During the COVID-19 pandemic, the national transplant activity has been reduced due to the overload of the health system and concern for patient safety in this situation. The aim of our work is to expose the activity of kidney transplantation in Cantabria during the state of alarm, as well as to assess the safety of the transplantation program.
Material and methodsRetrospective study of kidney transplants performed in our Center from the beginning of the state of alarm until the beginning of the lockdown easing in Cantabria. Descriptive analysis of the demographic data of recipients and their donors, intraoperative data and postoperative outcomes. Comparative analysis with the data of the same period in 2017–2019, by means of the X2 for categorical variables, Student’s T and Mann-Whitney U tests in case of quantitative variables of normal and non-normal distribution, respectively.
ResultsFifteen kidney transplants were performed in the period described. Delayed renal function (DRF) was seen in 7.5% of patients, and 26.6% showed data of acute rejection; no patient presented COVID-19 disease.
Comparative analysis showed a remarkable increase in the number of transplants in comparison with previous periods (15 vs 5.6), at the expense of donors from outside Cantabria (93.3%). We found no statistically significant differences in terms of cold ischemia time (p 0.77), DRF (p 0.73), need for dialysis (p 0.54), or appearance of post-surgical complications (p 0.61).
ConclusionsThe evolution of the pandemic in our region, and the adoption of strict protective measures has allowed the early and safe resumption of the renal transplantation program, increasing the number of transplants performed compared to previous years and maintaining comparable early post-operative results.
Durante la pandemia COVID-19, la actividad nacional de trasplante se ha visto reducida por la sobrecarga del sistema sanitario, y la preocupación por la seguridad de los pacientes en esta situación. El objetivo de nuestro trabajo es exponer la actividad de trasplante renal en Cantabria durante el estado de Alarma, así como valorar la seguridad del programa de trasplante.
Material y métodosEstudio retrospectivo de los trasplantes renales realizados en nuestro Centro desde el inicio del estado de Alarma hasta el inicio del desconfinamiento en Cantabria. Análisis descriptivo de los datos demográficos de receptores y sus donantes, datos intraoperatorios y resultados postoperatorios. Análisis comparativo con los datos del mismo periodo de 2017–2019, mediante los estadísticos X2 para variables categóricas, T-Student y U de Mann-Whitney en caso de variables cuantitativas de distribución normal y no normal, respectivamente.
ResultadosSe realizaron 15 trasplantes renales en el periodo descrito. 7,5% de pacientes presentaron función renal retrasada (FRR), 26,6% mostró datos de rechazo agudo; ningún paciente presentó enfermedad por COVID-19. En el análisis comparativo, llamativo aumento del número de trasplantes frente a periodos anteriores (15 vs 5,6), a expensas de donantes de fuera de Cantabria (93,3%). No encontramos diferencias estadísticamente significativas en cuanto a tiempo de isquemia fría (p 0,77), FRR (p 0,73), necesidad de diálisis (p 0,54), o aparición de complicaciones postquirúrgicas (p 0,61).
ConclusionesLa evolución de la pandemia en nuestra región y la adopción de medidas de protección rigurosas ha permitido reiniciar el programa de trasplante renal de una forma temprana y segura, aumentando el número de trasplantes realizados frente a años anteriores y manteniendo unos resultados postoperatorios tempranos comparables.
