The International Study of Asthma and Allergies in Childhood (ISAAC) identified trends in the prevalence of symptoms of asthma, rhinoconjunctivitis and eczema over a seven-year period. We hypothesised that environmental influences on the three diseases are different and therefore investigated the correlation over time between trends in the prevalence of these diseases and their combinations at centre and individual level.
MethodsCentre level analyses were correlations between time trends in the prevalence of symptoms. At an individual level, odds ratios were calculated for associations between symptoms between Phases One and Three. We also investigated potential effect modification in the younger versus older age group; male versus female; and by average Gross National Income per capita (GNI).
ResultsBoth phases were completed in 66 centres in 37 countries for the 6–7 year age group and in 106 centres in 56 countries for the 13–14 year age group. We found that the correlations in time trends were stronger for the older age group than the younger one. Between symptoms of diseases, correlations of time trends were the strongest for rhinoconjunctivitis with eczema and weakest for eczema with asthma. The relationship between the three diseases was generally consistent over the seven-year period, and there was little association found with average GNI.
ConclusionsDespite some increase in the proportion of children with symptoms of asthma, rhinoconjunctivitis and eczema, the pattern between the three diseases has not changed much, suggesting that similar factors may be affecting them at a global level.
The International Study of Asthma and Allergies in Childhood (ISAAC) epidemiological research programme was established in 1991 because of concern that asthma and allergies were increasing in prevalence and severity, but little was known about the world scale of the problem and the factors affecting prevalence.1 ISAAC Phase One found large variations in the prevalence of symptoms of asthma,2 rhinoconjunctivitis3 and eczema.4 In ISAAC Phase Three time trends in these diseases were examined a mean of seven years after Phase One.5–7 Most centres showed a change ≥1 standard error (SE) in prevalence of at least one condition, with increases being twice as common as decreases, and increases more common in the 6–7 year olds than 13–14 year olds.8
We hypothesised that environmental influences on asthma, rhinoconjunctivitis and eczema are different and therefore the changes in prevalence over time would vary in an inconsistent manner for each of these diseases – the null hypothesis being that they would remain in the same relationship with each other. In this paper the relationship between trends in prevalence of symptoms of asthma, rhinoconjunctivitis and eczema and combinations of symptoms are examined at centre level, along with combinations of these symptoms at individual level to answer the question ‘Do worldwide symptoms of asthma, rhinoconjunctivitis and eczema show the same time trends?’ We also examined whether the relationship between the three diseases within individuals changed over time for the whole population.
Materials and methodsISAAC Phase Three is a multi-centre multi-country cross-sectional study of two age groups of school children (13–14 year olds and 6–7 year olds) chosen from a sample of schools in a defined geographical area. The study instruments are simple standardised questionnaires with questions on symptoms of asthma, rhinitis and eczema. Each Phase Three centre conducted the study in the same way as Phase One to ensure comparable trend data. The details of the study design and methods are described elsewhere.9 Centres obtained ethics approval. This paper reports on those centres which completed an ISAAC Phase Three study 5–10 years after completing Phase One in which the methodology met the ISAAC quality control standards. Only centres which completed both Phase One and Phase Three studies and submitted data for asthma, rhinitis and eczema are the subjects of this paper.
Answers to written questions were reported by parents of children (6–7 years) and self-reported by adolescents (13–14 years). In this paper current symptoms of asthma were estimated from positive answers to the written question “Have you (Has your child) had wheezing or whistling in the chest in the past 12 months?”. Symptoms of severe asthma were defined as those with current wheeze who in the past 12 months have had >4 attacks of wheeze, or >1 night per week sleep disturbance from wheeze, or wheeze affecting speech. Current symptoms of rhinoconjunctivitis were estimated by positive answers to both these questions: “In the past 12 months have you (has your child) had a problem with sneezing or a runny or blocked nose when you (he/she) DID NOT have a cold or the flu?” and if yes, “In the past 12 months has this nose problem been accompanied by itchy watery eyes?”. The answer “a lot” to this question: “In the past 12 months, how much did this nose problem interfere with your (child's) daily activities?” was used to assess the prevalence of severe rhinoconjunctivitis symptoms. Current symptoms of eczema were estimated by positive answers to these questions: “Have you (Has your child) ever had this itchy rash at any time in the past 12 months?” (this question was preceded by the question “Have you (Has your child) ever had an itchy skin rash which was coming and going for at least 6 months?”) and if yes: “Has this itchy rash at any time affected any of the following places: the folds of the elbows, behind the knees, in front of the ankles, under the buttocks, or around the neck, ears or eyes?”. Current eczema associated with sleep disturbance one or more nights per week was used as a surrogate of severe eczema.
