To evaluate health-related quality of life (HRQOL) six years post-radical cystectomy in patients with muscle-invasive bladder cancer, comparing orthotopic ileal neobladder (ONB) and ileal conduit (IC). Therefore, the study aims to analyze the under-investigated long-term impact of standard bladder cancer treatments on HRQOL and provide insights into the HRQOL differences associated with these two common urinary diversion methods.
Patients and methodsThis prospective study included 39 patients with urothelial carcinoma treated with ONB or IC at our center between 03/2013 and 01/2023. Patients with variant histology, metastasis, neoadjuvant chemotherapy, or benign indications for cystectomy were excluded. HRQOL was assessed using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 questionnaire preoperatively, at four and six years postoperatively. Statistical analyses included Chi-square tests, T-tests, and logistic regression models.
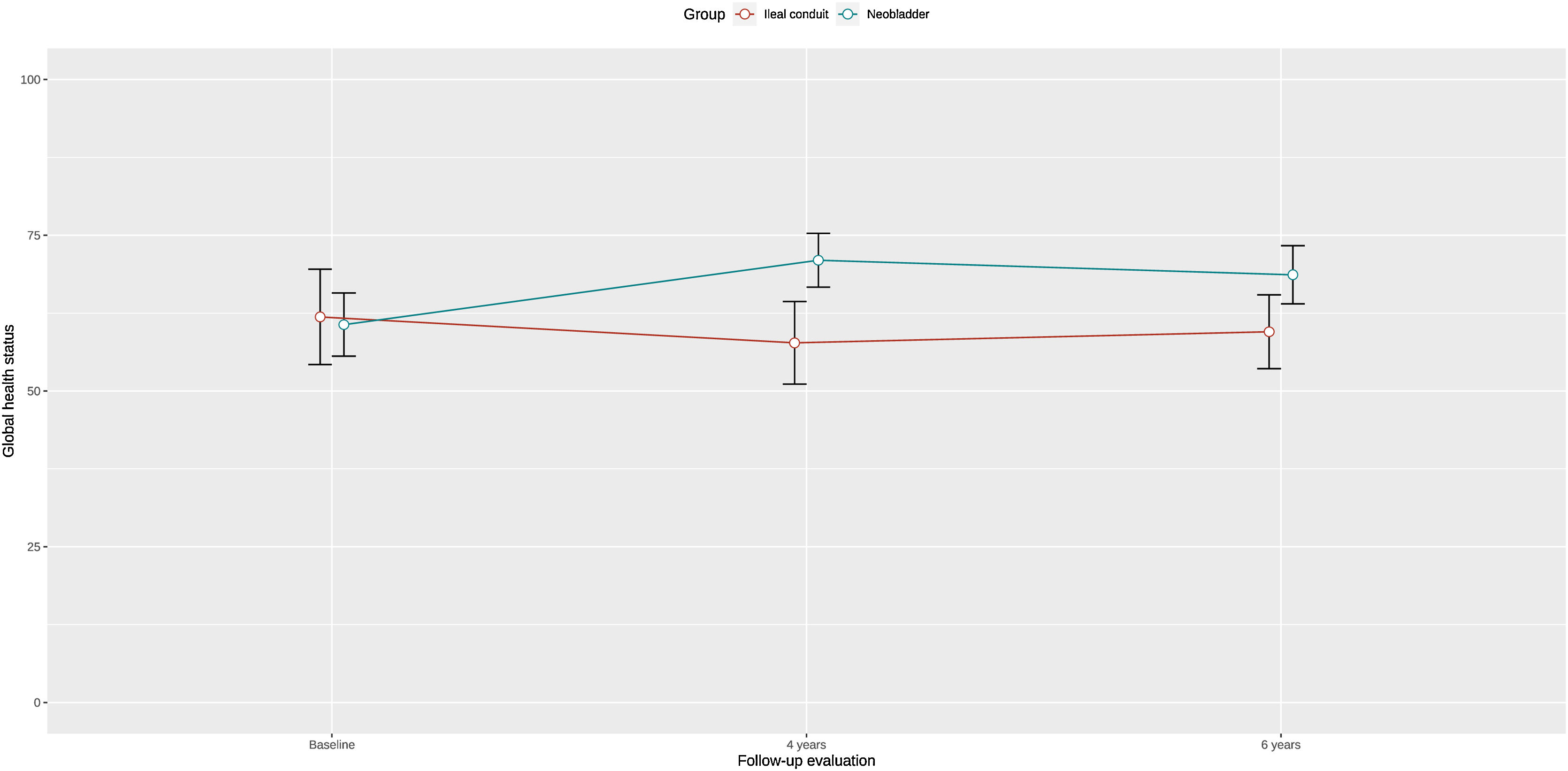
ResultsOf the patients, 64% (25/39) underwent ONB, and 76.9% (30/39) were male, with an average age of 69 years. No significant differences in overall good HRQOL (GHS > 70) were observed between ONB and IC at six years (IC: 60 ± 22; ONB: 69 ± 23, p = 0.2). Patients with IC reported higher insomnia at both follow-ups (4 years: p = 0.01; 6 years: p = 0.03). Emotional function remained stable in ONB patients but declined in IC patients from the fourth to sixth years (p = 0.04).
ConclusionLong-term HRQOL did not significantly differ between ONB and IC up to six years post-radical cystectomy. Both urinary diversion methods can be offered to patients, with tailored discussions in terms of HRQOL.
