To compare the activity the Urology Department of a Portuguese Academic Hospital during the state of emergency and the equivalent period at the previous year. We compared the number of elective consultations and diagnostic urologic examinations, number and type of elective surgeries, as well as patients’ demographic characteristics and main causes of presentation to Urology Emergency Department (ED) during the two mentioned periods.
Materials and methodsData from 691 patients coming to emergency department were collected from institutional clinical software from March 18th 2020 to May 2nd 2020—and from the same period the previous year. Data collected were age, sex, day of the presentation to Emergency Department, referral from other hospitals, triage color, reason of admission, diagnosis of discharge, and the need for emergency surgery or hospitalization. In order to identify associations between demographic and clinical variables with having been submitted to an emergency surgery (outcome), logistic regression models were applied.
ResultsMultivariable analysis showed an association of sex with being submitted to surgery, 65.6% decrease in the odds for the male gender. The period (COVID versus non-COVID) did not show a significant association with surgery.
ConclusionOur department experienced an noticeable activity reduction. We also observe a reduction in urgent causes to attend the ED considered less serious. The percentage of cases requiring emergency surgery and hospitalization was higher during COVID-period.
Comparar la actividad del Servicio de Urología de un Hospital Universitario Portugués durante el estado de alarma y el período equivalente del año anterior. Comparamos el número de consultas electivas y pruebas diagnósticas urológicas, el número y el tipo de cirugías electivas, así como las características demográficas de los pacientes y los principales causas de ingreso al Servicio de Urgencias (SU) de Urología durante los dos períodos mencionados.
Materiales y métodosLos datos de 691 pacientes que acudieron a urgencias desde el 18 de marzo de 2020 hasta el 2 de mayo de 2020—y del mismo período del año anterior-se recogieron del software medico institucional. Los datos recopilados fueron edad, sexo, fecha de visita al servicio de urgencias, derivación desde otros hospitales, color del triaje, causa del ingreso, diagnóstico al alta y la necesidad de cirugía de urgencia u hospitalización. Con la intención de identificar las asociaciones entre las variables demográficas y clínicas con el hecho de haber sido sometido a una cirugía de urgencia (variable), se aplicaron modelos de regresión logística.
ResultadosEl análisis multivariante mostró asociación entre el sexo del paciente con el hecho de ser sometido a una cirugía, con una disminución del 65,6% en las probabilidades para el género masculino. El período (COVID versus sin-COVID) no mostró una asociación significativa con la cirugía.
ConclusiónNuestro departamento experimentó una reducción importante en la actividad. También observamos una reducción de las causas urgentes para acudir a los servicios de urgencias considerados menos graves. El porcentaje de casos que requirieron cirugía de urgencia y hospitalización fue mayor durante el período COVID.
The outbreak of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2)1 has spread globally and was declared a worldwide pandemic by the World Health Organization on the 11th March 2020.2 After spreading in the Hubei region in China, the SARS-CoV-2 reached several different countries.
Portugal had the first cases reported on March 2nd, 2020, causing the Government to declare the state of emergency several days after, by March 18th. Due to the increase amount of cases, the state of emergency was renewed on April 2nd and finished on May 2nd.
Central Lisbon University Hospital Centre (CHULC) was identified as one of COVID-19 referral centers, where some of the existing Intensive Care Units were exclusively dedicated to patients with this virus. Some new medical wards were also created with the aim of hospitalizing less severe COVID-19 patients.
One of the objectives of this study was to compare the activity of the Urology Department of a Portuguese Academic Hospital – CHULC, during the state of emergency and the equivalent period at the previous year. The present study compared the number of elective consultations and diagnostic urologic examinations, number and type of elective surgeries, as well as patients’ demographic characteristics and main causes of presentation to Urology Emergency Department (ED) during the two mentioned periods. This study still aimed to explore, in a multivariable context, which demographic and clinical characteristics of the patients could be associated with having been submitted to emergency surgery considering these two different periods.
Materials and methodsData were collected from institutional clinical software from March 18th 2020 to May 2nd 2020—and from the same period the previous year (from March 18th 2019 to May 2nd 2019). The Urology emergency ward of CHULC runs every day, 24 h a day, including bank holidays and weekends. Data collected were age, sex, day of the presentation to ED, referral from other hospitals, triage color, reason of admission, diagnosis of discharge, and the need for emergency surgery or hospitalization. The triage at this hospital is done according to the Manchester Triage System (MTS),3 which classifies patients into five degrees of urgency (red, orange, yellow, green, blue), with red patients requiring immediate observation and blue patients considered non-urgent.