The data analyses were of three types. Firstly correlations of time trends in each disease were examined at centre level. An estimate of the average absolute rate of change per year of prevalence of symptoms of asthma, rhinoconjunctivitis and eczema was derived for each centre. Weighted correlations of time trends for each condition with each other condition were calculated for each age group. The weights were the average of the inverse of the variance of rate of change in prevalence. Secondly, we examined the inter-relationship between the three diseases at an individual level, across all centres combined. This was illustrated by scaled rectangle diagrams of the prevalence of combinations of current symptoms in all the participating children for each age group for Phases One and Three. We also examined the relationship of each of the diseases with each other disease separately in Phase One (ORPh1) and in Phase Three (ORPh3) (shown in Web Tables 1 and 2). Each association was measured by the odds of symptoms of one disease given the symptom status of another disease. Thirdly to investigate potential changes in associations between the diseases over time, we plotted the ratio of the two odds ratios (ORPh3/ORPh1 with 95% confidence intervals (CI)) for the following: 6–7 year age group versus 13–14 year age group for each gender; male versus female gender for each age group; for any one combination of symptoms versus any other combination of symptoms (or versus one symptom) for each age group; and by average Gross National Income per capita (GNI) for each age group by taking the average GNI between 2001 and 1994 for each country. Chi Square tests were undertaken for homogeneity of the ratios of odds ratios in the GNI analyses. GNI was unavailable in either year for Taiwan, and for 1994 in four other centres where the nearest available year was used (1995 for Iran and Kuwait, 1996 for Isle of Man and 2000 for Channel Islands).
