Allergic disease is a common cause of morbidity, particularly in young children, and its prevalence has increased in the last 20 years in most countries; and food allergy is the most common cause of allergy in the first years of life. Apparently diet has an important influence in a lot of physiological functions during pregnancy and childhood. Infants are exposed to allergens which are being eaten by the mother and go across placenta,1 and due to their intestinal immaturity can absorb proteins with high molecular weight that have a lot of allergenicity. This early exposure has an effect in humoral response and can curb the development of tolerance.2
Food hypersensitivity is associated with the presence of atopic dermatitis, gastrointestinal diseases and asthma. Various authors have found a high prevalence of food sensitisation in infants with atopic dermatitis3,4 and Aboudiab et al. determined that cow's milk proteins suppression could improve the symptoms of children with asthma and cow's milk hypersensitivity.5
In a recent review by the Cochrane Group they concluded that the use of hydrolysed formulas and other measures in infants with a high risk of atopy could reduce the risk of asthma in the first year of life.6 Other studies have shown that food hypersensitivity in the first years of life can promote the development of allergy against inhalant allergens.7,8
The aim of our retrospective descriptive and cases-controls study was to describe the characteristics of children with food allergy in Príncipe de Asturias Hospital, in Madrid, Spain and to determine the relationship between food allergy and the development of asthma and other signs of atopy.
Two hundred and fifty medical records of infants with cow's milk and egg challenge, between 1993 and 2003, were reviewed. The principal variables were sex; age at beginning of symptoms; symptoms of food allergy; skin prick test (SPT) and allergen-specific IgE antibody measurement; age at challenge and age of becoming tolerant. IgE-mediated hypersensitivity was determined by SPT and measurements of specific immunoglobulin E (IgE) in serum, taken at time of diagnosis of food hypersensitivity.
A telephone survey was done to 68 patient's parents. The rest of the patients were not located. All ages were between 3 and 17 (mean value 6.1). They were asked about persistence of allergy, development of asthma, atopy, medicine allergy, where they do the follow-up and how much they think allergy affects their quality of life (on a scale from 1–100, with one representing the smallest impact and 100 the highest impact). Parents of these 68 subjects agreed to participate in the study.
Results were compared to a group of healthy children, between 3 and 17 years old (mean value 7.1); 33 of whom were recruited from a school and 26 from three health care centres of the Area 3 in Madrid. Participation was voluntary, confidential and anonymous. The exclusion criterion was a record of food hypersensitivity. Data were obtained in accordance with the Data Protection Law (15/1999).
Numerical variables were expressed either as means and standard deviations (sd), or median and interquartile range (IQR). Qualitative variables were presented as frequencies and percentages. For comparison of qualitative variables, Chi2 analyses and Fisher's exact test were used. A p<0.05 significance level was chosen. The SPSS 15 software was used for statistical calculations.
One hundred and ninety-nine (77%) children were challenged to milk and 60 (23%) to egg. Symptoms of allergy started by the mean age of 5.4 months (±5.56 sd); 3 (±2 sd) months in children with cow's milk allergy (CMA) and 13.5 (±7.1 sd) in children with egg allergy. Skin symptoms and gastrointestinal symptoms were the most common symptoms in these children (Table 1).
Symptoms of food hypersensitivity
| Skin symptoms | Gastrointestinal symptoms | Respiratory symptoms | Anaphylaxis | Other symptoms | |
| Children challenged to cow's milk (n=199) | 154 (78.2%) | 83 (42%) | 5 (2.5%) | 1 (0.5%) | 26 (13.2%) |
| Children challenged to egg (n=60) | 46 (79.3%) | 15 (25.9%) | 6 (10.3%) | 1 (1.7%) | 5 (8.6%) |
Diagnosis of food allergy was done by the median age of 6 months (IQR 6.63). By groups, children with CMA were diagnosed at the median age of 5 months and children with egg allergy at 16 months. The first challenge was carried out by the median age of 14 months (IQR 23).
