Allergen-specific immunotherapy (ASI) is the only effective treatment for allergic respiratory diseases which has the potential to change the natural course of the disease. In this present study we aimed to evaluate the paediatricians’ knowledge, perspectives and attitudes about ASI for allergic respiratory diseases.
Materials and methodsThe study was conducted between September 2014 – January 2015. A survey of 25 questions assessing paediatricians’ knowledge, perceptions and attitudes about ASI was developed by an expert panel and applied by physicians in hospitals in Izmir, Turkey, where the paediatricians work. Data were recorded in SPSS for Windows v.16. Descriptive statistics, chi square analysis was used. P<0.05 was considered as significant.
ResultsFully completed surveys from 180 paediatricians were analysed. The respondent paediatricians had an age of 37±8.2 years, and 56 of them were male. The majority of the respondents (n: 146) were working fewer than five years as a paediatric specialist. 93.9% of the paediatricians believed that ASI was effective for the treatment of allergic respiratory diseases. There was satisfactory knowledge of the characteristics, aims, effects and limits of ASI.
ConclusionASI is generally well-known and accepted among paediatricians. A better synergy between paediatricians and paediatric allergy specialists can provide more use of this treatment method for allergic respiratory diseases in childhood.
Allergic respiratory disease represents a significant and expanding health problem worldwide.1 During the past four decades, a dramatic increase in the prevalence of allergic disease has occurred, and respiratory allergic disease is now the most common chronic disease among children and adolescents.2,3 The increase is especially problematic in children because of the chronicity and the frequently aggravating nature of the disease.4 So early and correct diagnosis and an adequate therapeutic management of allergic respiratory diseases in children are strongly desirable.
Allergen specific immunotherapy (ASI) is the only effective treatment for respiratory allergy which has the potential to change the natural course of the disease.5 Its immunological mechanisms of action have been demonstrated as induction of allergen specific immune tolerance. Many clinical trials and meta-analyses have convincingly shown that ASI can achieve promising results for patients and the society, improving the quality of life, reducing the long term costs and burden of allergies.6 Despite this, ASI remains underused in patients with allergic rhinitis or asthma worldwide.7
Paediatricians are the first-line specialist who face the problems related to respiratory allergic disease in childhood. Based on these premises we performed a questionnaire-based survey among paediatricians in Izmir, Turkey to assess their knowledge, perception and attitude about the ASI.
Materials and methodsThe questionnaire was developed based on the current literature, guidelines, and expert opinions8-10 (Table 1). Responses to the questionnaire were received between September 2014 through January 2015 from paediatricians working in our and the other hospitals in the İzmir area. The questionnaire (Y/N, T/F or multiple-choice answers) consisted of 25 items evaluating the paediatricians’ characteristics (age, gender, practice setting and working time) and knowledge, perception and attitudes regarding ASI. The Clinical and Laboratory Research Ethics Committee (2014/38-13) and the Provincial Directorate of Health approved the study. The data was recorded in SPSS for Windows v.16 (SPSS, Inc., Chicago, IL, USA). The frequency (%) was used for descriptive data, Pearson x2 and Fisher Exact tests were used for comparisons between groups. P<0.05 was considered significant.
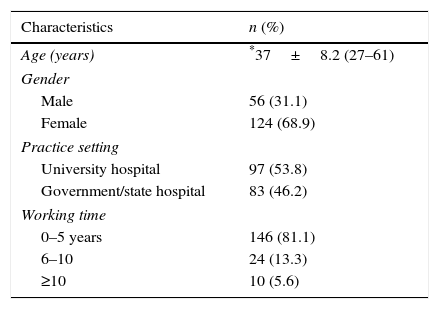
Demographic characteristics of the paediatricians who responded to the questionnaire (n=180).