ResultsThe median time period between phases was seven years (range 5–10 years) with Phase One data collection between 1991 and 1998 (mostly 1994–1995) and Phase Three between 1999 and 2004 (mostly 2002–2003). In Phase Three there were 193,404 participants in the 6–7 year age group from 66 centres in 37 countries and 304,679 participants in the 13–14 year age group from 106 centres in 56 countries, with mean response rates of 84.8% and 90.9%, respectively. The results for change per year for prevalence of symptoms of asthma, rhinoconjunctivitis and eczema have been reported elsewhere.8
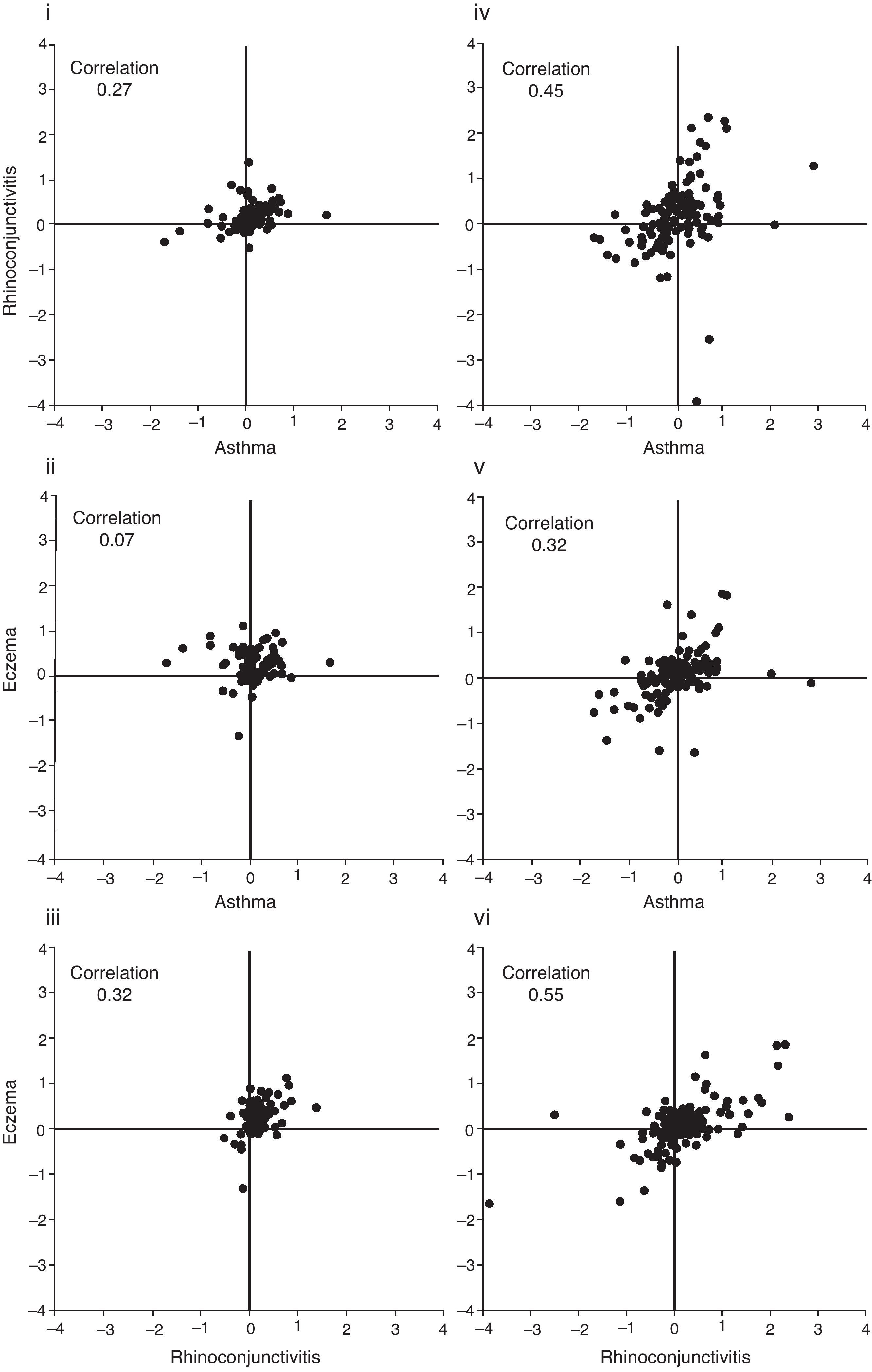
Firstly we considered the correlations of time trends in each disease at a centre level shown in Fig. 1(i–vi). Disease trends were more highly correlated in the older age group than the younger. Within each age group, correlations were highest for time trends of symptoms of rhinoconjunctivitis with symptoms of eczema; intermediate for time trends of symptoms of rhinoconjunctivitis with symptoms of asthma; and lowest for time trends of symptoms of eczema with symptoms of asthma. There was very little correlation between time trends of symptoms of eczema and symptoms of asthma in the younger age group.
(i–vi) Correlations of time trends (average % change in symptoms per year for Phase One and Phase Three) for each condition with another condition for each age group. Each dot represents a centre. The correlations illustrated are (i) symptoms of asthma and symptoms of rhinoconjunctivitis, 6–7 year age group; (ii) symptoms of asthma and symptoms of eczema, 6–7 year age group; (iii) symptoms of rhinoconjunctivitis and symptoms of eczema, 6–7 year age group; (iv) symptoms of asthma and symptoms of rhinoconjunctivitis, 13–14 year age group; (v) symptoms of asthma and symptoms of eczema, 13–14 year age group; and (vi) symptoms of rhinoconjunctivitis and symptoms of eczema, 13–14 year age group.