Since its detection in China in January 2020, the COVID-19 disease has spread globally. On March 11th, 2020, after more than 210,000 cases had been reported, the World Health Organization (WHO) declared the situation to be a global pandemic.1 In February 2020, the first 2 cases were reported in Spain. From that moment onwards, it has spread throughout the national territory.2
The health system has had to adapt in order to be able to attend to the growing number of patients affected by COVID-19, and to continue providing safe and quality care to the rest of patients. As a result, it has become necessary to minimize surgical activity throughout Spain,3 following the recommendations of different organizations.4,5
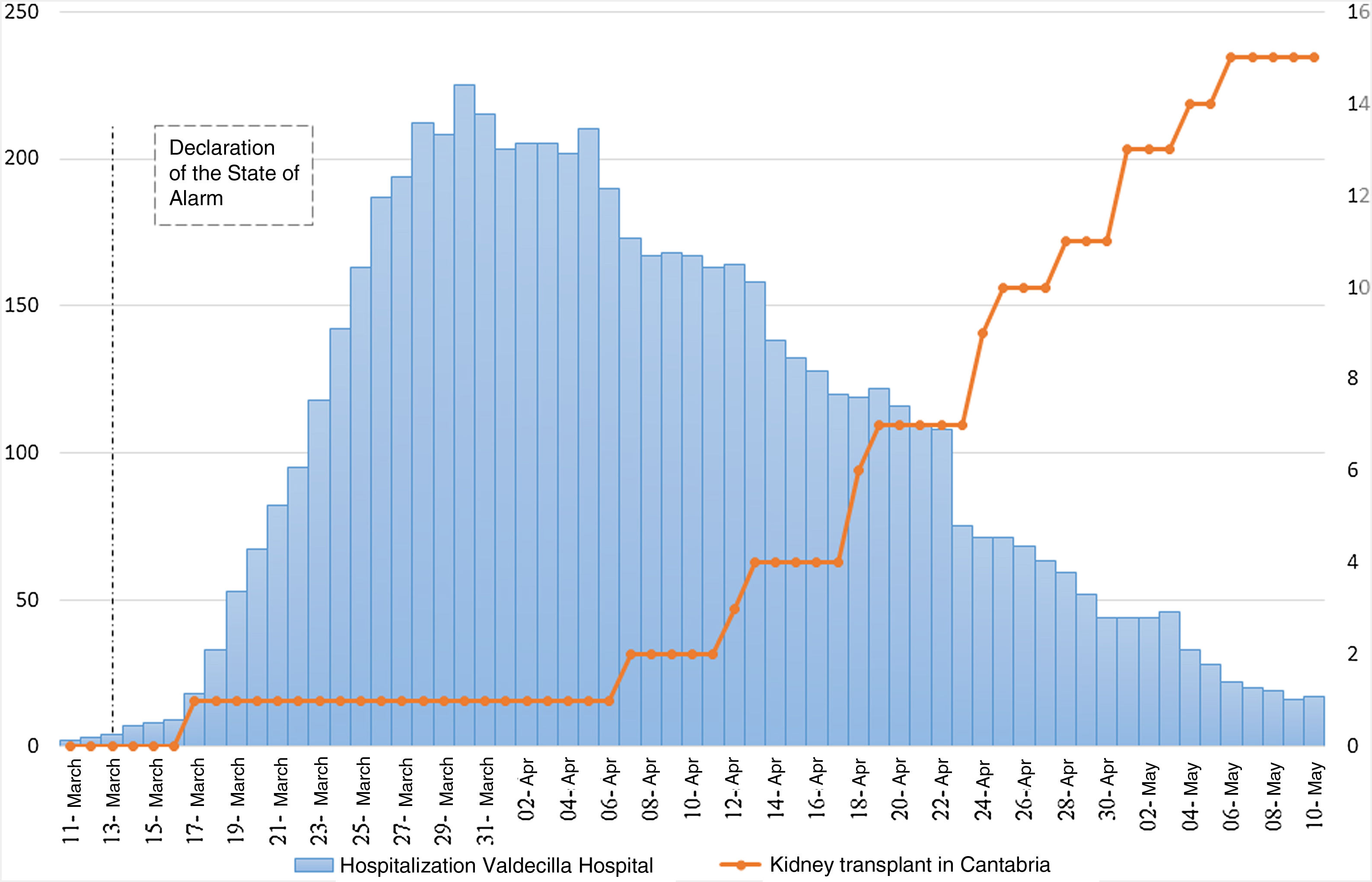
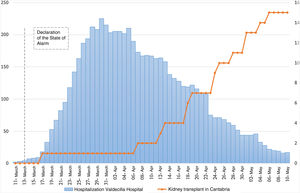
Transplant activity has been no exception. After the declaration of the state of alarm on March 13th, 2020, there was a drastic reduction in the number of donations and kidney transplants in the national territory. However, Cantabria has experienced an exceptional healthcare situation compared to other autonomous communities, with a maximum COVID-19 hospitalization peak of 400 patients, half of whom were located in the Marqués de Valdecilla University Hospital (Hospital Universitario Marqués de Valdecilla, HUMV). This, along with the enormous effort made by healthcare workers, has meant that the HUMV transplant program has been able to resume early, as opposed to the situation in most of the country.
The objective of the study is to present the activity and results of the kidney transplant program during the state of alarm in Cantabria, as well as to assess the safety of the program during the pandemic. To contextualize these results, they are compared to the same time period in the previous 3 years.
Material and methodsRetrospective data collection was carried out on the HUMV renal transplant activity in the period between the declaration of the state of alarm in Spain and the beginning of phase 1 of lockdown easing in Cantabria (May 11th) of the year 2020. The same data was collected for the same period from the years 2017–2019.