| Characteristics | n (%) |
|---|---|
| Age (years) | *37±8.2 (27–61) |
| Gender | |
| Male | 56 (31.1) |
| Female | 124 (68.9) |
| Practice setting | |
| University hospital | 97 (53.8) |
| Government/state hospital | 83 (46.2) |
| Working time | |
| 0–5 years | 146 (81.1) |
| 6–10 | 24 (13.3) |
| ≥10 | 10 (5.6) |
Fully completed surveys from 180 paediatricians were analysed. The characteristics of the study group are summarised in Table 1. The respondent population had a mean age of 37±8.2 years (range 27–61), and 56 (31%) of them were male. 54% of the respondent paediatricians worked in the university hospital and 46% of them worked in the government/state hospital. The majority of respondents (n: 146) have worked fewer than five years as a paediatric specialist.
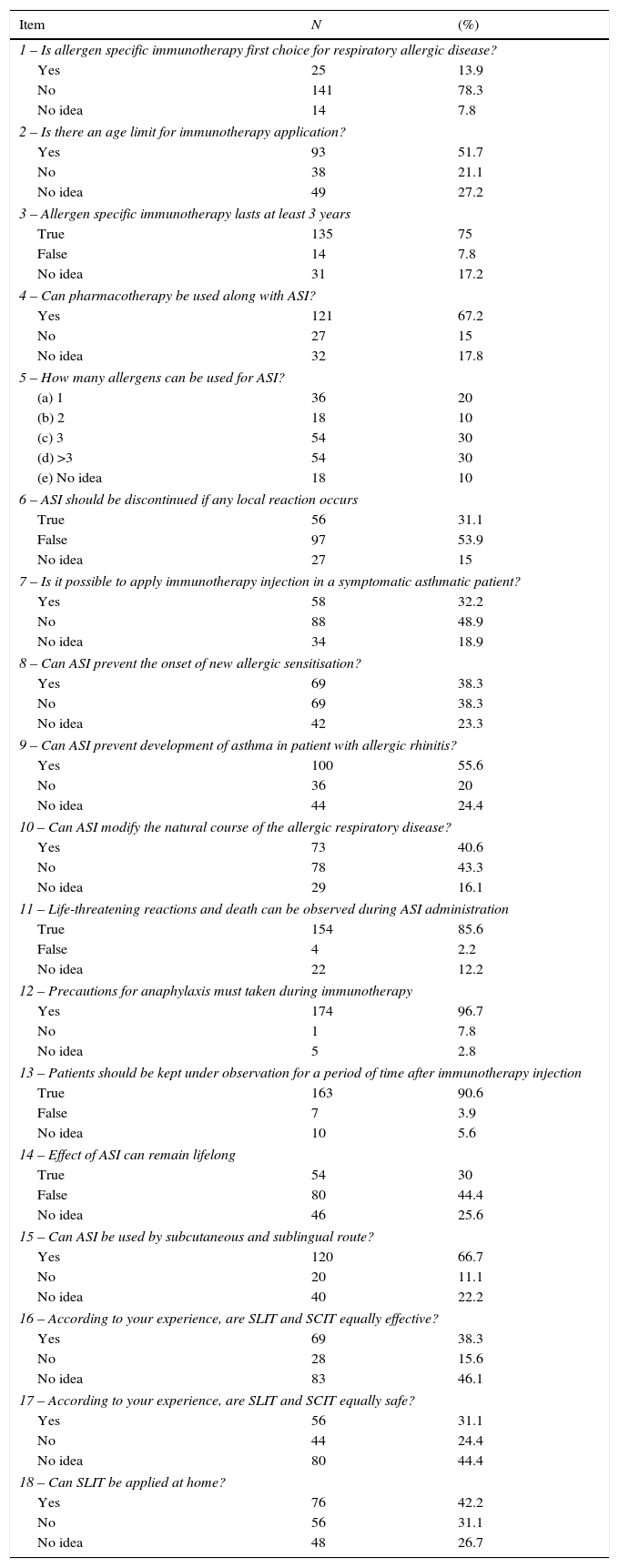
Knowledge and perception of paediatricians about allergen specific immunotherapy in İzmirResponses to several questions regarding ASI are presented in Table 2. According to the results, it seems that the general knowledge on ASI is overall satisfactory among paediatricians in İzmir and that they are well aware that ASI is recommended for allergic respiratory disease. The main differences between SCIT and SLIT, especially concerning the efficacy and safety aspects, are also known.