Evaluar la calidad de vida relacionada con la salud (CVRS) a los seis años de la cistectomía radical en pacientes con cáncer de vejiga músculo-invasor, comparando la neovejiga ileal ortotópica (NIO) y el conducto ileal (CI). El objetivo del estudio fue analizar los efectos a largo plazo (y poco estudiados) de los tratamientos estándar para el cáncer de vejiga en la CVRS y proporcionar información sobre las diferencias en la CVRS asociadas con estos dos métodos comunes de derivación urinaria.
Pacientes y métodosEste estudio prospectivo incluyó a 39 pacientes con carcinoma urotelial tratados con NIO o CI en nuestro centro entre 03/2013 y 01/2023. Se excluyeron pacientes con histología variante, metástasis, quimioterapia neoadyuvante o enfermedades benignas como indicación para la cistectomía. La CVRS se evaluó mediante el cuestionario QLQ-C30 de la European Organization for Research and Treatment of Cancer (EORTC) en el preoperatorio y a los cuatro y seis años del postoperatorio. Los análisis estadísticos incluyeron pruebas de Chi-cuadrado, pruebas T y modelos de regresión logística.
ResultadosDel total de pacientes, el 64% (25/39) fue sometido a NIO, y el 76,9% (30/39) eran varones, con una edad media de 69 años. No se observaron diferencias significativas en cuanto a buena CVRS global (ESG > 70) entre la NIO y el CI a los seis años (CI: 60 ± 22; NIO: 69 ± 23, p = 0,2). Los pacientes con CI refirieron mayor insomnio en los dos controles de seguimiento (4 años: p = 0,01; 6 años: p = 0,03). El estado emocional se mantuvo estable en los pacientes con NIO, pero disminuyó en los pacientes con CI del cuarto al sexto año (p = 0,04).
ConclusionesLa CVRS a largo plazo no mostró diferencias significativas entre la NIO y el CI durante los primeros seis años tras la cistectomía radical. Ambos métodos de derivación urinaria pueden ser opciones viables para los pacientes, con un asesoramiento personalizado basado en la CVRS de cada caso.
