Experts from six Latin American countries met to discuss critical issues and needs in the diagnosis and management of primary immunodeficiency diseases (PIDD). The diagnosis of PIDD is generally made following referral to an immunology centre located in a major city, but many paediatricians and general practitioners are not sufficiently trained to suspect PIDD in the first place. Access to laboratory testing is generally limited, and only some screening tests are typically covered by government health programmes. Specialised diagnostic tests are generally not reimbursed. Access to treatment varies by country reflecting differences in healthcare systems and reimbursement policies. An online PIDD Registry Programme for Latin America has been available since 2009, which will provide information about PIDD epidemiology in the region. Additional collaboration across countries appears feasible in at least two areas: a laboratory network to facilitate the diagnosis of PIDD, and educational programmes to improve PIDD awareness. In total, these collaborations should make it possible to advance the diagnosis and management of PIDD in Latin America.
Primary immunodeficiency diseases (PIDD) include almost 200 types of inherited disorders with impaired host defenses and other immune dysfunctions.1,2 PIDD predispose affected individuals to recurrent infections, but, depending on the immune deficit, may also lead to the development of autoimmune diseases, inflammation, and malignancies.3,4 The incidence of these diseases varies considerably from approximately 1 in 250 for the more common forms to 1 in 1,000,000 for rare types. The actual frequency of PIDD is unknown, but some estimates range from 1:10,0003 to as many as 1:1200.5 The most common forms of PIDD involve antibody deficiencies, whereas most remaining cases are mainly caused by cellular, combined, or phagocytic defects.3,6 In 2007, the second report of the Latin American Group for Immunodeficiencies (LAGID) described the characteristics of 3321 PIDD patients from 12 Latin American countries with the most common category of PIDD (predominantly antibody deficiencies), accounting for 53.2% of the cases.7 This category was followed by other well-defined immunodeficiency syndromes, such as DNA repair defects, hyper-IgE syndrome, and thymic defects (22.6%), combined T- and B-cell immunodeficiencies (9.5%), phagocytic disorders (8.6%), immune dysregulation (3.3%), and complement deficiencies (2.8%). An earlier report from the same group also concluded that antibody deficiencies account for at least half of the PIDD cases in Latin America.8 An online PIDD Registry Programme for Latin America (the Latin American Society of Immunodeficiencies [LASID] registry) – available at http://deficiencia.unicamp.br:8080/ – was initiated in 2009, which will provide further information about PIDD epidemiology in the region.
Significant advances have been made over the last 15 years in the diagnosis and management of PIDD, resulting in reduced rates of morbidity and mortality.9,10 North American and European guidelines have been published providing recommendations on how patients with suspected PIDD should be evaluated, which tests should be conducted to reach a specific diagnosis, and how patients should be treated depending on the type and severity of PIDD.3,11 Nevertheless, awareness about PIDD and access to appropriate treatment may be restricted in some regions of the world. On October 14, 2009, a group of PIDD experts from six Latin American countries (Argentina, Brazil, Chile, Colombia, Honduras, and México) and representatives from LASID met in Cartagena de Indias, Colombia to discuss critical issues and needs related to each country separately and to the regions as a whole. This report provides a summary of these discussions.
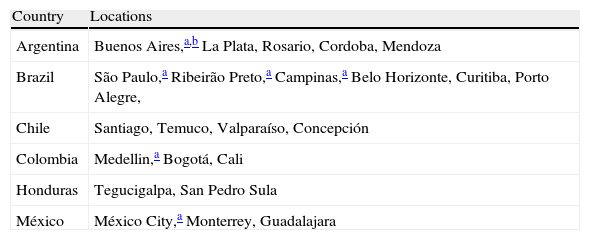
Current status and issues in PIDD diagnosisThe diagnosis of PIDD is generally made after patients are referred to an immunology centre with specific expertise in these disorders. Most centres are located in major cities of each country (Table 1). Unfortunately, many paediatricians and general practitioners, as well as specialists in areas related to these disorders, are not sufficiently trained to suspect PIDD in the first place. This represents a critical issue in each country, because it delays the diagnosis and leaves many patients without appropriate treatment, both of which contribute to PIDD-associated morbidity and mortality. The Jeffrey Modell Foundation has recently shown that physician education and public awareness might significantly impact the early diagnosis of PIDD;12 therefore, physicians educated to recognise at least the warning signs for PIDD can start to suspect PIDD and refer patients to immunologists for appropriate follow-up. The role of the immunologist is to confirm the diagnosis and indicate the most appropriate treatment and follow up. Therefore, referral to an immunology centre represents a critical step in the diagnostic process, and highlights the need to increase awareness about PIDD among Latin American physicians.
