A recent survey in Batumi, Georgia showed a low prevalence of asthma in children (1.8%). A potential explanation is underdiagnosis of asthma. To investigate this, we conducted a follow up to the survey with the objective of estimating the level of childhood asthma underdiagnosis and to describe factors related to it.
MethodsSubjects included 437 survey participants who had a history of asthma-like symptoms and no diagnosis of asthma. All children underwent clinical examination (spirometry, skin prick tests, FeNO measurement) to identify new cases of asthma. The distribution of host and environmental factors was compared between the group with newly identified asthma and a group of 59 children with previously known asthma (diagnosed asthma).
ResultsClinical investigation identified 107 cases of undiagnosed asthma. The corrected asthma prevalence estimate was 5.1% (95%CI: 4.4%–5.9%) suggesting that 65% of asthma cases were undiagnosed. Compared to children with diagnosed asthma, children with undiagnosed asthma were younger (8.2±1.6 vs. 9.3±2.1; p=0.0005), had less frequent history of allergic disorders (38.3% vs. 64.4%; p=0.001), and a lower prevalence of parental asthma (1.8% vs. 8.4%; p=0.04). The groups did not differ in terms of environmental characteristics except for more exposure to passive smoking in the undiagnosed asthma group (p=0.01). Multivariate analysis confirmed results of simple analyses.
ConclusionIn Batumi, 65% of children with asthma remain undiagnosed. Older age of a child, coexisting allergic disorders, and parental asthma seem to facilitate diagnosis. Implementation of current diagnostic guidelines should improve diagnostic accuracy of pediatric asthma in Batumi.
International variation in the prevalence of childhood asthma is well documented by many epidemiological studies, mostly by the International Study of Asthma and Allergies in Childhood (ISAAC).1 The general finding is that even if the occurrence of asthma has substantially risen over recent decades its prevalence remains relatively low in countries of Eastern Europe.2 Evidence provided by epidemiological studies conducted since 2010 and based on the same protocol in Belarus, Estonia, Macedonia, and Ukraine shows that asthma is diagnosed in 1.5%–2.9% of school children and that there is some evidence that there may be underdiagnosis of asthma.3,4
Our recent population-based survey performed in 5351 urban and rural children in the Batumi region (Georgia) showed a low prevalence of pediatric asthma in urban children –1.8% (95%CI: 1.3%–2.3%).5 Moreover the findings revealed that a diagnosis of chronic bronchitis was known and reported by parents in 5.5% of the children, and a diagnosis of spastic bronchitis in 7.3% of the children. Similar low figures regarding the occurrence of pediatric asthma were found in other countries of Eastern Europe.6,7 A low prevalence of reported pediatric asthma suggested that some cases of pediatric asthma in the Batumi region remained undiagnosed. The goal of the study was to estimate the level of underdiagnosis of pediatric asthma in the urban population of children in Batumi and find out if children with a newly established diagnosis of asthma differ from children with previously established and known diagnosis of asthma, in terms of environmental and host factors pertinent to the epidemiological pattern of pediatric asthma.
MethodsStudy population and study designIn 2018 we published the results of a population-based respiratory health survey performed in children aged 6–16 years, residing in the Batumi Region, Georgia.5 The survey included 3239 urban and 2113 rural children. The present analysis was based on data from that study, obtained in urban children. Based on the survey results, two groups of children were identified: the group of children with diagnosed asthma and the group of children suspected for undiagnosed asthma. Urban children were selected due to practical considerations regarding access to clinical testing.
Definition of asthma status based on surveyDiagnosed asthma was defined as the parents’ report (questionnaire) of physician-diagnosed asthma in a child. Among the survey sample of 3239 urban children, 59 had diagnosed asthma. Undiagnosed asthma was defined as asthma found in children with reported (questionnaire) asthma-like symptoms but without diagnosis of asthma at the time of the questionnaire survey. A child was suspected to have undiagnosed asthma if the questionnaire included a positive answer to one or more of the following questions: “In the last 12 months has your child had a dry cough at night apart from a cough associated with a cold or chest infection?”; “Has this child had a cough that occurred with shortness of breath or rapid breathing?”; “Does this child usually have congestion in the chest or bring up phlegm or mucus apart from colds?”; “Has this child had wheezing or whistling in the chest in the last 12 months apart from symptoms associated with a cold or chest infection?”; “In the last 12 months has your child’s chest ever sounded wheezy during or after exercise/sports?”.