Bladder cancer remains the tenth most common malignancy worldwide.1 Neoadjuvant chemotherapy followed by radical cystectomy with lymphadenectomy and urinary diversion using either an orthotopic ileal neobladder (ONB) or an ileal conduit (IC) is the gold standard in the treatment of patients with localized muscle-invasive bladder cancer.2 In addition to the well-documented oncological benefits in the clinical setting,3–5 the impact of radical cystectomy and urinary diversion on health-related quality of life (HRQOL), including functional, psychological, social, and sexual aspects, must not be overlooked.6,7 Whether the type of urinary diversion significantly influences HRQOL remains inconclusive in the literature. While some studies demonstrate a benefit for patients with ONB,8 others report no significant difference between the two forms of urinary diversion regarding HRQOL.9,10 However, there is a paucity of long-term data in the literature that focus on the HRQOL after ONB versus IC.11 Most studies examine the changes in HRQOL in the early postoperative period up to two years only. Therefore, the objective of the current study is to investigate the outcomes of a prospective cohort over a follow-up period of six years.
Patients and methodsBetween March 2013 and January 2023, a total of 997 cystectomies were performed at our high-volume center. For analysis, only patients with histologically confirmed urothelial carcinoma who received open urinary diversion via ONB or IC were included. Both urinary diversions were thoroughly discussed with the patients and a shared decision on the type of urinary diversion was made. Patients with variant histology, metastasis, neoadjuvant chemotherapy, as well as cystectomy for benign reasons, were excluded. Additionally, to qualify for inclusion, patients were required to have consistently completed the European Organization for Research and Treatment of Cancer (EORTC) standardized QLQ-C30 questionnaire preoperatively, at four years, and at six years postoperatively.
The perioperative surgical procedures at our center have been previously published.12,13 Following approval by the local ethics committee (Ludwig Maximilian University of Munich, reference number: 20–179), patients were provided with the validated HRQOL questionnaires one to three days prior to radical cystectomy and were subsequently mailed the questionnaires at the defined postoperative intervals.
HRQOL was assessed pre- and postoperatively using a validated translation of the standardized EORTC QLQ-C30 questionnaire, following the current EORTC guidelines.14,15 Higher symptom scores indicated more severe symptoms, while higher functional scores represented better functionality. The general quality of life was also evaluated using the global health status (GHS) (questions 29 and 30 of the QLQ-C30 questionnaire), where higher scores denoted better overall HRQOL. Complications were documented based on the Clavien-Dindo classification.16
Statistical analysisFor all patients meeting the inclusion criteria, the primary endpoint of the study was the overall HRQOL, assessed using the QLQ-C30 GHS at the defined time points. Based on previously published validated cut-off values, a good HRQOL was defined as a GHS score of 70 or higher.17 The secondary endpoints included the evaluation of the respective QLQ-C30 domains (symptoms, functions).
Categorical and continuous variables were analyzed accordingly using the Chi-square test and the t-test. Potential predictors of good overall HRQOL, based on the QLQ-C30 GHS, were analyzed using univariate and multivariate regression models. In the univariate and multivariate linear and logistic regression, the following parameters were included: type of urinary diversion, sex, tumor staging, and age. All statistical analyses were performed using the R statistical software. A p-value of <0.05 was considered statistically significant.
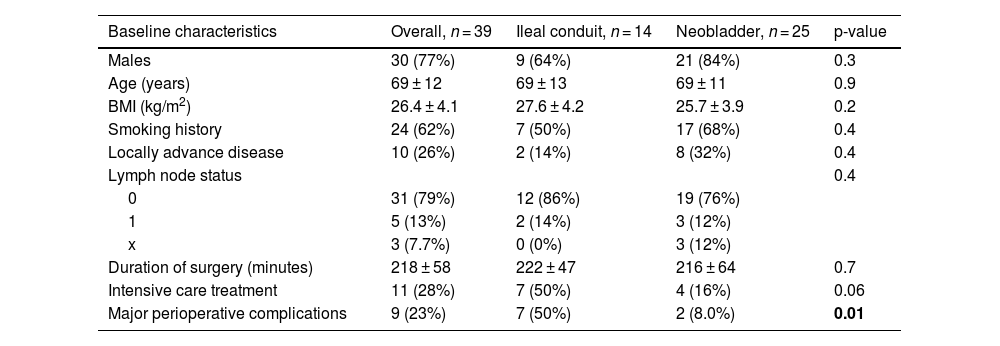
ResultsPatients characteristicsA total of 39 patients were included in the final analysis. The cohort consisted of 77% (30/39) males, with an average age of 69 years. The patient characteristics are summarized in Table 1. Except for "postoperative complications," no significant differences were observed between the two groups (IC vs. ONB). In summary, 64% (25/39) of the patients underwent radical cystectomy with ONB reconstruction. Of the patients who received an IC, 14% (2/14) presented locally advanced tumor growth at the time of surgery, compared to 32% (8/25) of those with an ONB (p = 0.4). The mean BMI was 28 for the IC group and 26 for the ONB group.