Location of immunology centres for supporting a PIDD diagnosis.
| Country | Locations |
| Argentina | Buenos Aires,a,b La Plata, Rosario, Cordoba, Mendoza |
| Brazil | São Paulo,a Ribeirão Preto,a Campinas,a Belo Horizonte, Curitiba, Porto Alegre, |
| Chile | Santiago, Temuco, Valparaíso, Concepción |
| Colombia | Medellin,a Bogotá, Cali |
| Honduras | Tegucigalpa, San Pedro Sula |
| México | México City,a Monterrey, Guadalajara |
Several immunology centres in Argentina can support a diagnosis of PIDD, most of which are located in Buenos Aires. Two of the five centres in Buenos Aires – Hospital de Pediatría “Prof Dr Juan Garrahan” and Hospital de Niños Ricardo Gutiérrez – have comprehensive immunology programmes with state-of-the-art facilities for immunological and molecular diagnosis. Other hospitals located in La Plata (Sor Ludovica), Rosario, Cordoba, and Mendoza can also support a PIDD diagnosis, but none have well-equipped facilities for molecular diagnosis. Moreover, only one of them, Hospital Durand in Buenos Aires, treats adult patients. Patients who are referred to an immunology centre in Argentina will be seen by trained immunologists and receive treatment, if necessary. In general, these centres are accessible and without cost to patients providing they are referred by a physician. Private hospitals provide only a partial solution, because they lack immunology laboratories and trained immunologists to support a PIDD diagnosis.
In Brazil, the diagnosis of PIDD is supported by immunology centres in a few large cities, including São Paulo, Ribeirão Preto, Campinas, Belo Horizonte, Curitiba, Porto Alegre, Salvador, and Rio de Janeiro. Of these, São Paulo, Ribeirão Preto, and Campinas have university centres qualified for comprehensive laboratory testing, including molecular diagnosis. Approximately 10 other centres, also located in large cities, are able to recognise patients with PIDD but only have the facilities to do basic lab exams and thus need support from São Paulo. The government sponsors a programme for patients who do not have specialists in their hometown that pays for travel to another city for diagnosis. However, patients living in some regions of the country must travel long distances from poorly developed areas to reach these centres, thus impacting accessibility. Apart from the limited physician awareness of PIDD, restricted access to clinical laboratories and reimbursement for diagnostic testing are critical issues for PIDD diagnosis in Brazil. The federal government provides coverage for basic screening tests, such as serum immunoglobulin levels and blood cell counts, but not for determining lymphocyte subpopulations or other specialised tests whose costs are borne by the immunology centres. Interestingly, the government pays for CD3, CD4, and CD8 testing in HIV patients but not for PIDD patients. These issues are illustrated in a survey conducted in 200513 – 4 years after an educational programme was started in Brazil. Surveys were sent to 34,117 paediatricians, but only 3047 (8.9%) responded. Most (97%) indicated that they care for patients with recurrent infections, and 62% responded that they had evaluated at least one patient for PIDD. When asked to identify the greatest difficulty in investigating a patient for PIDD, cost and laboratory access were the top responses. (Results available at http://www.bragid.org.br/download/graphicos.pps).