Number and percentages of the responses to the items asked for paediatrician's knowledge and perception about ASI in İzmir.
| Item | N | (%) |
|---|---|---|
| 1 – Is allergen specific immunotherapy first choice for respiratory allergic disease? | ||
| Yes | 25 | 13.9 |
| No | 141 | 78.3 |
| No idea | 14 | 7.8 |
| 2 – Is there an age limit for immunotherapy application? | ||
| Yes | 93 | 51.7 |
| No | 38 | 21.1 |
| No idea | 49 | 27.2 |
| 3 – Allergen specific immunotherapy lasts at least 3 years | ||
| True | 135 | 75 |
| False | 14 | 7.8 |
| No idea | 31 | 17.2 |
| 4 – Can pharmacotherapy be used along with ASI? | ||
| Yes | 121 | 67.2 |
| No | 27 | 15 |
| No idea | 32 | 17.8 |
| 5 – How many allergens can be used for ASI? | ||
| (a) 1 | 36 | 20 |
| (b) 2 | 18 | 10 |
| (c) 3 | 54 | 30 |
| (d) >3 | 54 | 30 |
| (e) No idea | 18 | 10 |
| 6 – ASI should be discontinued if any local reaction occurs | ||
| True | 56 | 31.1 |
| False | 97 | 53.9 |
| No idea | 27 | 15 |
| 7 – Is it possible to apply immunotherapy injection in a symptomatic asthmatic patient? | ||
| Yes | 58 | 32.2 |
| No | 88 | 48.9 |
| No idea | 34 | 18.9 |
| 8 – Can ASI prevent the onset of new allergic sensitisation? | ||
| Yes | 69 | 38.3 |
| No | 69 | 38.3 |
| No idea | 42 | 23.3 |
| 9 – Can ASI prevent development of asthma in patient with allergic rhinitis? | ||
| Yes | 100 | 55.6 |
| No | 36 | 20 |
| No idea | 44 | 24.4 |
| 10 – Can ASI modify the natural course of the allergic respiratory disease? | ||
| Yes | 73 | 40.6 |
| No | 78 | 43.3 |
| No idea | 29 | 16.1 |
| 11 – Life-threatening reactions and death can be observed during ASI administration | ||
| True | 154 | 85.6 |
| False | 4 | 2.2 |
| No idea | 22 | 12.2 |
| 12 – Precautions for anaphylaxis must taken during immunotherapy | ||
| Yes | 174 | 96.7 |
| No | 1 | 7.8 |
| No idea | 5 | 2.8 |
| 13 – Patients should be kept under observation for a period of time after immunotherapy injection | ||
| True | 163 | 90.6 |
| False | 7 | 3.9 |
| No idea | 10 | 5.6 |
| 14 – Effect of ASI can remain lifelong | ||
| True | 54 | 30 |
| False | 80 | 44.4 |
| No idea | 46 | 25.6 |
| 15 – Can ASI be used by subcutaneous and sublingual route? | ||
| Yes | 120 | 66.7 |
| No | 20 | 11.1 |
| No idea | 40 | 22.2 |
| 16 – According to your experience, are SLIT and SCIT equally effective? | ||
| Yes | 69 | 38.3 |
| No | 28 | 15.6 |
| No idea | 83 | 46.1 |
| 17 – According to your experience, are SLIT and SCIT equally safe? | ||
| Yes | 56 | 31.1 |
| No | 44 | 24.4 |
| No idea | 80 | 44.4 |
| 18 – Can SLIT be applied at home? | ||
| Yes | 76 | 42.2 |
| No | 56 | 31.1 |
| No idea | 48 | 26.7 |
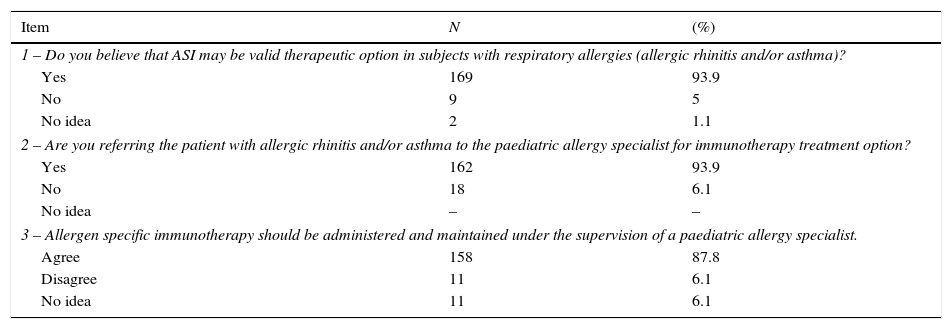
Responses to several questions about attitudes of paediatricians for ASI are presented in Table 3. The majority of respondent paediatricians (93.9%) believe that ASI is a valid therapeutic option for patients with allergic rhinitis and/or asthma. The majority of respondent paediatricians (93.6%) indicated that they refer the patients with allergic rhinitis and/or asthma to the paediatric allergy specialist for immunotherapy treatment option. 87.8% of respondent paediatricians agreed that the allergen specific immunotherapy should be administered and maintained under the supervision of the paediatric allergy specialist.
Number and percentages of responses to the items for attitudes of paediatricians in İzmir about ASI.
| Item | N | (%) |
|---|---|---|
| 1 – Do you believe that ASI may be valid therapeutic option in subjects with respiratory allergies (allergic rhinitis and/or asthma)? | ||
| Yes | 169 | 93.9 |
| No | 9 | 5 |