Baseline characteristics of participants undergoing urinary deviation with ileal conduit versus neobladder.
| Baseline characteristics | Overall, n = 39 | Ileal conduit, n = 14 | Neobladder, n = 25 | p-value |
|---|---|---|---|---|
| Males | 30 (77%) | 9 (64%) | 21 (84%) | 0.3 |
| Age (years) | 69 ± 12 | 69 ± 13 | 69 ± 11 | 0.9 |
| BMI (kg/m2) | 26.4 ± 4.1 | 27.6 ± 4.2 | 25.7 ± 3.9 | 0.2 |
| Smoking history | 24 (62%) | 7 (50%) | 17 (68%) | 0.4 |
| Locally advance disease | 10 (26%) | 2 (14%) | 8 (32%) | 0.4 |
| Lymph node status | 0.4 | |||
| 0 | 31 (79%) | 12 (86%) | 19 (76%) | |
| 1 | 5 (13%) | 2 (14%) | 3 (12%) | |
| x | 3 (7.7%) | 0 (0%) | 3 (12%) | |
| Duration of surgery (minutes) | 218 ± 58 | 222 ± 47 | 216 ± 64 | 0.7 |
| Intensive care treatment | 11 (28%) | 7 (50%) | 4 (16%) | 0.06 |
| Major perioperative complications | 9 (23%) | 7 (50%) | 2 (8.0%) | 0.01 |
Values presented as mean ± standard deviation or n (%). The chi-squared (χ2) and the two-sample t-test were performed for all comparisons. The b bold cells indicate statistically significant p-values. BMI: Body Mass Index.
Patients with an IC experienced significantly higher major (Clavien-Dindo ≥ III) perioperative complications, 50% (7/14), compared to patients with an ONB, 8% (2/25), p = 0.01. Furthermore, patients with IC were more frequently monitored in the intensive care unit (IC: 50% (7/14); ONB: 16% (4/25), p = 0.06). Histopathological examination of the resected lymph nodes revealed that 14% (2/14) of patients with an IC and 12% (3/25) of patients with an ONB had tumor-positive lymph nodes (p = 0.4).
HRQOL resultsThe assessment of HRQOL using the validated EORTC-QLQ-C30 questionnaire is summarized in Supplementary material 1 and Fig. 1. Overall, no significant difference in general good quality of life (GHS > 70) was observed between the two types of urinary diversion over the six-year period (IC vs. ONB: pre-op: 62 ± 29 vs. 61 ± 25, p = 0.9; 4-years FU: 58 ± 25 vs. 71 ± 22, p = 0.1; 6-years FU: 60 ± 22 vs. 69 ± 23, p = 0.2). However, there was a notable increase in GHS among patients with an ONB at the six-year follow-up, yet without reaching statistical significance.