To understand how the elective activity changes during the state of emergency in our Urology Department, we also analyzed the number of elective consultations, diagnostic urologic examinations as well as the type of elective surgeries. The elective activity occurs on the weekdays, from 8:00 am to 3:00 pm.
We regrouped the reason of admission, the diagnosis of discharge, as well as the hospitals that referrer to our center into a lower number of groups, in order to make the results easier to read. Concerning the reason of admission, three groups were created. For group 1 we included: dysuria, hematuria and urinary retention; for group 2: abdominal pain and lumbar plain; and for group 3: penile pain, testicular pain, and others where we consider other minor causes of searching urological care such as genital pruritus, dermatological conditions, among others isolated causes. Regarding the diagnosis of discharge, we classified them into four groups. In group 1 we considered: testicular trauma, urethral stricture, hydrocele, and orchiepidymitis; in group 2: prostatitis, uncomplicated urinary tract infection, benign prostate hyperplasia and hypoactive bladder; in group 3: hydronephrosis with acute kidney injury, pyelonephritis, pyonephrosis, prostate cancer, and kidney tumor; and in group 4: renal colic, unknow, others and bladder tumor.
With respect to hospitals referrals we divided it into three groups, namely group 0: not referred from other hospitals; group 1: Barreiro, Garcia Orta, Setubal; group 2: Beja; Évora; Litoral Alentejano, Portalegre; and group 3: Vila Franca de Xira, Private Hospitals, Santarém and others.
Continuous variables were expressed as median and inter-quartile range (IQR: P25–P75) and categorical variables as frequencies (percentages). Nonparametric Chi-Square, Fisher’s exact and Mann-Whitney tests were used to compare the two periods (2019 versus 2020), as appropriate. Additionally, to identify associations between demographic and clinical variables with having been submitted to an emergency surgery (outcome), logistic regression models were applied. In the univariable analysis, all the variables that attained a P-value ≤.25 were considered for the multivariable model. Crude and adjusted odds ratios were estimated (OR) with corresponding 95% confidence intervals.
The level of significance α = 0.05 was considered. All data were analyzed using the Statistical Package for the Social Sciences for Windows 25.0 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp.)
ResultsOn a 46-day period, the Urology Department performed 2739 (23.1% from all elective hospital consultations) and 2770 (31.3% from all elective hospital consultations) elective consultations in 2019 and 2020, respectively. In 2019 all the consultations were presential, and in 2020 virtually all of them were teleconsultation. The total number of elective appointments in CHULC, including Urology, was 11,868 in non-COVID period and 8860 in COVID-period. There is an evidence of a statistically difference between the incidence of the number of consultations in 2019 and 2020 (P < .001).
Regarding complementary diagnostic tests, we have performed 563 exams in non-COVID period and 107 in the emergency state in 2020, which represents a decrease in 81% of the total number of exams. Comparing the COVID-period with the homologous period of time, one year ago, we have not done any Urodynamic Studies (0 vs. 88), any Penile Doppler (0 vs. 11), and any Brachytherapy (0 vs. 3). Adding to this, there were a considerable reduction in the absolute number of prostate biopsies (14 vs. 52), cystoscopies (67 vs. 189), uroflowmetries (2 vs. 169), nephrostomy catheter replacement (5 vs. 8) and stent extraction (17 vs. 37).
However, considering corresponding percentages regarding the total number of complementary diagnostic tests previously reported in each year, there was an increase in the prostate biopsies (13.1% vs. 9.2%, P = .221), stent extraction (15.9% vs. 6.6%, P = .001) and nephrostomy catheter replacement (4.7% vs. 1.4%, P = .042), and a considerable reduction of cystoscopies (33.6% vs. 62.6%, P < .001) and uroflowmetries (1.9% vs. 30.0%, P < .001).
Similarly, in the same timeframe the total number of elective surgeries was reduced from 77.6% (177/228) in 2019 to 63.2% (79/125) in 2020, while the percentage of urgent surgery has increased from 22.4% (51/228) in 2019 to 36.8% (46/125) in 2020 (P = .004). On the other hand, we have performed 52 (29.4%) oncologic surgeries in 2019 and 60 (75.9%) in 2020, being the remaining 125 (70.6%) non-oncologic surgeries in 2019 and 19 (24.1%) in 2020 (P < .001).
