Such treatment approaches are increasingly widespread and offer excellent results.
The new drugs, such as anti-IgE monoclonal antibodies or anti-IL-5 agents and other products still in the investigational phase, open new management perspectives for allergic diseases.
This range of advances must be applied to a patient population different from the adult population. Children are not small adults but are individuals undergoing physical, mental and sexual growth and maturation, with a different metabolism and peculiarities pertaining to anamnesis, clinical examination, differential diagnosis, functional diagnosis and treatments that require adequate scientific preparation.
This defines the need for a specialty: Paediatric Allergology. The Spanish Association of Paediatrics (Asociación Española de Pediatría, AEP) refers to “Paediatrics and its specific areas”, as implicit recognition of the need for paediatric specialities in general. In addition, the AEP and its Steering Committee acknowledge and contemplate different paediatric specialities, including that represented by the Spanish Society of Pediatric Allergy and Clinical Immunology (Sociedad Española de Inmunología Clínica y Alergología Pediátrica, SEICAP). This Society is in clear expansion as regards its number of members, scientific activities, research projects, publications and ongoing training activities for members and interested paediatricians, as well as health education for families, teachers and children.
The recognition of this need on the part of the members of the SEICAP and its Steering Committee which have guided the Society in recent years has led to the implementation of a process for recognition of the specialty of Paediatric Allergology, based on a European accreditation process.
In relation to all the actions taken, due information has been provided, and support has been received, from the President of the National Paediatrics Commission of the Spanish Ministry of Health.
BackgroundSince the publication of Law 44/2003 of November 21, relating to the “Regulation of Healthcare Professions”, and which in its article 24 develops the Specific Capacitation Areas,1 the SEICAP started the organisation and design of a Specific Capacitation Area in Paediatric Allergology.
To this effect, and in accordance with the Spanish Society of Allergology and Clinical Immunology (Sociedad Española de Alergología e Inmunología Clínica, SEAIC), a series of work meetings were held with a view to reaching an agreement on the creation and accreditation of a Specific Capacitation Area in Paediatric Allergology, with a common training basis lasting two years. Resulting from the agreements reached, a joint document was signed and submitted to the President of the National Paediatrics Commission. This training agreement could not be materialised due to a number of reasons.
Knowing the training needs in Paediatric Allergology, and considering the scientific contents of training in Allergology as contemplated by the Spanish state medical residency training programme (Médico Interno Residente, MIR), Order 3.081/20052 and Spanish Royal Decree 183/2008 relating to Specialities in Health Sciences and specialised healthcare training,3 as well as the difficulties of establishing a programme for accreditation and training in Paediatric Allergology, the SEICAP has implemented the European Procedure for Accreditation in Pediatric Allergology – given the fact that Spain is fully integrated in the legal and scientific framework of the European Union.
European accreditation procedureIn May 2001, an adhesion contract was signed on the part of the European Academy of Allergology and Clinical Immunology (EAACI) and the European Society of Pediatric Allergology and Clinical Immunology (ESPACI). Article 6 of this agreement approves the specialty of Paediatric Allergology.
In 2003, the European Board of Paediatrics developed a document on the training programme, the European accreditation requirements, and the necessary training infrastructure for recognition of the specialty of Paediatric Allergology.4
In July 2005, the general lines were designed and approved for regulating the function of the Committee for Education and Training in Paediatric Allergology.
In 2006, the AEP submitted a Capacitation in Paediatric Allergology document to members of the SEICAP who met the training and experience requirements in Paediatric Allergology, and were members of the AEP. A total of 53 members of the SEICAP received this certification.
Contacts were established with the European Union of Medical Specialists (UEMS) through the paediatric section (Confederation of European Specialists in Pediatrics, CESP), and a series of criteria were developed for accreditation as European specialists in Paediatric Allergology (Annex 1).
In 2007, the Curricula and applications of the SEICAP members meeting the requirements were submitted, and the Certificate of European Pediatric Allergist was received from the European Training Committee in Pediatric Allergology (ETC-PA) by 95 members of the SEICAP.