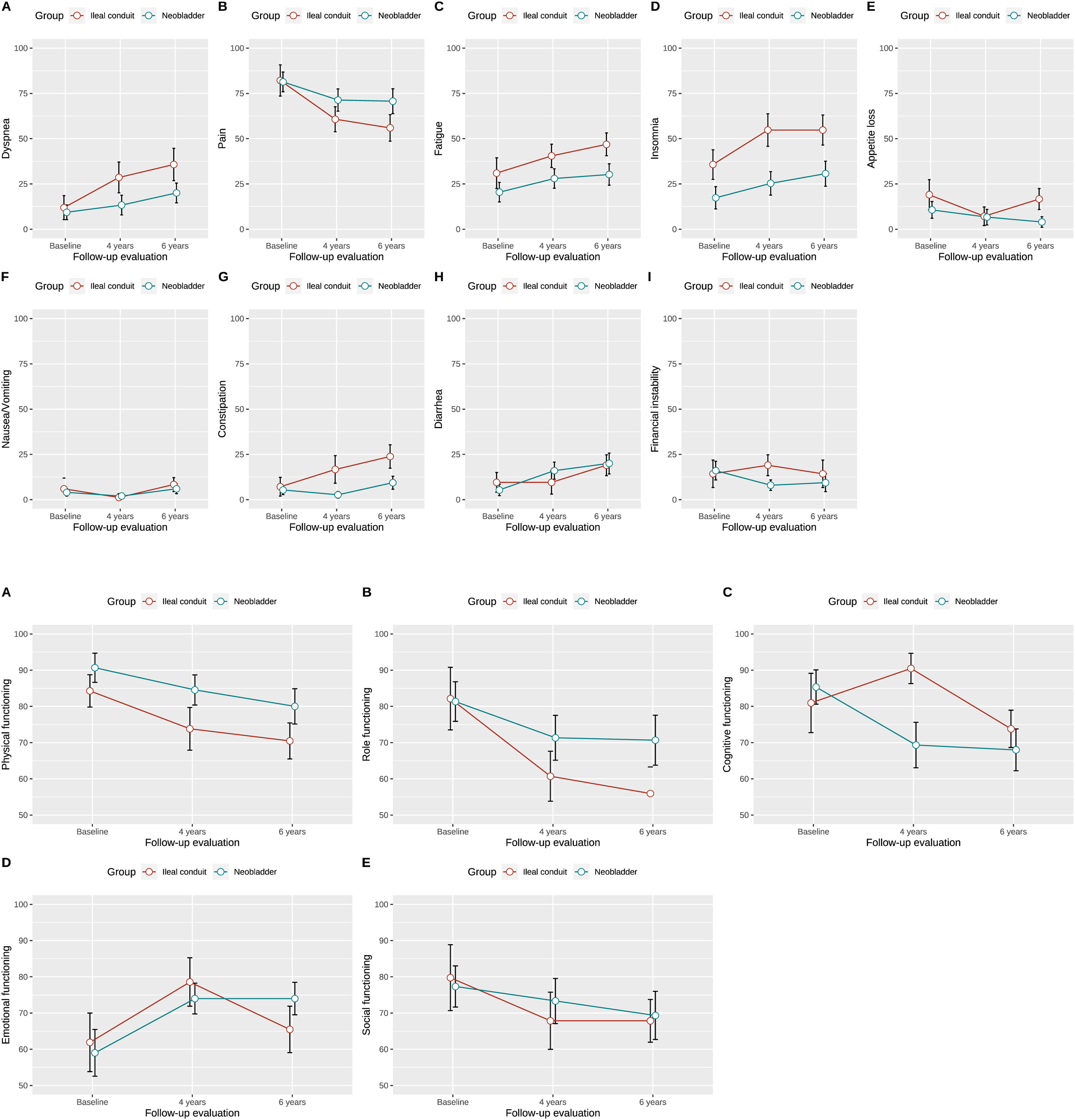
Regarding symptoms, patients with an IC exhibited statistically significant higher levels of insomnia compared to those with an ONB at both the four-year and six-year follow-ups (4-years FU: IC 55 ± 34 vs. ONB 25 ± 32, p = 0.01; 6-years FU: IC 55 ± 31 vs. ONB 31 ± 35, p = 0.03). These results are also depicted in Fig. 2A.