| No idea | 2 | 1.1 |
| 2 – Are you referring the patient with allergic rhinitis and/or asthma to the paediatric allergy specialist for immunotherapy treatment option? | ||
| Yes | 162 | 93.9 |
| No | 18 | 6.1 |
| No idea | – | – |
| 3 – Allergen specific immunotherapy should be administered and maintained under the supervision of a paediatric allergy specialist. | ||
| Agree | 158 | 87.8 |
| Disagree | 11 | 6.1 |
| No idea | 11 | 6.1 |
There were not significant differences between knowledge, perception and attitudes of paediatricians about ASI and experience of them.
DiscussionRespiratory allergic disease represents a significant health problem in both developed and developing countries.1 During the past four decades, a dramatic increase in the prevalence of allergic disease has occurred, and respiratory allergic disease is now the most common chronic disease among children and adolescents.2,3 This increase is especially problematic in children because of the prognosis of chronic and frequently aggravating disease.4 Respiratory allergic disease cause sleep impairment and reduce school performance.11 The quality of life of the children themselves and of their parents is usually affected.12,13
Current clinical guidelines recommend a combination of patient education, allergen avoidance, pharmacotherapy and ASI for respiratory allergic disease.9 Allergen avoidance is indicated whenever feasible, although, in practice, adequate symptom control is difficult to achieve with allergen avoidance alone. Although safe and inexpensive drugs are available for the treatment of allergic symptoms, pharmacotherapy has no effect on the progression of the disease and treatment has to be administered repeatedly as long as symptoms prevail. ASI is the casual treatment targeting the underlying allergic disease, affecting basic immunological tolerance.5 Induced tolerance implies disease modification, the clinical effects of which are reducing symptoms and drug consumption with a consequent improvement of the overall quality of life and prevention of the development of asthma in children with allergic rhinoconjunctivitis and also prevention of new allergic sensitisations.14 Clinical efficacy persists after discontinuation of ASI.15,16 The original administration form of ASI was by subcutaneous injection (SCIT). All injections are given in the doctor's surgery because there is a risk of severe or even life threatening allergic reactions. In the past 25 years, sublingual immunotherapy (SLIT) has emerged as an effective and safe alternative to the subcutaneous route for patients with respiratory allergic disease. However, ASI remains underused mainly because of: (1) a lack of agreement in documented efficacy and safety; (2) insufficient data on its cost-effectiveness; (3) difference in beliefs and educations of physicians taking care of allergic subjects; (4) lack of awareness of ASI in the general population and non-allergy/immunology trained population; (5) the reimbursement policy; and (6) long duration.17 ASI is estimated to be used in fewer than 10% of patients with allergic rhinitis or asthma worldwide.7