Following the European accreditation process, the basic requirements to be met by the Teaching Units in charge of preparation of the future Paediatric Allergologists were drawn up.
Following development and approval by the Steering Committee of the SEICAP, which represents the scientific committee of the SEICAP, these requirements were submitted to and approved by the European Training Committee in Pediatric Allergology (Annex 2).
The requirements for Teaching Units in Paediatric Allergology were made known to the Paediatric Allergology Sections able to meet the established conditions. The requirements were forwarded to a total of 15 Sections and Units throughout Spain.
In 2008, the replies from 10 centres were received, and after analysing the applications, the Steering Committee of the SEICAP selected five centres which clearly met the established requirements:
- •
Section of Paediatric Allergology. Hospital General Universitario. Valencia
- •
Section of Paediatric Allergology. Hospital Sant Joan de Déu. Barcelona
- •
Section of Paediatric Allergology. Hospital La Fe. Valencia
- •
Section of Paediatric Allergology. Hospital Niño Jesús. Madrid
- •
Section of Paediatric Allergology. Consorci Hospitalari Park Taulí. Sabadell. Barcelona
In the case of the other five requesting centres, evaluation and approval was postponed for a second phase.
The European Training Committee in Pediatric Allergology (ETC-PA) in turn was contacted for approval of the five selected centres. The ETC-PA agreed to conduct the required audits of the selected Sections of Paediatric Allergology.
The Committee in charge of the audits was established, with the following members:
- •
The Secretary of the ETC-PA: José Lopes dos Santos. Oporto. Portugal
- •
A member of the ETC-PA: Antonella Muraro. Padua. Italy
- •
A Spanish representative of the RTC-PA: Alfredo Blanco-Quirós. Valladolid. Spain
- •
A representative of the SEICAP: Antonio Martorell. President of the SEICAP. Valencia. Spain
- •
Maria Anunciación Martín-Mateos, Training Member of the SEICAP. Barcelona. Spain
The audit applications have been completed by the Directors of the Hospitals to which the Sections of Paediatric Allergology requesting the accreditation belong.
The entire procedure to date has been forwarded to CESP, which will approve the audits, grant definitive accreditation of the Training Units, and approve the corresponding training programme. CESP likewise will ultimately be in charge of accrediting all the European specialists in Paediatric Allergology, and which to date have been recognized by the ETC-PA. The title awarded will be: “Certificate of European Paediatric Allergist”. The nature of the Certificate will be scientific and professional within the setting of the European Union.
The audits of the proposed Paediatric Allergology Sections were carried out on two dates: September 2008 in Barcelona and Sabadell, and November 2008 in Madrid and Valencia, according to the procedure regulated by the European Training Centre Visitation Programme for Tertiary Care Paediatric Specialities.5 In December 2008, the accrediting certificates of the following Paediatric Allergology Sections were awarded:
- •
Section of Paediatric Allergology. Hospital Universitario Sant Joan de Deu. Barcelona
- •
Section of Paediatric Allergology. Consorci Hospitalari Park Taulí. Sabadell
- •
Section of Paediatric Allergology. Hospital La Fe. Valencia
- •
Section of Paediatric Allergology. Hospital General Universitario. Valencia
- •
Section of Paediatric Allergology. Hospital Niño Jesús. Madrid
The Training Guide in Paediatric Allergology has been developed and approved, and is to be applied in the Training Units (Annex 3) within the context of the two-year training programme, including a final evaluative examination. Once this training programme has been completed, CESP will award the corresponding Certificate of European Paediatric Allergist. The definitive approval of this programme, a pioneering initiative in Europe, is currently pending, and will probably take place at the planned meeting in Warsaw (Poland) within the context of the Congress of the European Academy of Allergology and Clinical Immunology (EAACI) to be held in June 2009.
- 1.
Accreditation in Paediatric Allergology
- 2.