As in the other countries, the diagnosis of PIDD in Chile is most often made after a patient is referred to an immunologist in a major city, though some are referred with a diagnosis. In many cases, the paediatrician or general practitioner will not suspect PIDD, and first refer the patient to an infectious disease specialist, who will subsequently refer the patient to an immunology centre for actual diagnosis. The public health system network – which covers approximately 75% of the population – allows patient referral from primary care centres to local hospitals and subsequently, to major centres. In Chile, Santiago and Temuco have the best laboratories for diagnosis, but Valparaíso and Concepción are also important centres. There are trained immunologists located in hospitals in some larger cities, such as Valparaíso, Concepción, Valdivia, Copiapó, Antofagasta, and Temuco. However, none of these, (except Temuco) have comprehensive laboratories. Usually, larger hospitals provide coverage for basic screening tests, such as serum immunoglobulin levels and blood cell counts, and in some cases, for determining lymphocyte populations or other specialised tests. Six hospitals in Santiago, half of which are paediatric hospitals, receive PIDD patients from throughout Chile. Laboratory testing for PIDD can be supported at three major laboratories – two in Santiago and one in Temuco. However, the public health system does not pay for these tests, and therefore the cost must be borne by the patient or the hospital. Accordingly, access to immunological laboratory testing remains a critical issue for PIDD diagnosis in Chile.
In Colombia, the Group of Primary Immunodeficiencies at the University of Antioquia in Medellín is a national referral centre for PIDD and is well equipped to perform both immunological and molecular diagnosis (for some diseases). Other programmes are being developed in Bogotá and Cali, and there are prospects for other programmes in Cartagena and Barranquilla. Most clinical laboratories in Colombia can measure immunoglobulin levels, and every major city has at least one laboratory capable of performing basic flow cytometry testing on lymphocyte populations. However, specialised immunological testing is only available in Medellín and for some tests, Bogotá. Two general strategies were instituted during the last five years to improve PIDD diagnosis. First, an outpatient group, the Group of Primary Immunodeficiencies at the University of Antioquia, for recurrent infections was established instead of a PIDD clinic, which has resulted in large numbers of referrals – an average of 20 to 25 new patients each week at the Medellin centre. Second, educational efforts for physicians, nurses, and medical students were focused mostly on recurrent infection, with PIDD discussed as a potential cause. This experience showed that physicians are receptive to information about recurrent infection, but are not very interested in learning about the cells and molecules involved in immune function, probably due to the lack of proper knowledge about immunology. This is a problem that has its roots in some graduate medical programmes in medical schools in Colombia. However, paediatricians and general practitioners (as well as specialists from other areas) have been showing increased awareness about PIDD, but mostly at sites where continued medical education is consistently provided. Although these physicians refer patients to immunologists, few immunologists in Colombia are actually fully trained in PIDD, and therefore, most patients must subsequently be referred to the main centre.
Presently, about 80% of PIDD cases come from the state of Antioquia and neighbouring states even though this represents less than 20% of the population. This disproportion reflects the increased awareness of PIDD through local educational efforts. Despite the success of this programme, it is important for physicians to recognise that PIDD can present without recurrent infection. For example, some forms of PIDD, such as hyperimmunoglobulin E syndrome and chronic granulomatous disease, present with inflammatory changes long before diagnosis. Therefore, a more global educational effort has been recently implemented that includes information on the association of PIDD with autoimmunity, inflammation, and cancer.
Honduras has two major health systems: public health and social security provide coverage for approximately 70% and 25% of the population, respectively, with 5% having private insurance. PIDD patients in Honduras are diagnosed after referral to major centres in Tegucigalpa or San Pedro Sula, with access to these centres available to all patients. The greatest challenges to diagnosis are laboratory access and the costs related to testing. The only immunology laboratory able to support a PIDD diagnosis is located in Tegucigalpa.