The kidney transplant protocol used follows the recommendations of European urology guidelines,6 and includes recommendations made by the National Transplant Organization (Organización Nacional de Trasplantes, ONT) during the COVID-19 pandemic:7
- -
All donors underwent SARS-COV-2 screening using a bronchoalveolar lavage sample, with a negative result.
- -
All renal recipients were subjected to a SARS-COV-2 PCR test by nasopharyngeal swab, with a negative result.
- -
Following protocol, recipients spend the first 24−48 hours in the intensive care unit after the intervention.
- -
The postoperative immunosuppression regimen is determined according to the risk of acute tubular necrosis (ATN) and the immunological risk:
- 1
In low-risk patients, the standard triple therapy regimen is used: Tacrolimus 0.1 mg/kg/12 h, Prednisone 10 mg/12 h and Mycophenolate mofetil (MMF) 500 mg/12 h.
- 2
In patients at high risk of type 3 ATN-asystole, donor older than 65, cold ischemia greater than 24 h, donor with cardiovascular risk factors: Tacrolimus 0.05 mg/kg/12 h, Prednisone 10 mg/ 12 h and MMF 500 mg/12 h and Basiliximab 20 mg is added.
- 3
In patients with high immunological risk-hyperimmunized patients (National Plan of Renal Exchange for Hyperimmunized Patients, PATHI) the standard regimen is established by adding Thymoglobulin to treatment. Dosage is dependent on lymphocyte count.
- -
During admission and after discharge, the nasopharyngeal swab is only repeated in patients with close contacts or symptomatology compatible with COVID-19.
Recipients' clinical variables were collected, including age, sex, origin, underlying kidney disease, comorbidities, and type of replacement therapy.
The donors' clinical variables (sex, age, origin, type of death), and HLA-ABDR mismatch were also recorded.
Perioperative variables were included, consisting of cold ischemia time, postoperative complications, classified according to the Clavien-Dindo system, delayed renal function (DRF) (defined as the need for dialysis in the first week after transplantation), the need for hemodialysis or renal biopsy, and functional results until removal of the ureteral catheter or discharge from hospital, using the analytical parameters of serum creatinine and glomerular filtration rate estimated by CKD-EPI.