During the state of emergency, on the aforementioned dates, the total number of ED admissions for any cause was reduced from 18,468 in 2019 to 9098 in 2020. Regarding Urology ED, 434 (2.4% from the total) visited our service in the referred period in 2019 and 257 (2.8% from the total) in the state of emergency time in 2020 (P = .018).
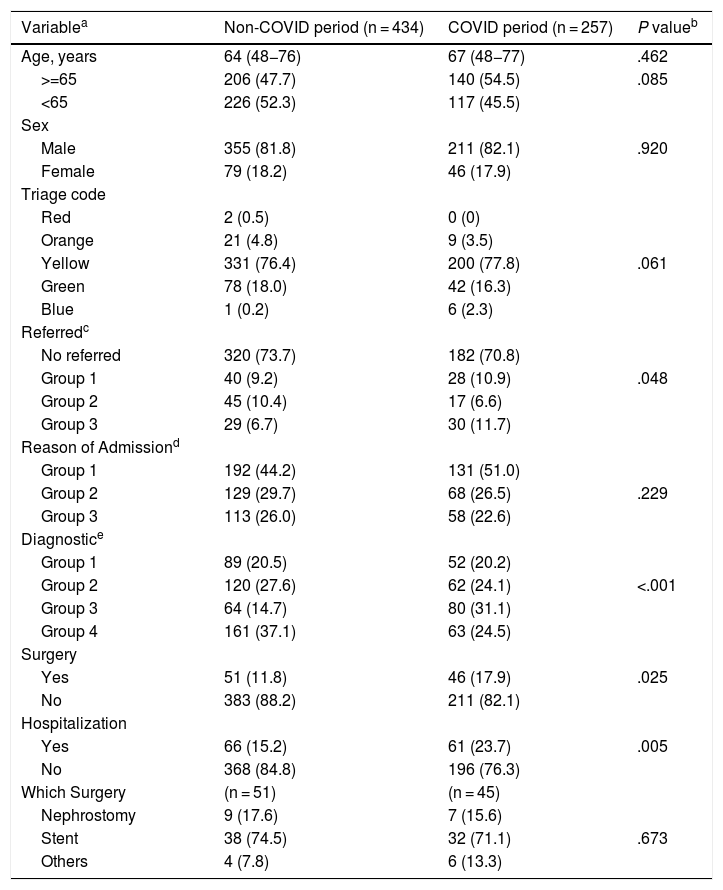
Table 1 summarizes the characteristics of the patients, based on each time frame. Accordingly, with respect to the clinical severity grade under the MTS, comparing the non-COVID period with COVID-period, 0.5% vs. 0% corresponded to the red bracelet, 4.8% vs. 3.5% of patients to the orange bracelet, 76.4% vs. 77.8% to the yellow bracelet, 18.0% vs. 16.3% to the green bracelet and 0.2% vs. 2.3% to the blue bracelet, respectively (P = .061). Nevertheless, no significant differences were noticed between urgent or very urgent cases (yellow, orange or red bracelet) vs. non-urgent cases (green or blue bracelet) in both groups (P = .887).
Characteristics of Urology ED Patients.
| Variablea | Non-COVID period (n = 434) | COVID period (n = 257) | P valueb |
|---|---|---|---|
| Age, years | 64 (48−76) | 67 (48−77) | .462 |
| >=65 | 206 (47.7) | 140 (54.5) | .085 |
| <65 | 226 (52.3) | 117 (45.5) | |
| Sex | |||
| Male | 355 (81.8) | 211 (82.1) | .920 |
| Female | 79 (18.2) | 46 (17.9) | |
| Triage code | |||
| Red | 2 (0.5) | 0 (0) | |
| Orange | 21 (4.8) | 9 (3.5) | |
| Yellow | 331 (76.4) | 200 (77.8) | .061 |
| Green | 78 (18.0) | 42 (16.3) | |
| Blue | 1 (0.2) | 6 (2.3) | |
| Referredc | |||
| No referred | 320 (73.7) | 182 (70.8) | |
| Group 1 | 40 (9.2) | 28 (10.9) | .048 |
| Group 2 | 45 (10.4) | 17 (6.6) | |
| Group 3 | 29 (6.7) | 30 (11.7) | |
| Reason of Admissiond | |||
| Group 1 | 192 (44.2) | 131 (51.0) | |
| Group 2 | 129 (29.7) | 68 (26.5) | .229 |
| Group 3 | 113 (26.0) | 58 (22.6) | |
| Diagnostice | |||
| Group 1 | 89 (20.5) | 52 (20.2) | |
| Group 2 | 120 (27.6) | 62 (24.1) | <.001 |
| Group 3 | 64 (14.7) | 80 (31.1) | |
| Group 4 | 161 (37.1) | 63 (24.5) | |
| Surgery | |||
| Yes | 51 (11.8) | 46 (17.9) | .025 |
| No | 383 (88.2) | 211 (82.1) | |
| Hospitalization | |||
| Yes | 66 (15.2) | 61 (23.7) | .005 |
| No | 368 (84.8) | 196 (76.3) | |
| Which Surgery | (n = 51) | (n = 45) | |
| Nephrostomy | 9 (17.6) | 7 (15.6) | |
| Stent | 38 (74.5) | 32 (71.1) | .673 |
| Others | 4 (7.8) | 6 (13.3) |
Group 0: not referred from other hospitals; group 1: Barreiro, Garcia Orta, Setubal; group 2: Beja; Évora; Litoral Alentejano, Portalegre; group 3: Vila Franca de Xira, Private Hospitals, Santarém and others.