In México, identification of hypogammaglobulinaemia can be made in most cities, whereas lymphocyte phenotyping and specialised testing are available only in major cities including México City, Monterrey, Guadalajara, and in most state capitals. The molecular and genetic diagnosis can be made only at one centre in México City, and for only a limited number of PIDD patients. In addition to the need to educate physicians to consider PIDD, access to laboratory testing and its associated cost are the greatest challenges to diagnosis, because only 60–70% of the Mexican population has public or private health insurance.
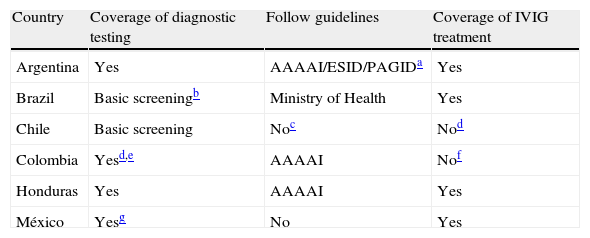
Current status and issues in PIDD treatmentDespite the proven effectiveness of intravenous immunoglobulin (IVIG), accessibility to treatment and reimbursement of treatment costs differ by country (Table 2). Moreover, practise guidelines from other regions (e.g., North American Academy of Allergy, Asthma, and Immunology [AAAAI] guidelines)3 are not uniformly followed across Latin America. In Argentina, patients from regions that do not provide coverage for PIDD must travel to Buenos Aires for treatment, although a new law is being organised that will require each region to offer treatment for their own patients. Treatment with IVIG is not automatically continued when patients enter adulthood, because they need to be transferred from a paediatric hospital to a general hospital for adults. In some cases, patients may have to wait for 1 or 2 years before resuming IVIG treatment. Alternatively, it is sometimes possible for the paediatrician to continue care until coverage is again acquired. PIDD patients from Paraguay, Bolivia, and Uruguay also come to hospitals in Buenos Aires for diagnosis and treatment, because these countries do not have appropriate facilities. An estimated 20% of PIDD patients seen at the Hospital de Niños Ricardo Gutiérrez come from these adjacent countries, but they do not have health insurance and their countries do not pay for their medical care. This creates a financial burden on the immunology centres in Argentina.
Coverage of diagnostic testing and IVIG treatment across countries.
| Country | Coverage of diagnostic testing | Follow guidelines | Coverage of IVIG treatment |
| Argentina | Yes | AAAAI/ESID/PAGIDa | Yes |
| Brazil | Basic screeningb | Ministry of Health | Yes |
| Chile | Basic screening | Noc | Nod |
| Colombia | Yesd,e | AAAAI | Nof |
| Honduras | Yes | AAAAI | Yes |
| México | Yesg | No | Yes |
AAAAI=American Academy of Allergy Asthma and Immunology; ESID=European Society for Immunodeficiencies; PAGID=Pan American Group for Immunodeficiencies.
Complex laboratory tests are performed at public university centres in the State of São Paulo and the expenses covered by research programmes supported by government research agencies. Patients do not have to pay.
Guidelines are usually followed for patients with private insurance; IVIG treatment follows AAAAI guidelines.
The AAAAI guidelines are not followed in Brazil; instead, efforts are underway to prepare national guidelines for IVIG administration in collaboration with the Associação Brasileira de Alergia e Imunopatologia (ASBAI, Brazilian Association of Allergy and Immunopathology). The guidelines require support of a relevant national medical society, because IVIG is reimbursed by the government. Guidelines from other countries or regions are not implemented by the Brazilian government, regardless of the supporting clinical evidence. Currently, the guidelines from the Ministry of Health published in 2006 are followed. Patients must first be admitted in order to receive IVIG treatment at most hospitals, although some centres provide treatment at day clinics. Because IVIG is fully reimbursed by the government, the greatest challenge for treatment is accessibility to a treatment centre. Private insurance usually does not provide reimbursement for regular treatment with IVIG for PIDD, and therefore, even patients with good private insurance have to receive IVIG through the government.