Paediatricians are usually the first-line specialists who affront the problems related to respiratory allergy in children. Paediatricians can refer the patients to the paediatric allergist for advanced treatments, such as ASI. ASI is prescribed by a paediatric allergist who diagnoses the disease and chooses the most appropriate ASI route. In such a setting, the present study was specifically designed for paediatricians in order to assess their perspective, knowledge on ASI and their attitude towards it. According to the results, it seems that the general knowledge on ASI is overall satisfactory among paediatricians and that they are well aware that ASI is recommended in patients with respiratory allergic disease, although they are not primarily responsible for the use and management of ASI in our country. Importantly, the majority of paediatricians (93.9%) agree that ASI may be a valid therapeutic option for subjects with respiratory allergic disease. And in the same way, the majority of them (93.9%) are referring the patients with respiratory allergic disease to the paediatric allergist for the immunotherapy treatment option. The main differences between SLIT and SCIT are also known among paediatricians, despite SLIT having been used in a comparatively recent time. In our study, the majority of respondents (n: 146) have worked for fewer than five years as a paediatric specialist, so these results may be associated with the fact that they have just completed their training and still follow the guidelines more closely than others (work time>5 years). It is not possible to compare our results with the previous ones because no survey in this sense has been attempted in the past in Turkey and the other countries. In a recent study in Italy, Landi et al. investigated the perception of allergen specific immunotherapy among paediatricians in the primary care setting. As a difference from our country, paediatricians represent the first-line contact and interface for prescription, use and management of ASI. Thus, it is not possible to compare our results with that study. But, similar to our study, Landi et al. found that, ASI is generally well-known and accepted among paediatricians. In this study a majority of paediatricians felt that a more intense divulgation and information about ASI would be needed. And about 50% of paediatricians still believe that ASI is an add-on therapy to be used when pharmacotherapy fails.18 In an another study, Lombardi et al. evaluated the overall level of knowledge about ASI among chest physicians. In this study, according to the results, it seems that the general knowledge on ASI overall satisfactory among pulmonologists and they are well aware that ASI is recommended in the most diffused guidelines and it has a disease modifying effect in addition to the short term clinical efficacy.19
In conclusion, because the ASI can prevent development of asthma in children with allergic rhinoconjunctivitis and new allergic sensitisations, the early and correct diagnosis of respiratory allergic disease and directing to these patients to the paediatric allergist is crucial in childhood. Our study provides the first assessments of paediatricians’ perception, knowledge and attitudes about ASI in Turkey. ASI is a generally well known and accepted treatment option among paediatricians in Izmir, Turkey. In our opinion, a better synergy between paediatricians and the paediatric allergist can provide more use of ASI for respiratory allergic diseases in childhood.
Authors’ contributionSakıne Işık, designed the study and wrote the manuscript. Şule Çağlayan-Sözmen, Atika Çağlar, Berna Eroğlu-Filibeli, Zeynep Arıkan-Ayyıldız contributed to data collection. Sakine Işık, Suna Asilsoy, Nevin Uzuner performed the statistical analysis and interpretation of the results. All authors read and approved the final manuscript.
Project was not supported by any funding.
Ethical disclosuresPatients’ data protectionConfidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors declare that they have no conflict of interest.
Our project was not supported and funded.