In terms of functionality (Fig. 2B), except for cognitive function, no statistically significant differences were observed between the two cohorts. Four years postoperatively, patients with an IC showed improved cognitive function (4-years FU: IC vs. ONB: 91 ± 16 vs. 69 ± 31, p = 0.008). However, this cognitive advantage diminished by the six-year follow-up (6-years FU: IC vs. ONB: 74 ± 19 vs. 68 ± 29, p = 0.5).
In a further analysis, we examined the absolute changes in HRQOL from baseline to the fourth and sixth postoperative year, as well as the changes between the fourth and sixth postoperative year. The results are summarized in Supplementary material 2. Patients with an ONB showed a significant improvement in loss of appetite compared to IC patients from the fourth to the sixth postoperative year (4-years FU to 6-years FU: IC vs. ONB: −10 ± 16 vs. 2.7 ± 9.2, p = 0.02). Additionally, emotional function remained stable in ONB patients while deteriorating in IC patients during the same period (4-years FU to 6-years FU: IC vs. ONB: −13 ± 19 vs. 0 ± 14, p = 0.04). Conversely, as previously described, patients with an IC demonstrated better cognitive function from the operation to the four-year follow-up (Pre-op to 4-years FU: IC vs. ONB: 9.5 ± 22 vs. −16 ± 33, p = 0.007). However, these differences leveled out over the long-term six-year period, resulting in no significant difference.
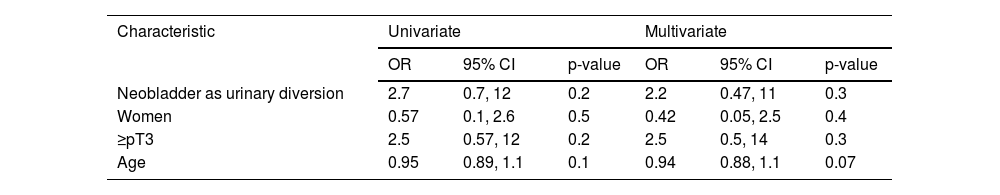
Predictive factors for a good general quality of lifeUltimately, neither univariate nor multivariate regression analyses identified urinary diversion with ONB, gender, age, or locally advanced tumor stage as independent predictors of overall good HRQOL. The results are summarized in Table 2.
Univariate and multivariate logistic regression models for global health status score ≥70.
| Characteristic | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Neobladder as urinary diversion | 2.7 | 0.7, 12 | 0.2 | 2.2 | 0.47, 11 | 0.3 |
| Women | 0.57 | 0.1, 2.6 | 0.5 | 0.42 | 0.05, 2.5 | 0.4 |
| ≥pT3 | 2.5 | 0.57, 12 | 0.2 | 2.5 | 0.5, 14 | 0.3 |
| Age | 0.95 | 0.89, 1.1 | 0.1 | 0.94 | 0.88, 1.1 | 0.07 |
CI: confidence interval; OR: odds ratio.
Radical cystectomy with pelvic lymphadenectomy and urinary diversion, either through ONB or IC, remains the surgical gold standard for the treatment of localized muscle-invasive bladder urothelial carcinoma.2 Though the oncological benefits are well-established,16,17 both types of urinary diversion significantly impact patients' daily activities and can substantially impair their HRQOL.6
Evaluating the long-term quality of life in these patients is crucial for tailoring the surgical approach to individual needs and for providing informed preoperative counseling regarding urinary diversion options.18 While short-term HRQOL after radical cystectomy is well-documented, there is a marked scarcity of studies investigating patient quality of life up to six years post-surgery.
Regarding overall patient satisfaction reflected in GHS, no significant advantage favoring one urinary diversion over the other was observed over the six years. However, a noteworthy increase in GHS was observed among patients with ONB over the six-year timeframe, contrasting with the stability seen in IC patients, suggesting a potential advantage for ONB as a urinary diversion. Nonetheless, statistical significance was not reached. Yet, this might be caused by the rather small patient cohort. Similar observations were noted by Singh et al., who reported significantly better GHS in the ONB cohort over an observation period of 18 months.19 This aligns with findings from other studies examining HRQOL post-radical cystectomy.10,20,21 However, ONB diversion as a predictor of overall good quality of life also did not achieve statistical significance in the multivariate or multivariate analysis.