The situation in Chile is very different from that in Brazil. IVIG is not reimbursed by the public health system for PIDD, even though it is reimbursed for other indications including transplantation, HIV, and Kawasaki disease. Accordingly, it is often quite difficult to treat PIDD patients under the public health system in a manner specified by guidelines. For those with private insurance, the AAAAI guidelines are usually followed. In some cases, the hospital will pay for IVIG treatment for 6 to 12 months, but then treatment will stop until special approval can be obtained from the hospital director or ethics committee. This approval process may need to be repeated periodically. When available, IVIG is always administered in the hospital. The greatest challenge for patients to receive treatment is obtaining reimbursement; however, attempts to resolve this issue are currently being made.
In Colombia, a basic health plan (Plan Obligatorio de Salud [POS]) provides basic universal coverage for everyone, and then additional coverage can be purchased from private insurance companies. Although the social healthcare and legal systems support PIDD treatment to a certain extent, IVIG is not included in the POS. Nevertheless, IVIG treatments are covered by the healthcare insurers; they are reimbursed by the government through a special fund called FOSYGA. However, in some instances treatments are denied, and legal approaches must be used to overcome these limitations, making treatment generally accessible depending on the disease severity. The Fundación Diana Garcia de Olarte for PIDD (FIP) was created about 4 years ago, and as a national organisation, supports and develops educational programmes and provides advice in addressing legal issues that most patients face when it comes to getting IVIG. The foundation provides the infrastructure to get patients to centres where they can receive treatment. Treatments in the Medellin Centre usually follow the AAAAI practise guidelines.
In Honduras, the availability and cost of IVIG are critical issues. AAAAI practise guidelines are usually followed when IVIG is available. IVIG treatment is usually administered in a hospital, but notably, only two hospitals in Tegucigalpa, including the Instituto Hondureno de Seguridad Social, actually offer treatment. Other hospitals in Honduras do not have IVIG.
In México, patients in the public health system have access to IVIG, but most physicians do not follow any specific guidelines. Instead, physicians commonly use the product empirically based on personal experience, or based on training by one of the pharmaceutical companies that sells IVIG. A regimen of 400mg/kg/dose is generally used, but few centres regularly adjust the dose according to IgG levels. Most IVIG is administered at government hospitals or clinics. There are six different brands of IVIG in México, but product availability and cost are still problematic. IVIG represents a sizeable fraction – perhaps 20% – of the drug budget in the Instituto Nacional de Pediatría in México City. For new patients, efforts are made to find a legal job that provides health coverage so that IVIG will be reimbursed by the government health system. By law, every company in México must provide health insurance, but 30–40% of the population works in a non-legal, informal manner without health insurance. Universal health coverage is expected to be instituted soon in Mexico, which should make it easier to provide IVIG to every PIDD patient.
Current status in immunology educationEducational systems and residency programmes in immunology differ across Latin America. In Argentina, immunology is not recognised as a speciality by the Public Health Ministry, but efforts are ongoing with the Argentina Immunology Society to change this situation. Two hospitals in Buenos Aires (Hospital de Niños Ricardo Gutiérrez and Hospital Nacional de Pediatría “Prof Dr Juan P. Garrahan”) offer medical and biochemical residency programmes and provide 1- to 2-year scholarships for projects in an immunology speciality funded by government agencies. Postgraduate immunology programmes are not available in other parts of the country. Since 2004, the Immunology Unit of the Hospital de Niños Ricardo Gutiérrez has offered an annual postgraduate course entitled The Immunology of Today: from Molecular to the Clinic. In addition, doctors from the Hospital de Niños Ricardo Gutiérrez and Nacional de Pediatría “Prof Dr Juan P. Garrahan” travel from Buenos Aires to the provinces to provide information and courses about different immunological diseases to physicians and biochemists.
Funded residency programmes in allergy/immunology are available in Brazil. However, few centres offer clinical immunology training and treat PIDD patients in the country. In order to gain experience in PIDD, residents and fellows must come to major university centres in the State of São Paulo, where they will receive an additional certificate upon completion of a 2-year programme. However, it has been difficult to maintain these programmes, because residents and fellows do not receive funding for training specifically in PIDD. Funded postgraduate programmes are available, in which fellows spend 2 to 6 years on a specific research programme in addition to receiving clinical training. Upon completion, the fellows receive either an MSc or PhD degree.
