There are very few Spanish studies that compare oncological outcomes following radical prostatectomy (RP) based on surgical approach, and their methodology is not appropriate.
ObjectiveTo compare oncological outcomes in terms of surgical margins (SM) and biochemical recurrence (BR) between open radical prostatectomy (ORP) and laparoscopic radical prostatectomy (LRP).
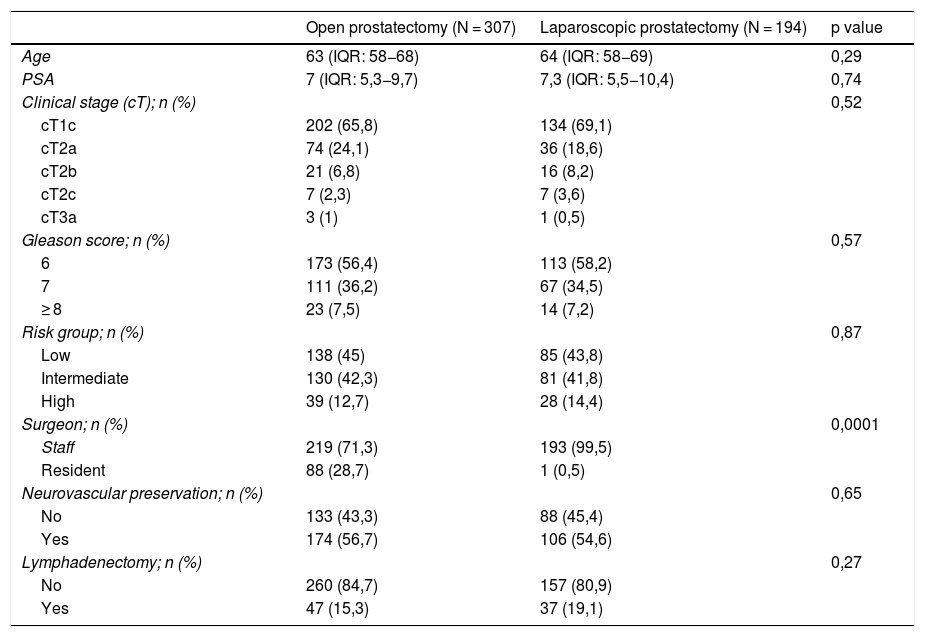
Material and methodsComparison of two cohorts (307 with ORP and 194 with LRP) between 2007−2015. Surgical margin status was defined as positive or negative, and BR as a PSA rise of >0,4 ng/ml after surgery.
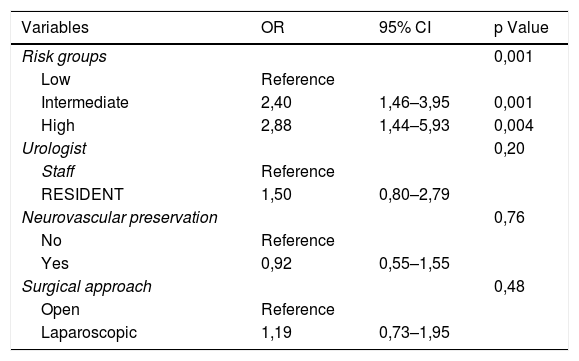
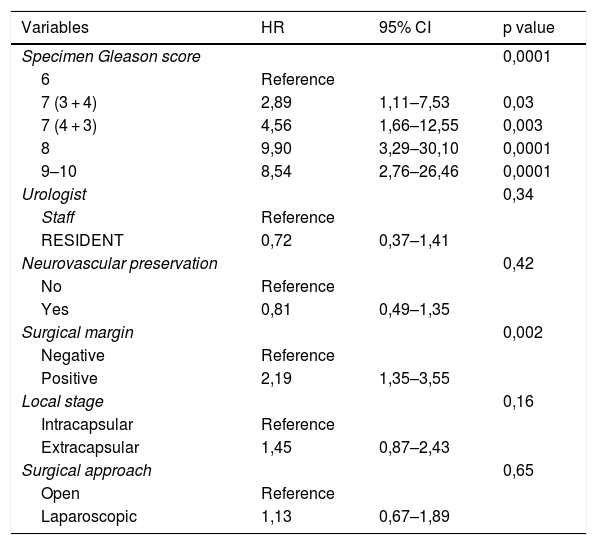
To compare the qualitative variables, we employed the Chi-squared test, and ANOVA was used for quantitative variables. We performed a multivariate analysis using logistic regression to evaluate the predictive factors of SM, and a multivariate analysis using Cox regression to evaluate the predictive factors of BR.
