INTRODUCTION
Formaldehyde (HCHO) is a low molecular weight organic chemical. It has industrial applications in the manufacturing of plastics, rubber, resins, plywood, fabric coatings and adhesives. It is also used as a disinfecting, preserving, and embalming agent1.
Formaldehyde has been reported to cause acute and chronic health problems1. When formaldehyde is inhaled most of it is absorbed in the upper respiratory tract and relatively small amount reach the alveolar membranes of the lung2. Formaldehyde acts as a sensitizer at low concentrations and as a potent asthmagenic agent. Because of its' widespread use in industrial processes, it causes occupational asthma3. Here, we report a case due to accidental formaldehyde exposure with various effects on bronchial tree.
CASE REPORT
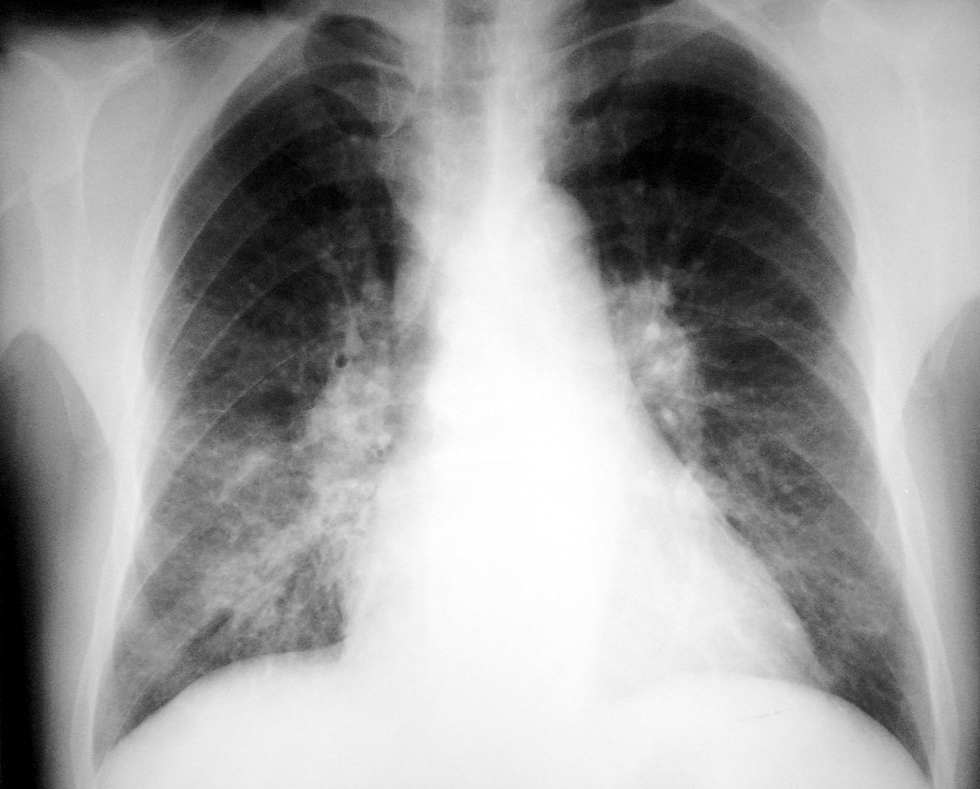
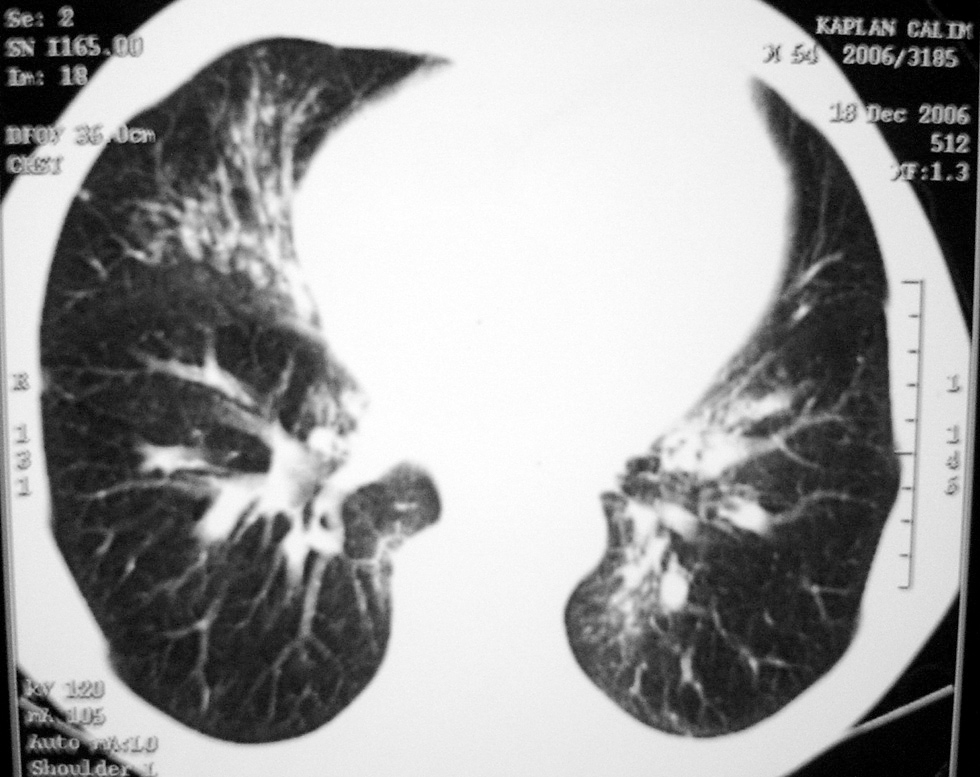
A 54-year-old male admitted to the department of internal medicine of university hospital. He was hospitalized with graves disease with no history of asthma/atopy. His initial pulmonary examination was normal, as well as normal spirometric test. He was an exsmoker with a 20 pack/year history of smoking. After ingestion of ~200 cc formaldehyde 10 % accidentally, he developed nausea, vomiting, and sore throat. Two days after the incident, he began complaining of cough, shortness of breath, wheezing and hemoptysis (10 cc/day). He was referred to the pulmonary department for the assessment of his chest symptoms. He had bronchospasm and bilateral infiltrates on CXR (fig. 1). Endoscopic examination revealed low grade oesophagitis/gastritis which was treated symptomatically with proton pump inhibitors and parenteral hydration as well. On the following day, he