Clinical testing and physician diagnosis of asthmaIn total, 489 out of 3239 children had asthma-like symptoms and all were invited for clinical examination performed by one pediatrician certified in allergology and experienced in the field of children’s respiratory diseases including asthma, and familiar with GINA guidelines on the diagnosis of asthma. Some children did not complete the clinical examination due to migration or lack of parental consent. In total, 437 children (89.3%) underwent clinical examination. Detailed interviews showed no convincing symptoms of asthma in 87 children, thus leaving 350 children for further examination. Spirometry showed obstructive disorder in 178 children and 107 had a reversible airflow obstruction as shown by salbutamol trial. Measurement of FeNO was performed in 178 children with the following results: <20ppb in 18 children, 20–50ppb in 77 children, 51–100ppb in 50 children, and >100ppb in 33 children. All children examined for asthma underwent skin prick testing (Allergopharma – standard prick panel for Europe). Sensitization to at least one allergen was found in 105 children with the most frequent positive test being for Dermatophagoides farinae/Dermatophagoides pteronyssinus in 86 children. Asthma symptoms, sensitization to at least one allergen (skin prick test), and reversible airway obstruction were the principal criteria used to establish the diagnosis of asthma. The choice and application of the diagnostic methods depended on the physician’s decision and was not covered by the protocol of this study. The consulting physician was requested to answer the question of whether a child had asthma (yes/no).
Data analysisChildren with previously-known diagnosis of asthma (diagnosed asthma) were compared with children with newly-diagnosed asthma (undiagnosed asthma) in terms of anthropometric status, occurrence of allergic disorders, and environmental characteristics. Tables 1–3 show the names and distributions of variables used in analyses. Statistical analysis involved description of the distributions of quantitative and qualitative variables. Between-group differences in the distribution of quantitative variables were assessed by the Kruskal-Wallis test because of a non-normal distribution based on the results of the Shapiro-Wilk test. Between-group differences in the distribution of qualitative variables were assessed by the chi2 test. Inference regarding statistical significance was based on the criterion p<0.05.
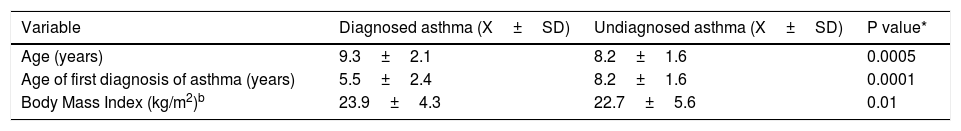
Personal characteristics of 59 children with diagnosed asthma and 107 children with undiagnosed asthma.
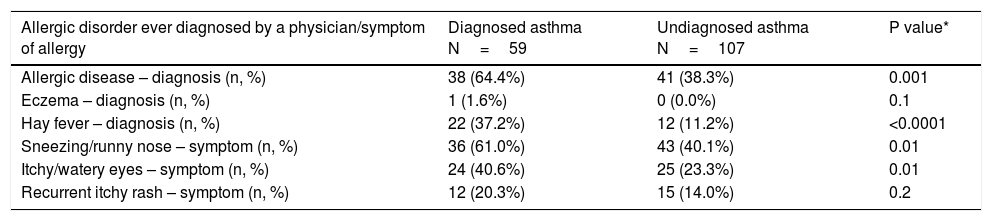
Allergic disorders diagnosed by physician in the past in 59 children with diagnosed asthma and 107 children with undiagnosed asthma.