A descriptive analysis of the results is carried out in the period described. The distribution of quantitative variables is analyzed by means of the Shapiro-Wilk test (or Kolmogorov-Smirnov), summarizing the results as median and standard deviation (SD) or median and interquartile range (IQR). Comparative analysis with data from the previous years, using χ2 for categorical variables, Student’s t for quantitative variables with normal distribution, and Mann-Whitney U for those with non-normal distribution. Statistical significance is taken to be a value of p < 0.05. Statistical analysis was performed with SPSS Statistics for Windows 22.0 (Armonk, NY: IBM Corp.)
ResultsIn the 2020 period described, 14 kidney transplants and one pancreas-kidney transplant were performed at this center. The median follow-up of the cohort was 40.5 days (IQR 33.5–48.5).
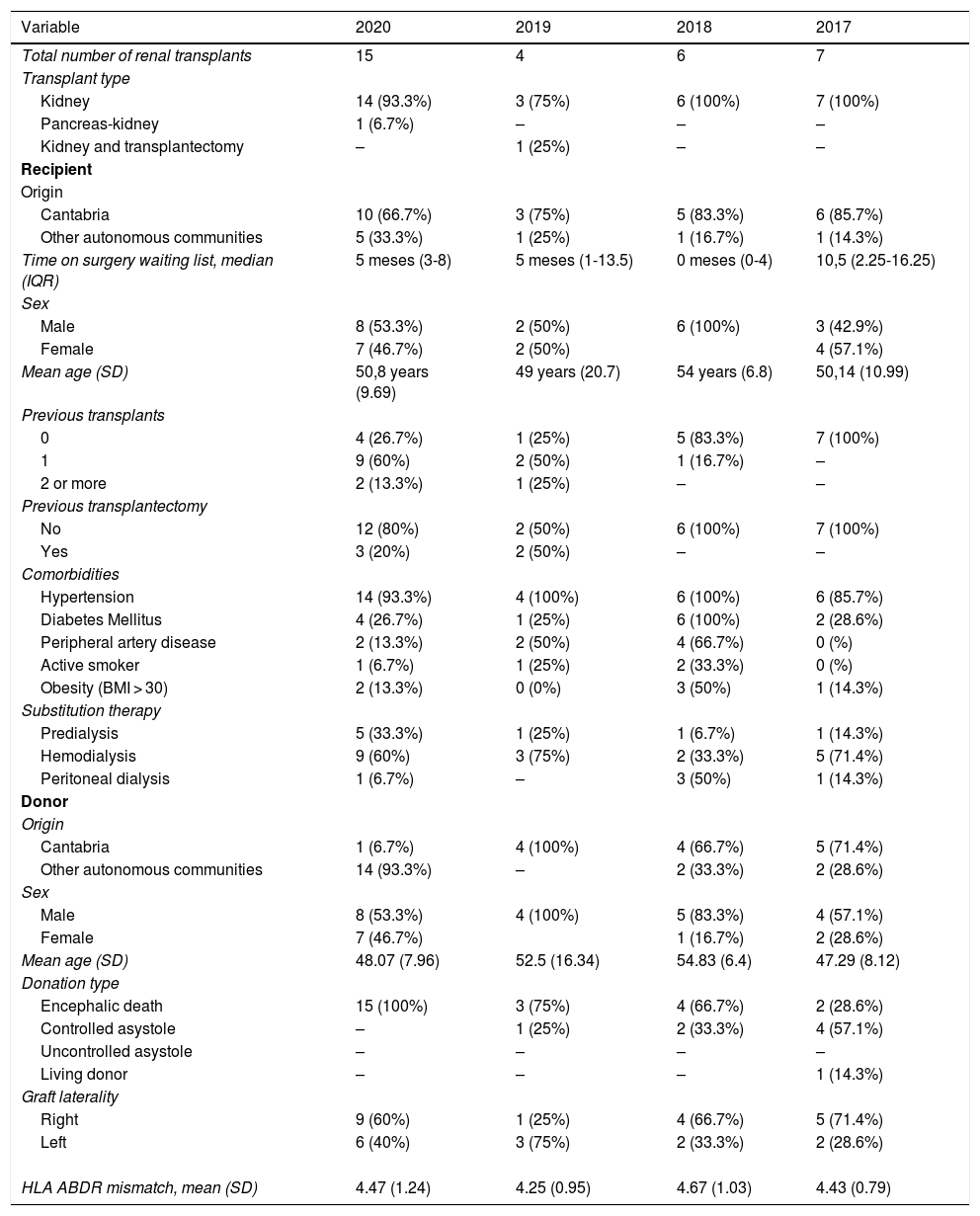
Table 1 shows the clinical variables of recipients and donors.
Demographics of recipients and donors.
| Variable | 2020 | 2019 | 2018 | 2017 |
|---|---|---|---|---|
| Total number of renal transplants | 15 | 4 | 6 | 7 |
| Transplant type | ||||
| Kidney | 14 (93.3%) | 3 (75%) | 6 (100%) | 7 (100%) |
| Pancreas-kidney | 1 (6.7%) | – | – | – |
| Kidney and transplantectomy | – | 1 (25%) | – | – |
| Recipient | ||||
| Origin | ||||
| Cantabria | 10 (66.7%) | 3 (75%) | 5 (83.3%) | 6 (85.7%) |
| Other autonomous communities | 5 (33.3%) | 1 (25%) | 1 (16.7%) | 1 (14.3%) |
| Time on surgery waiting list, median (IQR) | 5 meses (3-8) | 5 meses (1-13.5) | 0 meses (0-4) | 10,5 (2.25-16.25) |
| Sex | ||||
| Male | 8 (53.3%) | 2 (50%) | 6 (100%) | 3 (42.9%) |
| Female | 7 (46.7%) | 2 (50%) | 4 (57.1%) | |
| Mean age (SD) | 50,8 years (9.69) | 49 years (20.7) | 54 years (6.8) | 50,14 (10.99) |
| Previous transplants | ||||
| 0 | 4 (26.7%) | 1 (25%) | 5 (83.3%) | 7 (100%) |
| 1 | 9 (60%) | 2 (50%) | 1 (16.7%) | – |
| 2 or more | 2 (13.3%) | 1 (25%) | – | – |
| Previous transplantectomy | ||||
| No | 12 (80%) | 2 (50%) | 6 (100%) | 7 (100%) |
| Yes | 3 (20%) | 2 (50%) | – | – |
| Comorbidities | ||||
| Hypertension | 14 (93.3%) | 4 (100%) | 6 (100%) | 6 (85.7%) |
| Diabetes Mellitus | 4 (26.7%) | 1 (25%) | 6 (100%) | 2 (28.6%) |
| Peripheral artery disease | 2 (13.3%) | 2 (50%) | 4 (66.7%) | 0 (%) |
| Active smoker | 1 (6.7%) | 1 (25%) | 2 (33.3%) | 0 (%) |
| Obesity (BMI > 30) | 2 (13.3%) | 0 (0%) | 3 (50%) | 1 (14.3%) |
| Substitution therapy | ||||