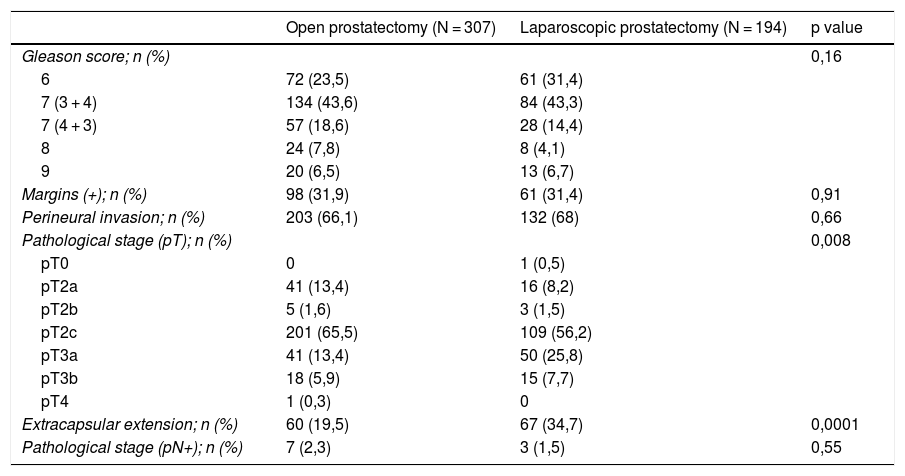
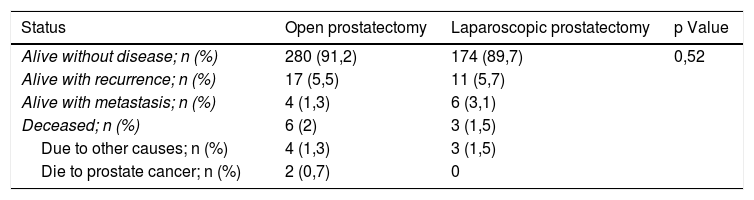
ResultsGleason 7(3 + 4) was determined in the surgical specimens of 43,5% of patients, and 31,7% had positive SM. The most frequent pathological stage was pT2c, on the 61,9% of the cases. No significant differences were found between both groups, except for extracapsular extension (p = 0,001), more frequent in LRP.
The median follow-up was 49 months. BR was seen in the 23% of patients, without significant differences between groups. In the multivariable analysis, only the D’Amico risk group behaved as an independent predictive factor of positive SM, and Gleason score and positive SM acted as independent predictive factors of BR.
ConclusionThe surgical approach did not influence SM status or BR.
Existe muy poca literatura española que compare resultados oncológicos tras prostatectomía radical (PR) según la vía de abordaje y la metodología es inadecuada.
Objetivocomparar los resultados oncológicos en cuanto a márgenes quirúrgicos (MQ) y recidiva bioquímica (RB) entre PR abierta y laparoscópica.
Material y métodos: Comparación de dos cohortes (307 con PRA y 194 con PRL) entre 2007 y 2015. El estado de los MQ se clasificaron como positivos o negativos y la RB como la elevación del PSA después de la PR > 0,4 ng/ml.
Para el contraste de variables cualitativas se utilizó el test Chi-cuadrado y ANOVA para las cuantitativas. Para evaluar los factores predictores de los MQ se ha realizado un análisis multivariante mediante regresión logística. Para evaluar los factores predictores de RB se ha realizado un análisis multivariable mediante regresión de Cox.
ResultadosEl 43,5% de pacientes tuvieron un Gleason 7(3 + 4) en la pieza quirúrgica y un 31,7% MQ positivos siendo el estadio patológico más frecuente pT2c en el 61,9%. No existieron diferencias significativas entre ambos grupos, excepto la afectación extracapsular (p = 0,001), más frecuente en PRL.
La mediana de seguimiento fue de 49 meses, evidenciando RB en el 23% de pacientes, sin diferencias significativas entre cohortes. En el análisis multivariable sólo el grupo de riesgo D’Amico se comportó como factor predictor independiente de MQ positivos y el score de Gleason y los MQ positivos como factores predictores independientes de RB.
ConclusiónLa vía de abordaje no influyó en el estado de MQ ni en la RB.