Chile has one residency programme in immunology at the University of Chile in Santiago. This 3-year programme includes education about basic immunology, autoimmune diseases, allergy, and immunodeficiencies, and provides training in both paediatric and adult disorders. Three or four fellows enrol each year. After completing the programme, some fellows have moved to other cities in Chile, which has spawned a network of immunologists across the country.
Colombia has a formal immunology programme for residents at the University of Antioquia in Medellin, who are being trained in specialties, such as paediatrics and dermatology. However, most participants choose to work in allergy or other paediatric disciplines, because they can earn more money than specialising in PIDD. Honduras does not have a residency programme specifically for immunology. However, paediatricians receive training in basic immunology, autoimmunity, allergy, and immunodeficiencies once per week over 3 months.
In México, several allergy/immunology residency programmes are available, but most have an allergy focus. The programme at the Instituto Nacional de Pediatría in México City is the only one offering a balance between allergy and immunology. The fellows spend at least one year in clinical immunology, and at least one month in the PIDD clinic. Programmes in paediatric allergy and immunology are open after 3 years of paediatric training, and those in adult allergy and immunology are open after 2 years of internal medicine training.
Educational needs and opportunitiesThere is a common need across countries to increase awareness about PIDD. Continuing education and training programmes are needed for paediatricians and general practitioners, as well as for specialists, to ensure that they can recognise the warning signs for PIDD, particularly for those practising in regions away from the large cities of each country. These programmes would improve early diagnosis and promote referrals to immunologists. To support these efforts, PIDD symposia need to be included in paediatric and internal medicine congresses. Summer school programmes are needed for young immunologists to help create networks of trained immunologists, and ensure that they have up-to-date information about PIDD. Importantly, educational efforts should not only focus on general physicians and specialists, but should also include medical school students, nurses, and the general public. In all educational efforts, it is important to take the mystery out of immunology and PIDD. Funding for these programmes is a critical issue.
The Internet is a powerful educational tool that is being increasingly used to disseminate PIDD information. In Brazil, the number of physicians registered on the Brazilian Group for Immunodeficiency (BRAGID) Web site (http://www.bragid.org.br) has increased dramatically from 190 (in 2002) to over 2500 (in 2009). Awareness of the site increased after it was discussed at local/regional seminars and in educational materials. The site offers an opportunity to discuss clinical cases on the Internet. Moreover, BRAGID offers a brochure describing the warning signs for PIDD, clinical presentations according to disease type, and first steps to take including which laboratory to contact. The back of the brochure lists normal immunoglobulin levels and lymphocyte counts by age. The brochure is distributed at seminars and is also published on the Web site. Approximately 80,000 warning-sign cards and other educational material have already been distributed to physicians throughout the country. In Brazil, there are three patients’ associations (one in Belo Horizonte and two in São Paulo) which work independently but with the same objective. Similarly, in Colombia, the FIP has a Web site and produces brochures, cartoons, and videos which explain how the immune system works and what PIDD are; how to use IVIG; and identify options for PIDD patients.
In Argentina, the government is not aware of the magnitude of PIDD, and therefore immunologists must work alone without government support to increase awareness. Workshops about PIDD are needed throughout the country to stimulate young physicians and biochemists, but outside collaboration will be necessary to make these a reality. Some teams have started to work on increasing awareness about PIDD in the community. Presentations by immunologists and psychiatrists provide information about PIDD and how it impacts the family. A play with several clowns has been organised by the Asociación de Ayuda al Paciente con Immunodeficiencia Primara (AAPIDP; http://www.aapidp.com.ar) to offer information about PIDD to patients and their families. Finally, patients and family members have started to work with the immunology centres to increase PIDD awareness. In Brazil, the Jeffrey Modell Foundation opened a PIDD diagnostic centre in São Paulo in 2007, involving major institutions in the area with the goals of advancing educational programmes, improving diagnosis, and implementing the online PIDD Registry in Latin America. Another diagnostic centre sponsored by the Jeffrey Modell Foundation is open in Mexico City, which has produced posters and promoted radio and television advertisements in order to increase public awareness about PIDD. Similar diagnostic centres are expected to open soon in Medellin, Colombia and Santiago, Chile.