underwent a spirometric examination which showed a decreased FEV1 of 2.10L (69 %). Because he might have inhalated or asphyxiated formaldehyde while vomiting, a possible diagnosis of hypersensitivity and/or chemical pneumonitis was made with severe dyspnea, prevalent ronci, low FEV1 and bilateral infiltrates on CXR. After a week of treatment with systemic glucocorticosteroid and nebulised salbutamol, his symptoms disappeared, ronci relieved, FEV1 increased to 2.36L (77 %) and infiltrates were cleared. On the fourth day of prophylactic low MW heparin which was given for thrombus prophylaxis, he developed massive hemoptysis ~500 cc, 38.4 °C fever, leucocytes of 23600/mm3, prevalent crackles, severe bronchospasm, and new infiltrates on CXR. He had mild hypoxemia (PaO2:59 mmHg) and low carbon monoxide diffusion capacity (DLCO: 5.6L, 63 %). After bronchoscopic examination revealed intensive hemorrhagic mucosa predominantly at the right middle lobe and left lower lobe, heparin was sustained, antibiotic and combination therapy with inhaled steroid and salbutamol were started. Thoracic CT (fig. 2) demonstrated bilateral heterogeneous infiltrates which were consistent with the bronchoscopic findings. A week later, his symptoms and crackles were cleared, leukocyte count returned to normal values, re-bronchoscopic examination was normal, radiographic infiltrates were totally regressed, and FEV1 and DLCO were found to be within normal limits (3.09L, 100 % and 6.3L, 71 %, respectively). Allergologic investigations provided as follows: total and formaldehyde specific immunoglobulin E (IgE) were normal, skin prick tests to common aeroallergens were negative, patch tests with the Standard European Panel were positive to formaldehyde.