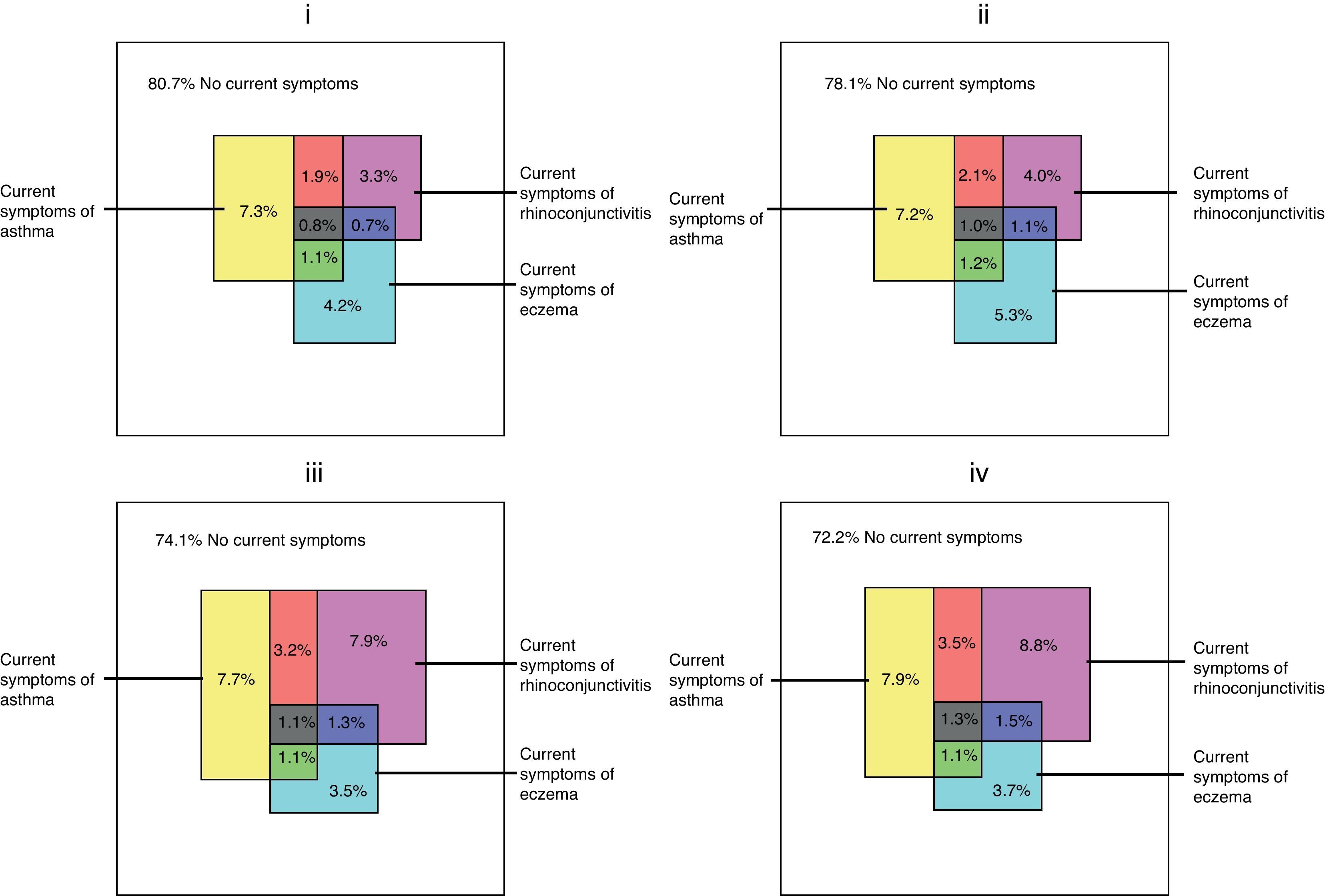
Secondly, we examined the inter-relationship between the three diseases at an individual level, across all centres combined. Scaled rectangle diagrams of the prevalence in all the participating children of current symptoms and their combinations drawn in Fig. 2(i–iv) showed that the pattern of intersection between the three diseases was similar in each phase for each age group.
(i–iv) The relationships at the individual level of symptoms of asthma, rhinoconjunctivitis, and eczema for each age group in Phase One and Phase Three. The outermost rectangle represents the whole population. The plots presented are for (i) Phase One, 6–7 year age group; (ii) Phase Three, 6–7 year age group; (iii) Phase One, 13–14 year age group; and (iv) Phase Three, 13–14 year age group.