Group 1: dysuria, hematuria and urinary retention; group 2: abdominal pain and lumbar plain; for group 3: penile pain, testicular pain and others.
Group 1: testicular trauma, urethral stricture, hydrocele, and orchiepidymitis; group 2: prostatitis, uncomplicated urinary tract infection, benign prostate hyperplasia and hypoactive bladder; group 3: hydronephrosis with acute kidney injury, pyelonephritis, pyonephrosis, prostate cancer, and kidney tumor; group 4: renal colic, unknow, others and bladder tumour.
Between the two period, there was no significant difference of the median age (67 vs. 64 years, P = .462). There was a higher number of older patients (with 65 years old or above) during the COVID period but also without statistically significance (54.5% vs. 47.7%, P = .085). In what concerns sex, there was no statistically significant difference between the two periods (P = .920).
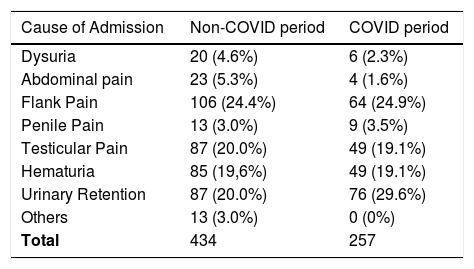
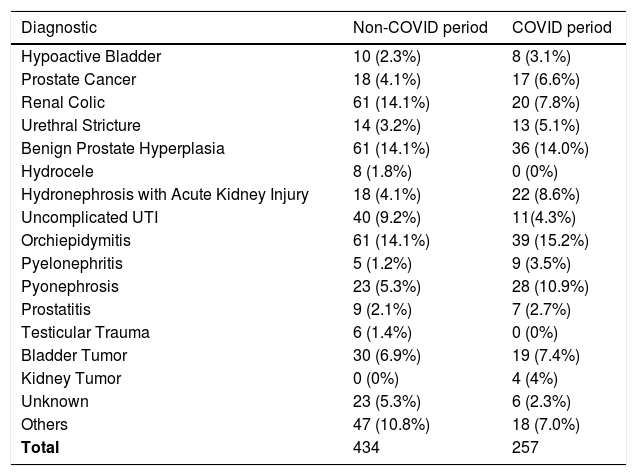
Regarding the three groups of causes of admission (Table 1), there were no significant differences between the two periods (P = .229). See Table 2 for more detailed data regarding causes of admission. Nevertheless, there were different diagnostics of discharge, with almost one third (31.1%) presenting in the most severe group (group 3), which includes hydronephrosis with acute kidney injury, pyelonephritis, pyonephrosis, prostate cancer, and kidney tumor, compared to 14.7% of the last year (P < .001). There were a decrease of approximately 50% in the renal colic and uncomplicated urinary tract infections (UTI) in COVID time (14.1% vs. 7.8%) and (9.2% vs. 4.3%) respectively, but there were a considerable increase in hydronephrosis with acute kidney injury (4.1% vs. 8.6%) and pyonephrosis (5.3% vs. 10.9%) (Table 3).