Figure 1.--Bilateral reticulary infiltrates at the lower zones on CXR.
Figure 2.--Bilateral heterogeneous infiltrates on the thoracic CT.
DISCUSSION
Although there is an increasing interest to formaldehyde exposure because of its' high levels in occupational settings, occupational asthma occurs in sporadic cases. There is a latent period, which extends from weeks to years before symptoms begin. Reactions are then provocated by concentrations that were previously well tolerated and that have little effect on the majority of fellow workers.
Asthma induced by formaldehyde can be diagnosed by non-specific or specific bronchial provocation challenge4, but it was found to be difficult to maintain a constant concentration or to determine the atmospheric end-target concentration of formaldehyde inhalation. A closed-circuit apparatus to generate formaldehyde as a vapour was introduced by Lemiere et al5. Non-irritant concentrations of formaldehyde can be obtained by these apparatus but they are not standardised and therefore not useful for the clinical practice. Kim et al showed that environmental assessment as the mean level of formaldehyde was 0.06 ppm in the working area, but it was considered that the mean exposure level had been much higher when their patient suffered asthmatic attacks in workplace3. There was some discrepancy between the formaldehyde concentrations which induced asthmatic reactions in the workplace challenge and in the specific challenge tests. A lower concentration of formaldehyde was enough to induce asthma in the work place. Our patient demonstrated asthmatic attack as well as alveolitis and pneumonitis with direct bronchial contact to high concentration of formaldehyde for a short duration of exposure. However, in this case there was no need for a provocation test, because our patient had the specific inhalation challenge accidentally. It is expected to see either a neutrophilic response or an exacerbation of pre-existent eosinophilic airways inflammation4. A neutrophilic response in bronchial secretions in this case was consistent with the literature.
The mechanism of formaldehyde induced asthma is not clear. Bronchoconstriction and airway symptoms can be explained by magnified acute airway inflammatory responses with its irritant effect on the upper airways. Immunological hypersensitivity and development of IgE to formaldehyde was proved in some studies4. Casset et al showed that low levels of formaldehyde significantly enhanced bronchial responsiveness to mite allergen in sensitized subjects with asthma6. In this case; IgE mediated hypersensitivity was ruled out with negative skin prick tests and specific IgE. A weak reaction to formaldehyde in the patch test was found to be related with delayed hypersensitivity to formaldehyde and which be an explanation of the chest symptoms occurred 48 hours after the incident.
In conclusion this is the first case of formaldehyde induced asthma different from the occupational exposure. It is most probable that the patient had inhaled formaldehyde 10 % while vomiting and specific bronchial hyperresponsiveness occurred, as well as focal alveolitis and bronchiolitis. Asthmatic findings found after three days of exposure was a typical of formaldehyde induced late reaction and responded well to glucocorticosteroids. It is known that more than 95 % of inhaled formaldehyde is absorbed in the upper respiratory tract and comparatively small amount reach the alveolar membranes2. Pneumonitis in this case may also be explained by the asphyxia of formaldehyde and haemoptysis was seen as a result of alveolitis and tracheabrochiolitis.
Outcome of the formaldehyde-induced asthma is often poor, and duration of exposure, severity of asthma and the pulmonary functions before the exposure are the prognostic determinants3. Two months after the accident, our patient still had expectoration of mucus.
This data suggests that the direct and indirect effects of formaldehyde may occur in healthy human airways, whereas mild asthmatic response and pneumonitis can be seen simultaneously in the same patient due to accidental exposure. Therefore, pulmonologists should be aware of the possibility of the reactions to formaldehyde not only in occupational settings, but also in many other fields.
Correspondence:
A. Baccioglu
Kirikkale University. School of Medicine
Department of Allergic Diseases
71300 Kirikkale. Turkey
TEL: + 90 318 225 24 85/119
FAX: + 90 318 225 24 82
E-mail: ayshe_dr@yahoo.com