| Allergic disorder ever diagnosed by a physician/symptom of allergy | Diagnosed asthma N=59 | Undiagnosed asthma N=107 | P value* |
|---|---|---|---|
| Allergic disease – diagnosis (n, %) | 38 (64.4%) | 41 (38.3%) | 0.001 |
| Eczema – diagnosis (n, %) | 1 (1.6%) | 0 (0.0%) | 0.1 |
| Hay fever – diagnosis (n, %) | 22 (37.2%) | 12 (11.2%) | <0.0001 |
| Sneezing/runny nose – symptom (n, %) | 36 (61.0%) | 43 (40.1%) | 0.01 |
| Itchy/watery eyes – symptom (n, %) | 24 (40.6%) | 25 (23.3%) | 0.01 |
| Recurrent itchy rash – symptom (n, %) | 12 (20.3%) | 15 (14.0%) | 0.2 |
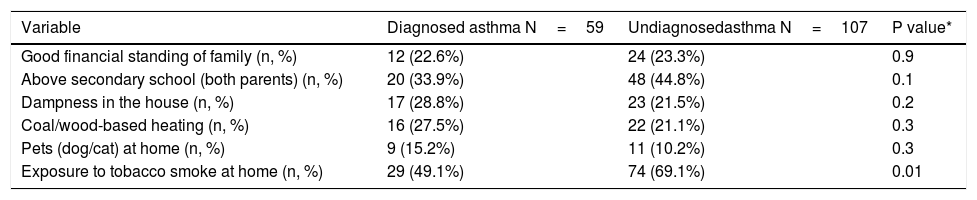
Social and environmental characteristics of 59 children with diagnosed asthma and 107 children with undiagnosed asthma.
| Variable | Diagnosed asthma N=59 | Undiagnosedasthma N=107 | P value* |
|---|---|---|---|
| Good financial standing of family (n, %) | 12 (22.6%) | 24 (23.3%) | 0.9 |
| Above secondary school (both parents) (n, %) | 20 (33.9%) | 48 (44.8%) | 0.1 |
| Dampness in the house (n, %) | 17 (28.8%) | 23 (21.5%) | 0.2 |
| Coal/wood-based heating (n, %) | 16 (27.5%) | 22 (21.1%) | 0.3 |
| Pets (dog/cat) at home (n, %) | 9 (15.2%) | 11 (10.2%) | 0.3 |
| Exposure to tobacco smoke at home (n, %) | 29 (49.1%) | 74 (69.1%) | 0.01 |
Results of simple analyses were verified by logistic regression analysis with diagnosed/undiagnosed asthma as the dependent variable. The complete model was parametrized using automatic backward selection of all candidate variables tested in simple analyses except for BMI (correlation with age: r=0.62; p<0.0001) and physician diagnosis of hay fever (association with physician diagnosis of any allergic disorder; p<0.0001). Statistical inference was based on the values of odds ratios (OR) and their 95% confidence intervals (95%CI) according to the criterion p<0.1. Underdiagnosis-corrected prevalence of pediatric asthma was estimated according to the formula: (number of diagnosed cases+number of undiagnosed cases)/number of children in the total study group (n=3239). The study protocol was approved by a local Ethics Committee at the Batumi Shota Rustaveli State University.
ResultsAs a result of the clinical examination, there were 107 new and previously unknown cases of asthma diagnosed among children. Based on the assumption that the true occurrence of asthma is reflected by the sum of diagnosed (n=59) and undiagnosed (n=107) asthma cases it could be estimated that in the examined population the likely prevalence of asthma in urban children is 5.1% (95%CI: 4.4%–5.9%). A comparison of that estimate with the estimate provided by the survey (1.8%; 95%CI: 1.3%–2.3%) suggests that only one third of children having asthma have been diagnosed with that disease, resulting in a 65% level of underdiagnosis of pediatric asthma.