Cause of Admission of Urology ED patients.
| Cause of Admission | Non-COVID period | COVID period |
|---|---|---|
| Dysuria | 20 (4.6%) | 6 (2.3%) |
| Abdominal pain | 23 (5.3%) | 4 (1.6%) |
| Flank Pain | 106 (24.4%) | 64 (24.9%) |
| Penile Pain | 13 (3.0%) | 9 (3.5%) |
| Testicular Pain | 87 (20.0%) | 49 (19.1%) |
| Hematuria | 85 (19,6%) | 49 (19.1%) |
| Urinary Retention | 87 (20.0%) | 76 (29.6%) |
| Others | 13 (3.0%) | 0 (0%) |
| Total | 434 | 257 |
ED, Emergency Department.
Diagnostic of Urology ED patients.
| Diagnostic | Non-COVID period | COVID period |
|---|---|---|
| Hypoactive Bladder | 10 (2.3%) | 8 (3.1%) |
| Prostate Cancer | 18 (4.1%) | 17 (6.6%) |
| Renal Colic | 61 (14.1%) | 20 (7.8%) |
| Urethral Stricture | 14 (3.2%) | 13 (5.1%) |
| Benign Prostate Hyperplasia | 61 (14.1%) | 36 (14.0%) |
| Hydrocele | 8 (1.8%) | 0 (0%) |
| Hydronephrosis with Acute Kidney Injury | 18 (4.1%) | 22 (8.6%) |
| Uncomplicated UTI | 40 (9.2%) | 11(4.3%) |
| Orchiepidymitis | 61 (14.1%) | 39 (15.2%) |
| Pyelonephritis | 5 (1.2%) | 9 (3.5%) |
| Pyonephrosis | 23 (5.3%) | 28 (10.9%) |
| Prostatitis | 9 (2.1%) | 7 (2.7%) |
| Testicular Trauma | 6 (1.4%) | 0 (0%) |
| Bladder Tumor | 30 (6.9%) | 19 (7.4%) |
| Kidney Tumor | 0 (0%) | 4 (4%) |
| Unknown | 23 (5.3%) | 6 (2.3%) |
| Others | 47 (10.8%) | 18 (7.0%) |
| Total | 434 | 257 |
ED, Emergency Department; UTI, Urinary tract infections.
During the period analyzed in 2019, the percentage of patients who required emergency surgery and hospitalization was 11.8% and 15.2%, respectively. At the corresponding period in 2020, 17.9% required emergency surgery (P = .025) and 23.7% needed hospitalization (P = .005) (Table 1).
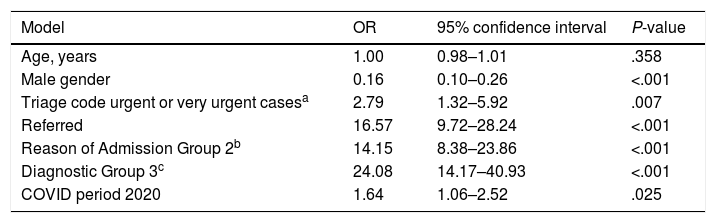
Univariable analysis results for the outcome (to have been submitted to surgery) are presented in Table 4. Results of the multivariable analysis showed an association of sex with being submitted to surgery, with a 65.6% decrease in the odds for the male gender (OR = 0.34; 95% CI: 0.17−0.70; P = .003). Also, patients coming from other hospitals had a ten-fold increase in the odds of surgery (OR = 10.57; 95% CI: 5.52–20.26; P < .001), and belonging to diagnostic group 3 is associated with a nine-fold increase in the same odds when compared with diagnostic group 1, 2 or 4 patients (OR = 9.85; 95% CI: 5.06–19.17; P < .001). Regarding the reasons for consultation, patients with backache or with abdominal pain (group 2) had almost a four-fold increase in the odds of being submitted to surgery when comparing with the remaining groups of reasons (OR = 3.60; 95% CI: 1.84–7.05; P < .001).
Results of univariable regression analysis – outcome: to have been submitted to surgery.
| Model | OR | 95% confidence interval | P-value |
|---|---|---|---|
| Age, years | 1.00 | 0.98–1.01 | .358 |
| Male gender | 0.16 | 0.10–0.26 | <.001 |
| Triage code urgent or very urgent casesa | 2.79 | 1.32–5.92 | .007 |
| Referred | 16.57 | 9.72–28.24 | <.001 |
| Reason of Admission Group 2b | 14.15 | 8.38–23.86 | <.001 |
| Diagnostic Group 3c | 24.08 | 14.17–40.93 | <.001 |
| COVID period 2020 | 1.64 | 1.06–2.52 | .025 |
Abbreviations: COVID, coronavirus disease; OR, odds ratio estimate; P-values were obtained by logistic regression models.