Summer schoolsSummer schools may represent a viable solution for Latin America, inasmuch as educational systems and residency programmes differ by country. The objective of these programmes is to provide education about PIDD to young physicians and promote scientific interactions with established investigators. The first summer school in Latin America was held in São Paulo in 2006, and was patterned after similar programmes sponsored by the European Society of Immunodeficiencies (ESID) and Clinical Immunology Society (CIS). The two and a half day meeting included 36 students and 12 faculty members from LAGID, ESID, and CIS. Topics at future summer schools should be of general interest, potentially including sessions on (a) laboratory and molecular diagnoses of PIDD; (b) types of PIDD, such as common variable immunodeficiency or X-linked agammaglobulinaemia; (c) guidelines for IVIG therapy; (d) bone marrow transplantation in Latin America; and (e) the laboratory network in Latin America –LATIM America – where they are, what they do, and how to send samples. In addition, students with research projects could be selected to make presentations. Agreement was reached that a summer school should be held every two years, with the site and organisational responsibilities rotating among countries. A small summer school was held in Temuco, Chile in August 2008. The most recent summer school included 90 students and took place in April 2010 in Bahia, Brazil. Additional summer schools are planned in Chile, Peru, and other countries.
PIDD registryThe online PIDD Registry for Latin America – adapted from a similar registry established by ESID in Europe – is supported by the Jeffrey Modell Foundation and by a research agency in Brazil: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The system can be accessed at http://deficiencia.unicamp.br:8080/. The kickoff meeting, held on April 28-29, 2009, in São Paulo, was attended by 90 participants from Argentina, Brazil, Chile, Colombia, Honduras, and México. Participants received information and training on the use of the Web-based registry. Three faculty members from the United States and a faculty member representing ESID assisted the host Brazilian faculty in presenting the programme. The success of the programme is reflected by early results: 24 centres have enrolled, and more than 600 patients have been registered. This has become a very important component of ongoing efforts to enhance information, diagnosis, and treatment of PIDD in Latin America, and has helped ongoing development of diagnostic centres in the region.
SummaryHealthcare systems differ across Latin America, making it difficult to initiate a common programme across the region. Notably, access to treatment and reimbursement policies differ from country to country. Nevertheless, there are a number of common issues regarding PIDD. Access to laboratory testing is generally limited or, if available, costs to cover testing are problematic. Some screening tests are covered by governmental health programmes, but specialised diagnostic tests are typically not reimbursed. Not all centres can conduct all diagnostic tests, due to the inherent cost. This highlights the need for a laboratory network in the region, and to identify the infrastructure necessary for shipping samples across borders. Access to IVIG for treatment of PIDD patients with antibody deficiency needs to be promoted and supported by health authorities. Education is another common need in the region. Programmes designed for paediatricians, general practitioners, specialists, nurses, patients, families, and the general public must be developed in order to increase awareness about PIDD. Successful programmes in one country may serve as templates for new programmes in other countries. Summer school programmes represent a strategy that can be used to bridge the educational needs of the entire region. Together with the ongoing PIDD Registry Programme for Latin America, these collaborative efforts should make it possible to advance research and improve diagnosis and management of PIDD in Latin America.
Conflict of InterestJosé Luis Franco has received consulting fees from Baxter. All other authors declare no conflicts of interest.
The authors thank Baxter Biosciences for supporting the Latin American Advisory Board on Primary Immunodeficiencies initiative as well as supporting the editorial services for the development of the proceedings of this initiative.