Table 1 shows a comparison of age and body mass index between children with diagnosed and undiagnosed asthma. Children with diagnosed asthma were older, on average, than those with undiagnosed asthma. Likely resulting from this, all the differences in anthropometric measurements were statistically significant. However, the age of diagnosis among those with a previous diagnosis of asthma was statistically lower than the mean age at diagnosis of new cases of asthma (p=0.0001). The distribution of sex did not differ in a statistically significant way between the two groups (p=0.1): diagnosed asthma – 32.2% of boys; undiagnosed asthma – 44.8% of boys.
Compared to the group with diagnosed asthma, the group with undiagnosed asthma had less frequent diagnosis of chronic bronchitis made by physician in the past (40.6% vs. 24.3%, respectively; p=0.02), but did not differ in terms of past diagnosis of spastic bronchitis (44.0% vs. 44.8%, respectively; p=0.9). Moreover, the occurrence of the following physician diagnoses did not differ between two groups in a statistically significant way: pneumonia, sinusitis, tonsillitis, and ear infection.
Table 2 shows the occurrence of allergic disorders diagnosed by physician in the past and of symptoms of allergy reported by the parents. A statistically significantly smaller prevalence of a general diagnosis of allergic disease and hay fever as well as of nasal and eye symptoms was found in children with undiagnosed asthma than in those with diagnosed asthma. The occurrence of isolated cases of such disorders as diabetes, heart diseases, gastro-intestinal diseases and neurological disorders was similar in both groups.
Parents of children with undiagnosed, as compared with parents of children with diagnosed asthma had less frequent diagnosis of asthma (1.8% vs. 8.4%, respectively; p=0.04) and not of chronic bronchitis (7.5% vs. 8.4%, respectively; p=0.8). Both groups of parents did not differ in terms of questionnaire-derived diagnoses of any allergic disorder, eczema or hay fever.
Table 3 shows the occurrence of selected environmental characteristics of the two study groups. Compared with the group of children with diagnosed asthma, the group of children with undiagnosed asthma had more frequent exposure to tobacco smoke at home (p=0.01). In the latter group, the higher parental education, dampness in the house, coal/wood-based heating in the house and contact with pets were less frequent than in the group with diagnosed asthma, although the differences were not statistically significant (Table 3).
Results of multivariate analysis confirmed that for diagnosed asthma explanatory variables were older age (OR=1.48; 95%CI: 1.21–1.80; p=0.0001), any allergic disorder in a child diagnosed by physician (OR=3.02; 95%CI: 1.46–6.23; p=0.002), asthma in parents (OR=5.38; 95%CI: 0.86–33.69; p=0.07), and exposure to tobacco smoke at home (OR=0.44; 95%CI: 0.21-0.92; p=0.02). Presence of exposure to tobacco smoke at home was associated with an increased risk of undiagnosed asthma (OR=2.24; 95%PU: 1.08–4.64; p=0.02).
DiscussionThe results of our study suggest that the prevalence of pediatric asthma in Batumi, Georgia corrected for underdiagnosis is 5.1% (95%CI: 4.4%–5.9%). The figure of 5.1% is almost three times as large as the estimate of 1.8% (95%CI: 1.3%–2.3%) provided by our cross-sectional survey in the source population composed of urban children.5 The obtained difference can be translated to a 65% level of underdiagnosis of pediatric asthma in urban children of Batumi. A smaller difference reflecting a 50% underdiagnosis of pediatric asthma was found in Poland with other European studies showing a comparable prevalence of underdiagnosis of the disease, from 37% in a Danish study to 62% in a Dutch study.4,8,9 A high prevalence of undiagnosed asthma reaching 50% was also reported for primary care adult patients.10
In our earlier communication we hypothesized that some cases of undiagnosed asthma might be included in the diagnostic category of spastic bronchitis.5 Current findings do not seem to support such a view since a history of chronic bronchitis and not of spastic bronchitis was more frequent in children with diagnosed than in undiagnosed asthma. However, based on the current clinical evidence we would like to expand that view. In comparison with diagnosed asthma, children with undiagnosed asthma had less frequent history of allergic disorders and of parental asthma. In terms of environmental factors, the two groups compared did not differ in a statistically significant manner except for exposure to tobacco smoke at home, which was more frequent in the undiagnosed asthma group. The latter finding is difficult to explain, although it could convey the effect of social factors. In general, our findings seem to reflect the dominant role of host-related factors and seem to suggest that in pediatric practice in the area studied asthma is more readily diagnosed when respiratory and non-respiratory allergic symptoms are combined and are thus more convincing during diagnostic work-up. Published evidence shows that children with fewer respiratory symptoms, with less severe presentation, or without the usual allergic co-morbidities are more likely to be undiagnosed.11 In pediatric practice such a possibility cannot be neglected in light of the fact that current diagnostic guidelines are often not applied by general practitioners.12 We do not have data regarding insufficient application of pertinent diagnostic standards by pediatricians in Batumi but in our opinion it represents a real problem in primary health units.