Interestingly, patients with IC showed significantly higher rates of insomnia at both the four-year and six-year postoperative evaluations. Given the nocturnal incontinence often associated with ONB, one would typically expect an advantage for IC diversion. Similar findings were reported by Hobisch et al. and Volz et al., possibly attributable to the higher comorbidity burden often seen in patients with IC.10,20 The latter is also explained by the higher rates of major perioperative complications observed in the present cohort study, which is in line with previous relevant studies in the matter.22 Erber et al. also noted a significantly higher incidence of diarrhea in ONB patients compared to IC in their study.23 Despite the higher diarrhea rate observed in this study compared to the IC cohort, statistical significance was not attained. Furthermore, a slight, albeit non-significant advantage was observed in physical, social, and role functioning among ONB patients. This is consistent with earlier published studies.10,19,20,24 In contrast, IC patients demonstrated significantly improved cognitive function four years postoperatively, though this advantage diminished by the six-year follow-up.
Lastly, we examined prognostic factors for reduced overall HRQOL based on previously published GHS cutoff values.17 Similar to Tostivint et al., we did not identify significant predictors related to age, gender, choice of urinary diversion, or locally advanced tumor stage (>pT2).25
Even after six years, no significant difference in HRQOL was observed. Consequently, the choice of urinary diversion was not a predictor of HRQOL. Considering the contraindications of ONB, such as urethral carcinoma, impaired renal function (creatinine clearance <35−40 ml/min), limited life expectancy, or chronic inflammatory bowel disease, patients should be thoroughly informed about all forms of urinary diversion and their respective advantages and disadvantages. Based on our findings, both modalities of urinary diversion can be proposed to patients undergoing radical cystectomy, given that no significant differences in HRQOL are expected up to six years postoperatively.
It should be highlighted that this study is not devoid of some important limitations, mainly due to the requirement that patients had to complete the QLQ-C30 questionnaire preoperatively and at four and six years postoperatively. Additionally, it should be stressed that localized muscle-invasive bladder cancer has a high mortality, and plenty of patients were lost to follow-up or did not fulfill the questionnaires at a given time point. The latter has led to a relatively small number of included patients. Due to the small sample size, the interpretation of some analyses might be problematic. Importantly, we restricted our analyses to patients undergoing radical cystectomy with IC and ONB. Therefore, other commonly used urinary diversions such as ureterocutaneostomy or ileal pouch could not be evaluated. Importantly, other tools to assess HRQOL or frailty, as well as further risk items such as the ASA or the Charlson Comorbidity Index could not be provided. Moreover, patients opting for neoadjuvant chemotherapy were also excluded. The latter was mandatory given that neoadjuvant chemotherapy has started being widely used during the last few years. Nevertheless, due to the six-year follow-up of the study, most patients were operated in the previous decade, before the implementation of neoadjuvant chemotherapy.26 It should be also acknowledged that the EORTC QLQ30 was mainly developed to capture HRQOL in patients being treated with chemotherapy and strong deterioration of their well-being.14 Hence the validity of EORTC QLQ30 might be quite limited in detecting the long-term effect of surgical treatments on HRQOL.
ConclusionOverall patient HRQOL, reflected by GHS, did not significantly differ between ONB and IC over six years. Nevertheless, patients undergoing open urinary diversion with ONB showed an increasing trend in GHS, suggesting potential advantages. Patients with IC reported higher insomnia rates, contrasting expectations due to ONB-associated nocturnal incontinence. Based on the previous notion, the long-term HRQOL seems not to differ between ONB and INC. Therefore, both types of urinary diversion may be offered after careful patient selection.
CRediT authorship contribution statementNikolaos Pyrgidis, Julian Hermans and Yannic Volz contributed equally to the manuscript and read and approved the final version of the manuscript. All other authors were involved in the data analyzing, statistics and review of the manuscript.
FundingNo funding was received for this project.