Reference categories: female gender, non-urgent cases (green or blue bracelet), non-referred, reason of admission: Group 1 (dysuria, hematuria and urinary retention) + Group 3 (penile pain, testicular pain and others), Diagnostic: Group 1 (testicular trauma, urethral stricture, hydrocele, and orchiepididymitis) + Group 2 (prostatitis, uncomplicated urinary tract infection, benign prostate hyperplasia and hypoactive bladder) + Group 4 (renal colic, unknow, others and bladder); non-COVID period 2019.
The period (COVID versus non-COVID) did not show a significant association with surgery (OR = 1.04; 95% CI: 0.54–2.02; P = .905).
DiscussionThe COVID 19 pandemic resulted in an international health emergency crisis, forcing a rapid and targeted response to the disease, apparently leaving other assistance areas on standby, reduced to minimal and urgent procedures.4 The consequences of this strategic option in terms of patient health are unknown.
As expected, the Urology Department experienced an noticeable reduction, in elective surgeries, diagnostic urologic examinations, as well as in the number of patients who attended the Urology Emergency Department, as already reported by others.5,6
All the planned surgical procedures and complementary exams have been progressively reduced in our institution during the crisis. Within the period analyzed in our study, there was a reduction of ED global accesses in CHULC (−9370), and Urology ED was not an exception (−177). In the same period, elective surgical activity performed in our Department experienced 55% reduction, compared to last year, diagnostic tests had an 81% decrease, while the number of elective urological consultations were 2% higher. This minimal increase in the number of consultations is due to the fact that we transformed all in person consultations into telephonic consultations, we did not cancel appointments during COVID-period and doctors, including urologists, were not allowed to go on vacation, so the department had the entire team working. When we needed the patient in person, we scheduled a face-to-face appointment.
Furthermore, in our sample, we were able to observe a reduction in urgent causes to attend the ED considered less serious, such as non-complicated UTI or renal colic, as also pointed out by Madanelo et al.5 Probably, a significant proportion of this reduction is due to the fact that some of the patients with mild and nonurgent conditions were afraid to attend the ED because of the pandemic. Additionally, the percentage of cases requiring emergency surgery and hospitalization, such as pyonephrosis, or hydronephrosis with acute kidney injury, was higher during COVID-period.
In this context, there is a shared view in Portugal that ED access may be frequently misused by patients, that might take advantage of a 24 h service in order to address conditions that are non-urgent and could be treated electively. Therefore, this number of patients is expectable to be mitigated during the pandemic.
Besides that, the association of sex with having been submitted to surgery, may be due to the fact that women are more apprehensive about viral transmission, addressing the urgency in more serious cases. In addition, patients from other hospitals also had a tenfold increase in the odds of surgery, as they were already evaluated by a doctor who suspected conditions that had to be urgently evaluated by a urologist.
COVID versus non-COVID did not show a significant association with surgery. It means that there are many other factors that cause patients to be operated, and not the fact that we are in COVID or non-COVID period. It leads us to believe that, during the pandemic period, despite all the constraints, we managed to maintain a similar quality of health care in the emergency department.
This study has a limitation concerning the causes for ED attendance because these were collected based on the medical records and not following a pre-established coding, which can interfere with the data presented.
On the other hand, despite being a recent and still ongoing situation, a complete period of time was analyzed, the state of emergency, with an acceptable number of patients, which we believe is representative of an extensive area of Portugal as CHULC is a tertiary central hospital covering the major part of Portuguese south territory.7
ConclusionsIn conclusion, the experience in a Urologic Department of a tertiary center during the COVID-19 pandemic demonstrated how Urologic activities, specially ED could be seriously affected. After the emergency state, new challenges are waiting at the urologic community namely longer waiting lists and the high risk of recurrence of the COVID-19 infection, and possibly limited healthcare resources.
FundingNo funding.
Conflict of interestNothing to declare.
Please cite this article as: Bernardino R, Gil M, Andrade V, Severo L, Alves M, Papoila AL, et al. Los cambios producidos durante el estado de alarma debido a la COVID-19 en un Servicio de Urología de un Hospital Universitario Terciario en Portugal. Actas Urol Esp. 2020;44:604–610.