Known non-medical factors associated with the underdiagnosis of pediatric asthma include low physical activity, high BMI, serious family problems, passive smoking, under-reporting of symptoms by parents, and poor socioeconomic status.9,13,14 Our study confirmed the association of passive smoking with underdiagnosis of asthma. However, we did not have access to data concerning the potential role of physical activity of children, family problems or socioeconomic status, except for a vaguely assessed financial standing. On the other hand, some of the described factors may have local/regional specificity due to cultural and social environments or their impact may be masked by their small between-subject variability in a study group. A study in Poland showed that among non-medical factors associated with the underdiagnosis of pediatric asthma, the age of a child plays a major role and other factors of importance include a large distance between residence and health center, and low parental attention at home.15 The meaning of age, also seen in our study, seems to reflect a flow of time in arriving at the convincing diagnosis in less overt cases, in the pediatric practice.
Our study has some limitations. The correction that we used to estimate asthma prevalence was based on the assumption that undiagnosed cases of asthma might be found among children with symptoms suggestive of an asthmatic disorder. We do not claim that we provided the perfect estimate, but it seems unlikely that undiagnosed cases frequently occur among children without chronic respiratory symptoms. Such a risk is more likely in pediatric health care than in questionnaire-driven standard interviews. Indeed, a substantial proportion, even two thirds of children with undiagnosed asthma, do not report their symptoms to a doctor.11 The design of our study did not include the examination of rural children. This is why our estimate of underdiagnosis of pediatric asthma is pertinent to the population of the city of Batumi. It cannot be generalized to a rural population even if our original survey showed 2.8% of asthma in rural children, compared to 1.8% of asthma in urban children.5 Another potential limitation of our study is related to the lack of clinical verification of the diagnostic accuracy of physician-diagnosed asthma, as reported by parents.
The strengths of our study stem from its design. Firstly, the source data set was large and distinct by a good participation rate of 91% in the urban area.5 Secondly, we used a standard questionnaire. Moreover, the selection procedure for clinical examination included children with a wide spectrum of asthma-like symptoms and resulted in a large group of children. It is also important that all children were examined by one pediatrician, who was an allergologist experienced in the field of respiratory diseases and used standard diagnostic criteria.
ConclusionIn Batumi, Georgia 65% of urban children with asthma remain undiagnosed. The prevalence of pediatric asthma in that population, corrected for underdiagnosis, is 5.1% (95%CI: 4.4%–5.9%) instead of the estimate of 1.8% (95%CI: 1.3%–2.3%) provided by the questionnaire survey. In our study, factors associated with the diagnostic accuracy of pediatric asthma include age, the presence of non-respiratory allergic disorders in children, parental history of asthma, and exposure to tobacco smoke at home. Older age of a child with suspected asthma, co-existing allergic disorders in a child and asthma in parents seem to facilitate the diagnostic process leading to the final diagnosis of pediatric asthma. Implementation of current diagnostic guidelines in pediatric practice should improve diagnostic accuracy and should substantially contribute to more appropriate management of pediatric asthma in Batumi.
FundingThis work was supported by University of Silesia in Katowice, Poland (intramural grant: KNW-1-132/K/8/O).
Conflict of interestThe authors have no conflict of interest to declare.