Basic requirements for European training centres in Paediatric Allergology
- 3.
Guide for the training of specialists in Paediatric Allergology
Paediatric Allergology has been recognised by CESP and UEMS as a Paediatric Subspecialty and its Training Syllabus has been approved. CESP is setting up a visitation programme to accredit Training Centres for paediatric subspecialties in EU countries, and in the future, European Paediatric Allergists will all be trained in such centres, according to the approved Training Syllabus.
However, there are many doctors currently practicing Paediatric Allergology in Europe, who have clinical experience and scientific activity in the field. Although their background and training may have been heterogeneous, they were really the pioneers of Paediatric Allergology, and many work in centres that will be accredited for training in this new subspecialty.
The Section on Paediatrics of EAACI (SP EAACI) considers, therefore, that interested European Paediatricians should have an opportunity, during a limited period of time, to submit their curricula and eventually be accredited as European Paediatric Allergists. This will be a provisional accreditation to be submitted to CESP later on.
Accreditation will be based on any of the following criteria:
- 1.
Doctors with double certification in both Paediatrics and Allergology.
- 2.
Paediatricians with the subspecialty, competence or equivalent differentiation in Paediatric Allergology recognised by professional, scientific or government departments, responsible for professional training and/or health care in their countries.
- 3.
Paediatricians considered by the Jury to have fulfilled the Training Syllabus for Paediatric Allergology.
- 4.
Paediatricians with at least 2 years training in a Paediatric Allergy Unit with recognised official capacity to train allergologists in that country.
- 5.
Paediatricians working in the field of Paediatric Allergology for at least 5 years, with a period of at least 2 years supervised by a certified allergist.
- 6.
Paediatricians with special interest in Allergology, who, for at least 10 years, significantly contributed to scientific progress in the field of Paediatric Allergology and the implementation of this subspecialty in their country, as judged by the Jury.
- 1.
This accreditation will be carried out during a temporary two-year period starting on 1st January 2005.
- 2.
Candidates must submit three copies of their Curriculum Vitae in English, to the secretary of the ETC-PA, or one copy in electronic format.
- 3.
The Jury will be constituted by:
- a.
The President of the SP EAACI
- b.
The Liaison Officer of the ETC-PA in CESP
- c.
Element of recognised reputation nominated by ETC-PA (this person may vary, and should preferably be the national delegate of the country of the candidate).
- a.
- 4.
The Jury may ask for confirmatory documents or for additional elements and may require an interview with the candidate.
- 5.
All candidates must pay a 50 Euro fee, to cover administrative costs and eventual travel costs or other expenses of the Jury. This should be paid to the treasurer of ETC-PA.
- 6.
All accredited candidates will receive a diploma.
This preliminary accreditation will form the basis of a first European list of Paediatric Allergists, to be submitted to CESP for final official approval. It is also a prerequisite for certification of Training Centres, since trainers must be certified specialists themselves.
Training Centres should have the necessary manpower, physical structure, equipment and clinical activity to provide training according to the objectives of the European Training Syllabus in Pediatric Allergology
Paediatric Hospitals, Paediatric Departments in General Hospitals, Allergy Units or Departments with significant Paediatric Allergology activity preferably in an autonomous unit.
Paediatric Allergy Department, Clinic or Unit
Capacity to treat patients with any allergic pathology: respiratory, digestive, dermatological, food-induced or drug-induced. Outpatient clinic with a minimum of 500 first attendances and 2000 subsequent attendances each year. Availability of up to five paediatric hospital beds for specific admission of allergy patients.
Capacity to perform clinical and if possible basic research, so that the trainees may be involved in scientific activity and publication. They should acquire and develop skills for critical evaluation of published studies.
The Training Centre may consist of more than one centre in close collaboration and should include at least two paediatricians certified in Paediatric Allergology.
Medical staff should have clinical, teaching, and research activity.
It is important to have nurses and other non-medical staff with expertise in allergy testing, pulmonary function and patient education, who might also participate in teaching and research activities.