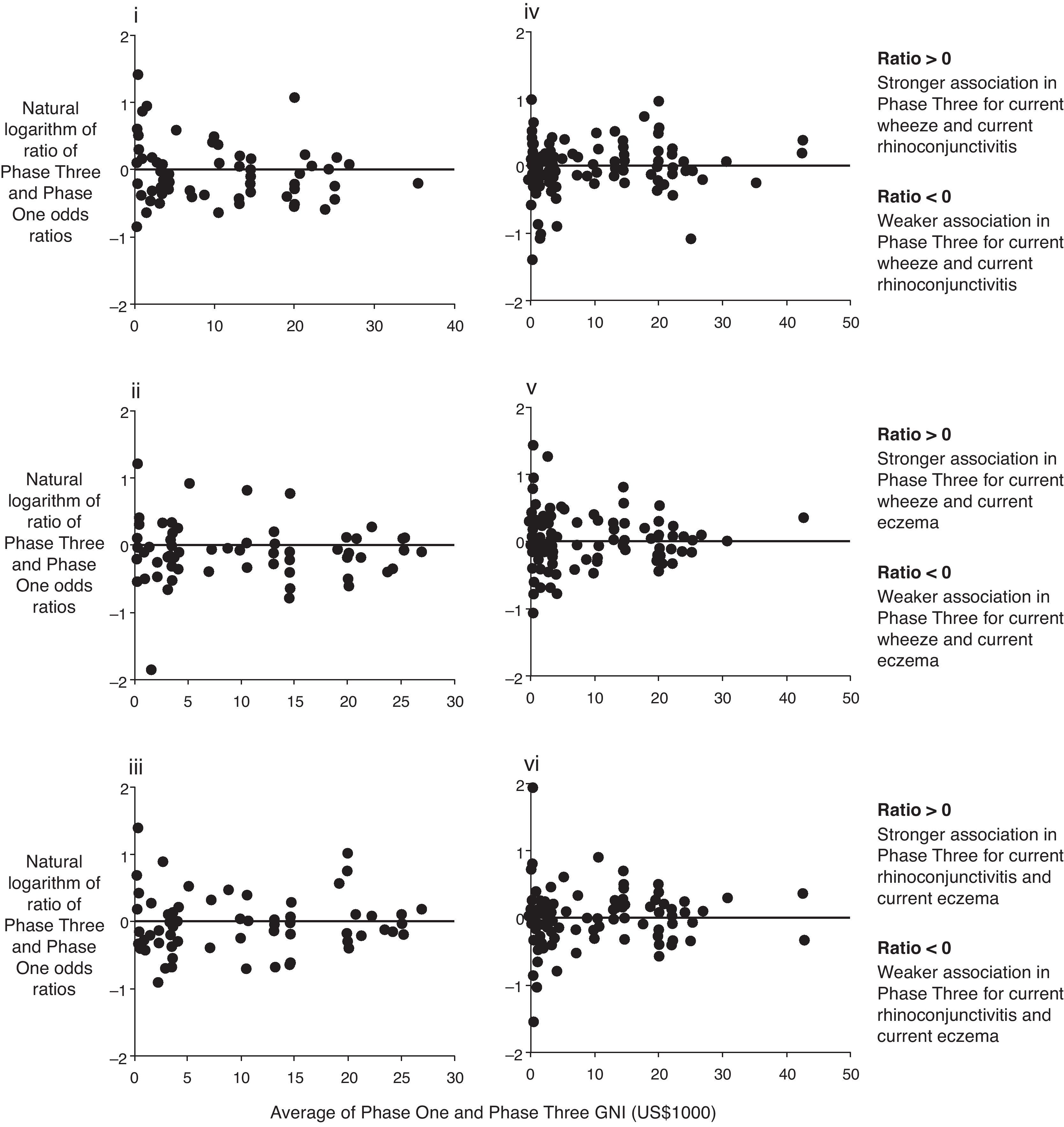
Thirdly, we assessed how the relationship between symptoms of each disease, measured at the individual level, had changed over time in centres of varying affluence (GNI). Fig. 3(i–vi) shows that the associations changed in a similar manner in countries of all levels of GNI (low to high income) between Phase One and Phase Three. The general pattern was for little change in the patterns of association. However, in the younger age group, for all comparisons, there were more centres with weaker associations between the diseases in Phase Three than Phase One, across the range of country level GNI. The Chi Square statistic for homogeneity showed no evidence for variation between centres (p values of 0.97–1.00).
(i–vi) Average GNI (1994 and 2001) and the ratio of Phase Three and Phase One odds ratios (log transformed) for symptoms of the three conditions. Each dot represents a centre. The plots presented are for the ratio of Phase Three and Phase One odds ratios of (i) symptoms of asthma (outcome) and symptoms of rhinoconjunctivitis (exposure), 6–7 year age group; (ii) symptoms of asthma (outcome) and symptoms of eczema (exposure), 6–7 year age group; (iii) symptoms of rhinoconjunctivitis (outcome) and symptoms of eczema (exposure), 6–7 year age group; (iv) symptoms of asthma (outcome) and symptoms of rhinoconjunctivitis (exposure), 13–14 year age group; (v) symptoms of asthma (outcome) and symptoms of eczema (exposure), 13–14 year age group; and (vi) symptoms of rhinoconjunctivitis (outcome) and symptoms of eczema (exposure), 13–14 year age group.