At the median age of 13 months (IQR 16), 92% of the subjects challenged to milk became tolerant and at the median age of 46 months (IQR 32), 85% of the children challenged to egg also became tolerant.
Thirty-three (17%) of the children challenged to milk had egg hypersensitivity and 11 (6%) had other food hypersensitivity. Eighteen (30%) of the children challenged to egg had cow's milk hypersensitivity and 14 (23%) had other food hypersensitivity.
SPT was positive in 92 (43%) children with CMA and in 56 (12%) children with egg allergy. Specific IgE was >0.35KU/L in 76 (36%) children with CMA and 57(63%) children with egg allergy.
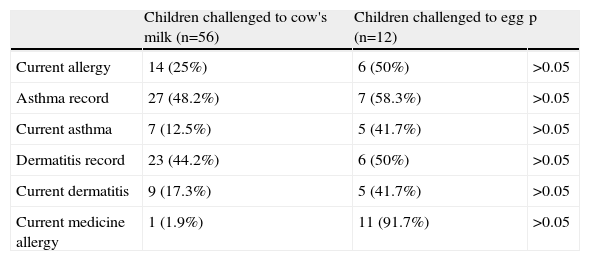
We determined the proportion of children who did not become tolerant or developed other allergy (Table 2). The proportion of children with asthma and symptoms of atopy is higher in children with egg hypersensitivity. We also found that 90% of the children with allergy had food hypersensitivity and 21% inhalant hypersensitivity.
Children who did not become tolerant or developed other allergy
| Children challenged to cow's milk (n=56) | Children challenged to egg (n=12) | p | |
| Current allergy | 14 (25%) | 6 (50%) | >0.05 |
| Asthma record | 27 (48.2%) | 7 (58.3%) | >0.05 |
| Current asthma | 7 (12.5%) | 5 (41.7%) | >0.05 |
| Dermatitis record | 23 (44.2%) | 6 (50%) | >0.05 |
| Current dermatitis | 9 (17.3%) | 5 (41.7%) | >0.05 |
| Current medicine allergy | 1 (1.9%) | 11 (91.7%) | >0.05 |
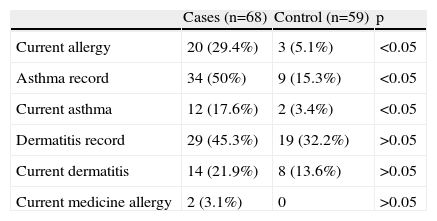
When we compared cases to controls, the proportion of persistent allergy and asthma was higher in cases than in controls (Table 3). Sixty-two percent and 32% of the children with food hypersensitivity and without food hypersensitivity respectively had relatives with allergic diseases.
Allergic diseases in cases (children with food hypersensitivity) and controls (survey results)*
| Cases (n=68) | Control (n=59) | p | |
| Current allergy | 20 (29.4%) | 3 (5.1%) | <0.05 |
| Asthma record | 34 (50%) | 9 (15.3%) | <0.05 |
| Current asthma | 12 (17.6%) | 2 (3.4%) | <0.05 |
| Dermatitis record | 29 (45.3%) | 19 (32.2%) | >0.05 |
| Current dermatitis | 14 (21.9%) | 8 (13.6%) | >0.05 |
| Current medicine allergy | 2 (3.1%) | 0 | >0.05 |
We conclude that, in our hospital, the majority of the children with food hypersensitivity have CMA and skin symptoms. However children with cow's milk hypersensitivity become more tolerant than children with egg hypersensitivity.
We have shown that egg hypersensitivity is related to IgE-mediated allergy in more cases than CMA. Moreover this result could be related to a later development of atopic symptoms.
When we compared children with food hypersensitivity and children without it, we found that the first group can develop asthma and other allergies as inhalant allergy more frequently than the second group, and that their relatives have more allergic diseases.
Our beliefs regarding the burden of this disease have been confirmed with the data from the survey. Parents think allergy affects their child's quality of life in a proportion of 50% and we should, as paediatricians, try to detect these children and teach them different measures in order to improve their quality of life.