Besides the general facilities assumed to be available in an average Hospital or Clinic, the Training Centre should provide:
- •
One consulting room for each doctor
- •
Facilities for allergy skin testing
- •
Facilities for allergy challenge testing (bronchial, oral, nasal conjunctival)
- •
Facilities for pulmonary function testing
- •
Facilities for allergen Immunotherapy
- •
Meeting Room for staff
- •
Access to specialised books and Journals
- •
General teaching and learning facilities, such as computers, Internet, data-show etc.
Training Centres should have available the specific equipment necessary for the comprehensive care of allergic children, therefore, fulfilling the learning aims included in the European Training Syllabus in Pediatric Allergology, including all relevant diagnostic and therapeutic methods.
- •
Basic paediatric office equipment (stethoscopes, otoscopes, scales, etc)
- •
Allergen extracts for the different kinds of tests
- •
Peak-flow meters
- •
Spirometer/s
- •
Facilities for bronchial provocation tests
- •
Spacers and face masks
- •
Placebo inhalatory devices
- •
Refrigerator(s)
- •
Facilities for exercise testing
- •
Rhinomanometer
- •
Tympanogram equipment (eg: Microtymp)
- •
Audiometry equipment (eg: audioscope)
- •
Plethysmograph
- •
Infant pulmonary testing equipment
- •
Exhaled Nitric Oxide measurement equipment
- •
Facilities for conjunctival provocation testing
Necessary equipment for cardio-pulmonary resuscitation and severe anaphylaxis treatment.
All relevant current laboratory studies to investigate allergic children should be available either in the Training Centre or in a directly cooperating clinical laboratory.
There may be some certified centres with conditions that are not strictly identical with the above described, but are reasonably comparable, as judged by the visiting task force. This may be the case, particularly during a transition period, when the first centres are accredited in a given country.
SEICAP December 2008
Prof. M.A. Martín-Mateos
Training and Teaching Member
- •
Accreditation in Paediatric Allergology
- •
Duration of training: two years
- •
Requirements:
- ○
Degree in Medicine
- ○
Specialist in Paediatrics or resident having completed the third year of training in Paediatrics
- ○
- •
Number of posts: 8–10 each year for all of Spain, distributed among the five accredited centres.
- •
Access:
- ○
Evaluation of the personal academic, scientific and professional curriculum
- ○
Evaluating examination involving a subject in the field of Paediatrics
- ○
A specific area in Paediatrics comprising the knowledge, diagnosis and treatment of disorders produced by immune mechanisms, based on the techniques inherent to the field, in podiatric patients (0–18 years of age).
The training period will span two years, and will have progressive contents with regard to the gaining of knowledge, operative capacity and responsibility, with the definition of three progressive levels:
- •
Level 1: Activities carried out by the clinical professionals of the teaching unit, and observed or assisted by the student.
- •
Level 2: Activities carried out by the student and supervised by the tutor or a specialist of the teaching unit.
- •
Level 3: Activities carried out directly by the student, without the need for direct tutoring. The student will carry out clinical activities, followed by due reporting of the work done.
- •
Knowledge of the immune system and of immunopathological processes, particularly referring to hypersensitivity.
- •
Knowledge of the clinical characteristics and exploratory techniques relating to allergic and immune processes, together with in vivo and in vitro exploratory methods.
- •
Knowledge of the bases and management of the therapies employed, together with allergic patient follow-up.
- •
Acquisition of skills and expertise in the application of diagnostic and therapeutic procedures relating to allergic diseases in children.
- 1.
T cell maturation in the thymus gland. T cell populations and subpopulations. B-T lymphocyte interaction. Characteristics of the T cells. Antigen recognition and presentation. T cell antigen receptor.
- 2.
Immunoglobulins. Structure and function. Control of IgE synthesis.
- 3.
Complement system.
- 4.
Adhesion molecules and cytokines in inflammation.
- 5.
Biology and function of eosinophils, mast cells and basophils.