Finally, no consistent underlying patterns were found for analyses by gender, comparison of the two age-groups, or for any one combination of symptoms versus any other another combination or versus one symptom.
DiscussionThis is the first worldwide study of changes over time in the relationship between symptoms of asthma, rhinoconjunctivitis and eczema at both ecological and individual levels. This study has wide relevance because it has included 106 centres in 56 countries from all world regions and low, middle and high income countries, with a wide range of symptom prevalence values and changes over time using the same methodology.8
There was little association found with average GNI as the associations changed in a similar manner in countries of all income levels. The analyses by GNI were done at country level, because GNI is a country only estimate. However GNI may mask large socioeconomic inequalities within countries, with high proportions of people living in greater economic deprivation than the GNI would indicate because the greater part of income share is held by a minority.10,11 Thus GNI may not reflect the situation occurring in population subsets as suggested by cases where there is important variation in prevalence found between centres in the same city (e.g. Mexico City). The country level symptom prevalence for comparisons with GNI was estimated from the average of centre prevalence with few national samples included. We recognise that country level prevalence thus obtained may not be a true reflection of country prevalence. This approach has also been used in other ISAAC analyses.12–16 Thus caution is needed in interpreting this data.
Our findings do not support our hypothesis that environmental influences on asthma, rhinoconjunctivitis and eczema are different and therefore the changes in prevalence over time would vary in an inconsistent manner for each of these diseases, but rather supported the null hypothesis which stated that the three diseases would remain in the same relationship to each other. The finding that the relationship between the three diseases has been relatively consistent over the seven years is interesting and intriguing. It could be that the three diseases regulate themselves for prevalence and severity, and by coincidence have remained in the same relationship (we have only two time points, and only a 5–10 year period of observation). Alternatively the findings suggest that whatever factors underlie the changing prevalence of symptoms of the three diseases, they may be similar and may have been operating across the globe, in centres and countries with diverse economic and cultural environments, suggesting they are mainly determined by environmental rather than genetic factors. This is of particular interest, since it is now known that these diseases are linked not only through atopic processes but also by non-atopic processes, and the non-atopic processes are more influential in low and middle income countries.12,15,16 These results confirm the importance of further investigation of non-atopic factors.
As previously reported, the prevalence of symptoms more commonly increased than decreased over a seven-year period for each of the conditions. The relationship for the changes over time in the three diseases showed some variation. We would have predicted that correlations between symptoms of eczema and rhinoconjunctivitis which are more commonly regarded as atopic diseases would be stronger than those with asthma which is less commonly atopic. Within age groups we found this to be the case as judged by the correlation coefficients of centre level data. Furthermore, we would have predicted that these correlations would be stronger in the older than younger age group based on the assumption that asthma in younger children is more influenced by non-atopic factors, such as viral infections, than in older children. Again, this is supported by the correlation coefficients of centre level data where the relationship was weaker in the younger than the older age group.
No strong underlying patterns were found for analyses by gender, comparison of the two age-groups, or one combination of symptoms versus another combination or versus one symptom. The stronger relationship for changes over time in symptoms of rhinoconjunctivitis with eczema in the older rather than the younger age group suggests that these two diseases may have more commonality than with asthma, whereas previously the three diseases have been strongly linked in the literature17 which is based mainly on research in children from high income countries. Alternatively rhinoconjunctivitis and eczema symptoms may be more noticeable by adolescents than asthma symptoms, particularly in those with mild asthma symptoms.
In summary, in this worldwide study of centres in low to high income countries we have shown that little has changed in the inter-relationship of symptoms of asthma, rhinoconjunctivitis and eczema, despite changes in global prevalence.
Conflict of interestThe authors have no conflict of interest to declare.