- 6.
Physiopathology of allergic inflammation.
- 7.
Genetics of allergic diseases.
- 1.
Aerobiology and inhaled allergens. Panallergens. Allergenic extracts.
- 2.
Food allergens.
- 3.
Drugs as allergens.
- 4.
In vivo allergy study methods.
- 5.
Functional bronchial and nasal respiratory study. Inhaled allergen provocation techniques.
- 6.
In vitro diagnostic methods.
- 1.
Immune deficiencies. Immune complexes and allergic disease.
- 2.
Asthma. Natural history. Epidemiology. Pathogenesis of asthma. Diagnosis.
- 3.
Drug treatment for asthma.
- 4.
Exercise-induced asthma.
- 5.
Professional respiratory allergic diseases.
- 6.
Hypersensitivity pneumonitis.
- 7.
Allergic bronchopulmonary aspergillosis.
- 8.
Rhinitis: etiopathogenesis, classification, diagnosis and management. Sinusitis.
- 9.
Allergic conjunctivitis.
- 10.
Immunotherapy in allergic diseases.
- 11.
Management of allergic disease in the emergency setting and in surgery.
- 12.
Anaphylaxis and anaphylactoid reactions.
- 13.
Urticaria and angio-oedema.
- 14.
Mastocytosis.
- 15.
Atopic dermatitis.
- 16.
Contact dermatitis and professional dermatoses.
- 17.
Adverse reactions to foods. Allergic reactions.
- 18.
Drug allergy. Non-steroidal anti-inflammatory drug intolerance. Desensitisation protocols.
- 19.
Allergies to new agents: latex, Anisakis, etc.
- 20.
Prevention of allergic diseases.
- 1.
Skin tests: prick test, ID, rubbing test, patch, photopatch.
- 2.
Study of respiratory function: spirometry, forced spirometry, bronchodilation test, active anterior and/or acoustic rhinomanometry, plethysmography, impulse oscillometry.
- 3.
Provocation tests: conjunctival, nasal with/without rhinomanometry, non-specific bronchial testing: methacholine test, cold air test. Specific bronchial provocation tests: with allergens.
- 4.
Oral provocation tests: foods, additives.
- 5.
Food tolerance induction protocols: milk and egg.
- 6.
Study of drugs: skin tests, controlled administration, tolerance induction (hyposensitisation).
- 7.
Immunotherapy techniques and their clinical and immunological follow-up: conventional, co-seasonal, rapid, cluster.
- 8.
Inflammatory markers in asthma (induced sputum, nitric oxide determination, inflammatory mediators in exhaled air condensate).
- 9.
Blood gases.
- 10.
Rehabilitation techniques.
- 11.
Health training for the asthmatic patient and allergic patient.
- 1.
Total IgE quantification: CAP, RIA, ELISA, NF, INF.
- 2.
Specific IgE quantification: CAP, RIA, ELISA, immunoblotting, NF, microarrays.
- 3.
Antigen identification and characterization: immunoblot, Western-blot, RIA, ELISA, SDS-PAGE, PCR.
- 4.
Preparation of antigens: ultracentrifugation, chromatography, HPLC.
- 5.
Methods for the detection and quantification of other antibodies: ELISA, INF, immunoblot, immunodiffusion, radioisotopes, NF.
- 6.
Methods for the determination of cytokines and inflammatory markers: ELISA, RIA, IRMA, flow cytometry.
- 7.
Morphological and functional exploration of cells and molecules implicated in hypersensitivity mechanisms and immunopathology: flow cytometry, fluorescence microscopy, cell cultures, cryobiology, isotopic labelling of cells, polymerase chain reaction (PCR).
- 8.
Methods for the determination of immune complexes (Immunology laboratory).
- 9.
Methods for quantifying complement factors (Immunology laboratory).
- 10.
Methods for analysing complement function (Immunology laboratory).
- 11.
Aerobiology and environmental studies.
- 1.
Use of computer resources.