We are grateful to the children and parents who participated in ISAAC Phase Three and the coordination and assistance by the school staff is sincerely appreciated. The authors also acknowledge and thank the many funding bodies throughout the world that supported the individual ISAAC centres and collaborators and their meetings. Currently the main source of funding for the ISAAC International Data Centre (IIDC) is Lottery Health Research New Zealand. Many New Zealand and international funding bodies have contributed support for the IIDC during the periods of fieldwork and data compilation (the BUPA Foundation, the Health Research Council of New Zealand, the Asthma and Respiratory Foundation of New Zealand, the Child Health Research Foundation, the Hawke's Bay Medical Research Foundation, the Waikato Medical Research Foundation, Glaxo Wellcome New Zealand, the Auckland Medical Research Foundation and Astra Zeneca New Zealand). Glaxo Wellcome International Medical Affairs supported the regional coordination for Phase Three and the IIDC. Without help from all of the above, ISAAC would not have been such a global success.
N. Aït-Khaled* (International Union Against Tuberculosis and Lung Disease (The Union), Cheraga, Algeria), H.R. Anderson (Division of Community Health Sciences, St George's, University of London and MRC Centre for Environment and Health, London, UK), M.I. Asher (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand), R. Beasley*, (Medical Research Institute of New Zealand, Wellington, New Zealand), B. Björkstén* (Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden), B. Brunekreef (Institute of Risk Assessment Science, Universiteit Utrecht, Netherlands), J. Crane (Wellington Asthma Research Group, Wellington School of Medicine, New Zealand), P. Ellwood (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand), C. Flohr (Dept of Paediatric Allergy & Dermatology, St John's Institute of Dermatology, London, UK), S. Foliaki* (Centre for Public Health Research, Massey University, Wellington, New Zealand), F. Forastiere (Department of Epidemiology, Rome E Health Authority, Rome, Italy), L. García-Marcos (Respiratory Medicine and Allergy Units, “Virgen de la Arrixaca” University Children's Hospital, University of Murcia, Spain), U. Keil* (Institut für Epidemiologie und Sozialmedizin, der Universität Münster, Germany), CKW Lai* (Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong SAR, China), J. Mallol* (Department of Respiratory Medicine, Hospital CRS El Pino, University of Santiago de Chile, Chile), E.A. Mitchell (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand), S. Montefort* (Department of Medicine, University of Malta, Malta), J. Odhiambo* (Centre for Respiratory Diseases Research, Kenya Medical Research Institute, Nairobi, Kenya), N. Pearce (Department of Medical Statistics, Faculty of Epidemiology and Public Health, London School of Hygiene and Tropical Medicine, London, UK), C.F. Robertson (Murdoch Children's Research Institute, Melbourne, Australia), A.W. Stewart (Epidemiology and Biostatistics, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand), D.P. Strachan (Division of Community Health Sciences, St George's, University of London, UK), E. von Mutius (Dr. von Haunersches University Children's Hospital, Ludwig-Maximilians University, München, Germany), S.K. Weiland† (Institute of Epidemiology, University of Ulm, Germany), G. Weinmayr (Institute of Epidemiology, University of Ulm, Germany), H.C. Williams (Centre for Evidence Based Dermatology, Queen's Medical Centre, University Hospital, Nottingham, UK), G. Wong (Department of Paediatrics, Prince of Wales Hospital, Hong Kong SAR, China). *Regional Coordinators. †Deceased 2007.
M.I. Asher, T.O. Clayton, E. Ellwood, P. Ellwood, E.A. Mitchell, Department of Paediatrics: Child and Youth Health, and A.W. Stewart, Epidemiology and Biostatistics, School of Population Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand.
Albania: A. Priftanji* (Tiranë); Algeria: B. Benhabylès (Wilaya of Algiers); Argentina: C.E. Baena-Cagnani* (Córdoba); Australia: C.F. Robertson* (Melbourne); Austria: G. Haidinger* (Kärnten, Urfahr-Umgebung); Barbados: M.E. Howitt* (Barbados); Belgium: J. Weyler (Antwerp); Brazil: G.B. Fischer (Porto Alegre), N. Rosário (Curitiba), D. Solé* (São Paulo), M. de Britto (Recife), L. de Freitas Souza (Salvador); Canada: D. Rennie (Saskatoon); Channel Islands: R. Goulding (Jersey), P. Standring (Guernsey); Chile: P. Aguilar (South Santiago), L. Amarales (Punta Arenas), M.A. Calvo (Valdivia); China: Y-Z. Chen* (Beijing), N-S. Zhong (Guangzhou); Costa Rica: M.E. Soto-Quirós* (Costa Rica); Estonia: M-A. Riikjärv* (Tallinn); Ethiopia: K. Melaku (Addis Ababa); Finland: J. Pekkanen* (Kuopio County); Georgia: M. Gotua* (Kutaisi); Germany: U. Keil* (Münster); Hong Kong SAR, China: Y.L. Lau (Hong Kong 6–7yr), G. Wong (Hong Kong 13–14yr); India: N.M. Hanumante (Pune), K.C. Jain (Jodhpur), M.K. Joshi (Mumbai (16)), V.A. Khatav (Borivali), L. Kumar (Chandigarh), A.V. Pherwani (Mumbai (18)), G. Setty (Chennai (3)), S.K. Sharma (New Delhi (7)), T.U. Sukumaran (Kottayam); Indonesia: C.B. Kartasasmita (Bandung); Iran: M-R. Masjedi* (Rasht, Tehran); Isle of Man: A. Steriu (Isle of Man); Italy: L. Bisanti (Milano), E. Bonci (Cosenza), E. Chellini (Firenze), G. Ciccone (Torino), F. Forastiere* (Roma), C. Galassi (Emilia-Romagna), M.G. Petronio (Empoli), S. Piffer (Trento), P. Sestini (Siena); Japan: H. Odajima (Fukuoka); Kenya: F.O. Esamai (Eldoret), L. Ng’ang’a* (Nairobi); Kuwait: J.A. al-Momen (Kuwait); Latvia: V. Svabe (Riga); Lithuania: J. Kudzyte* (Kaunas); Malaysia: B.S. Quah (Kota Bharu), K.H. Teh (Alor Setar), J. de Bruyne* (Klang Valley); Malta: S. Montefort* (Malta); Mexico: I. Romieu (Cuernavaca); Morocco: Z. Bouayad* (Casablanca, Marrakech); New Zealand: M.I. Asher* (Auckland), R. MacKay (Nelson), C. Moyes (Bay of Plenty), P. Pattemore (Christchurch), N. Pearce (Wellington); Nigeria: B.O. Onadeko (Ibadan); Pakistan: N. Mahmood* (Karachi); Panama: G. Cukier* (David-Panamá); Paraguay: J.A. Guggiari-Chase* (Asunción); Peru: P. Chiarella* (Lima); Philippines: F. Cua-Lim* (Metro Manila); Poland: A. Brêborowicz (Poznan), G. Lis* (Kraków); Portugal: R. Câmara (Funchal), J.M. Lopes dos Santos (Porto), C. Nunes (Portimao), J. Rosado Pinto* (Lisbon); Republic of Ireland: L. Clancy (Republic of Ireland); Romania: D. Deleanu* (Cluj); Russia: E.G. Kondiourina (Novosibirsk); Singapore: D.Y.T. Goh (Singapore); South Africa: H.J. Zar* (Cape Town); South Korea: H-B. Lee* (Provincial Korea, Seoul); Spain: A. Arnedo-Pena (Castellón), A. Blanco-Quirós (Valladolid), R.M. Busquets (Barcelona), G. García-Hernández (Madrid), L. García-Marcos* (Cartagena), C. González Díaz (Bilbao), F. Guillén-Grima (Pamplona), M.M. Morales Suárez-Varela (Valencia); Sultanate of Oman: O. Al-Rawas* (Al-Khod); Sweden: H. Vogt (Linköping); Taiwan: J-L. Huang* (Taipei); Thailand: M. Trakultivakorn (Chiang Mai), P. Vichyanond* (Bangkok); Tunisia: M. Jerray (Sousse); USA: G.J. Redding (Seattle); Ukraine: V. Ognev* (Kharkiv); United Kingdom: H.R. Anderson* (North Thames, South Thames), J.B. Austin (Scotland), M. Burr (Wales), M.H. Shamssain (Sunderland), D.P. Strachan (Surrey/Sussex); Uruguay: D. Holgado* (Montevideo). *National Coordinators.
M. Sears (Canada); H.R. Anderson (Channel Islands, Isle of Man); V. Aguirre (Chile); C.K.W. Lai (Hong Kong SAR, China); J. Shah (India); K. Baratawidjaja (Indonesia); S. Nishima (Japan); M. Baeza-Bacab (Mexico); P. Manning (Republic of Ireland); R.M. Khaitov (Russia); B-W. Lee (Singapore); L. Nilsson (Sweden).
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.aller.2011.11.004.