- 2.
Management and quality.
- 3.
Biomedical ethics.
- 4.
Evidence based medicine.
The teaching and research activities in all cases will be supervised by a specialist from the unit and/or the tutor.
- •
Addressing subjects of the training programme
- •
Once a week
- •
Clinical sessions:
- ○
Addressing cases of clinical interest or with diagnostic/treatment problems
- ○
Once a week
- ○
To be presented by the students undergoing training
- ○
- •
Once a week
- •
The presentations will be made by the students undergoing training and by the staff physicians
- •
At least once a year
- •
To be presented by the students undergoing training
- •
The presentations will be followed by discussion
All students undergoing training will participate in the following:
- •
Review and critical reading of published articles related to the speciality.
- •
Identification of problems that require study.
- •
Design and conduction of data collection, and evaluation of the results.
- •
Presentation at congresses and/or publication of the work done.
This experience is necessary in order to develop critical thinking and study habits that will serve to address diagnostic problems or control a healthcare protocol, as well as to assess the true usefulness of treatment innovations.
Both fourth-year residents in Paediatrics and first-year specialists in Paediatrics will dedicate the 11 months to specialised outpatient care, with the development of electronic case history protocols corresponding to the usual illnesses: childhood asthma, asthma in nursing infants, asthma in adolescents, atopic dermatitis, urticaria, food allergy, cow's milk protein allergy, drug allergies, and primary or acquired immunodeficiencies. They will orientate the diagnosis and propose treatment, and will conduct patient follow-up on the successive visits.
During these months, dedication will be from 8:00 a.m. to 15:00 p.m., from Monday to Friday.
During guided training, the students will rotate through the teaching unit staff members to become familiarised with the different ways of addressing problems and their solutions, and all activities will be supervised by the specialists of the teaching unit.
All the students undergoing training will follow the same program:
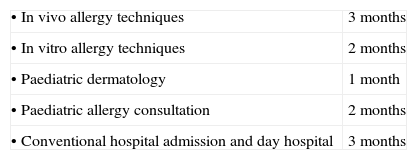
During the first three months the students will work in the in vivo tests laboratory, learning the following techniques:
- •
Exploration of respiratory function:
- ○
Basal spirometry
- ○
Non-specific bronchial provocation testing (stress, methacholine, histamine, cold air)
- ○
Specific bronchial provocation testing
- ○
Measurement of bronchial inflammation: NO, exhaled air condensate
- ○
Plethysmography
- ○
Impulse oscillometry
- ○
- •
Exploration of nasal function
- •
Drug provocation tests
- •
Food provocation/tolerance tests
- •
Skin tests
- •
Patch tests
- •
Immunotherapeutic techniques
During two months the students will work in the hospital laboratory to become familiarised with the diagnostic techniques in immunology and allergology related with the training programme.
- 1.
Continuous evaluation will be made, and at the end of each training module the unit team will evaluate whether the expected objectives have been reached in each student.
- 2.
A practical examination at the end of the training period is considered optional, but would be useful for the students and teaching unit members, who would be able to assess the quality of the training provided.
- 3.
There will be an obligatory final theoretical examination, comprising:
- a.
A multiple response test (100 questions).
- b.
Ten short response questions.
- c.
The resolving of a clinical case in which the student will be required to offer a diagnosis, request complementary tests, assess the results correctly, and propose treatment.
- a.
- 4.
During the training period, the students will prepare a research project, which will be evaluated and published before the training period is over.
- •
Master in Immunology and Pediatric Allergy. M.A. Martín-Mateos. University of Barcelona 1990–2008.
- •
Work group of the SEAIC-SEICAP. Training program for creation of the Specific Recruitment Area in Pediatric Allergology. 2003–2004.
- •
Training program in Allergology. Guide for the training of specialists. Ministry of Health. Ministry of Education and Culture. Edit. Rumagraf. 1996.
- •
European training center visitation program for tertiary care pediatric specialities. EAACI, 2004.