| Predialysis | 5 (33.3%) | 1 (25%) | 1 (6.7%) | 1 (14.3%) |
| Hemodialysis | 9 (60%) | 3 (75%) | 2 (33.3%) | 5 (71.4%) |
| Peritoneal dialysis | 1 (6.7%) | – | 3 (50%) | 1 (14.3%) |
| Donor | ||||
| Origin | ||||
| Cantabria | 1 (6.7%) | 4 (100%) | 4 (66.7%) | 5 (71.4%) |
| Other autonomous communities | 14 (93.3%) | – | 2 (33.3%) | 2 (28.6%) |
| Sex | ||||
| Male | 8 (53.3%) | 4 (100%) | 5 (83.3%) | 4 (57.1%) |
| Female | 7 (46.7%) | 1 (16.7%) | 2 (28.6%) | |
| Mean age (SD) | 48.07 (7.96) | 52.5 (16.34) | 54.83 (6.4) | 47.29 (8.12) |
| Donation type | ||||
| Encephalic death | 15 (100%) | 3 (75%) | 4 (66.7%) | 2 (28.6%) |
| Controlled asystole | – | 1 (25%) | 2 (33.3%) | 4 (57.1%) |
| Uncontrolled asystole | – | – | – | – |
| Living donor | – | – | – | 1 (14.3%) |
| Graft laterality | ||||
| Right | 9 (60%) | 1 (25%) | 4 (66.7%) | 5 (71.4%) |
| Left | 6 (40%) | 3 (75%) | 2 (33.3%) | 2 (28.6%) |
| HLA ABDR mismatch, mean (SD) | 4.47 (1.24) | 4.25 (0.95) | 4.67 (1.03) | 4.43 (0.79) |
The mean age of the recipients was 50.8 years (SD 9.69), highlighting that 93.3% were hypertensive, 26.7% diabetic and 13.3% obese.
While 66.7% of the recipients resided in Cantabria, 33.3% came from other autonomous communities. Eleven patients were second or third transplants (73.3%), of which 3 had undergone transplantectomy.
The donors had a mean age of 48.1 (SD 7.96) years, with 93.3% coming from other autonomous communities. All were encephalic death donors, with no extended criteria donor.
Mean cold ischemia was 20.8 (SD 3.91) hours. After transplantation, 2 patients (7.5%) presented delayed renal function, requiring hemodialysis in the first postoperative week.
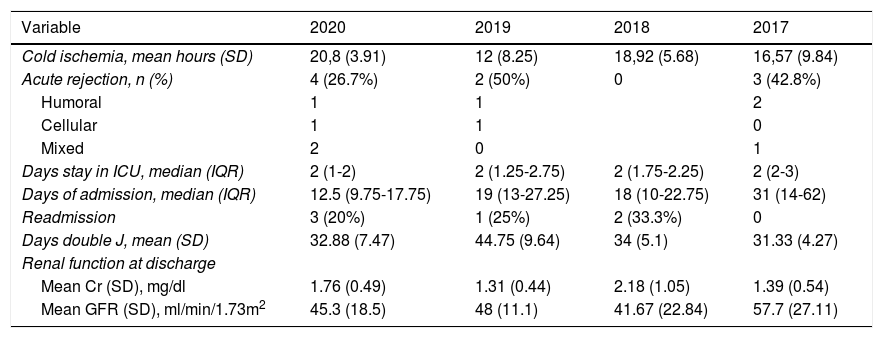
Postoperative data are detailed in Table 2. During admission, 2 patients presented fever, in the absence of respiratory, gastrointestinal, or voiding symptoms. Microbiological screening was performed, including a nasopharyngeal swab to rule out COVID-19, which was negative in both cases, and a chest radiograph without abnormalities.
Perioperative data of kidney transplant patients in each period.
| Variable | 2020 | 2019 | 2018 | 2017 |
|---|---|---|---|---|
| Cold ischemia, mean hours (SD) | 20,8 (3.91) | 12 (8.25) | 18,92 (5.68) | 16,57 (9.84) |
| Acute rejection, n (%) | 4 (26.7%) | 2 (50%) | 0 | 3 (42.8%) |
| Humoral | 1 | 1 | 2 | |
| Cellular | 1 | 1 | 0 | |
| Mixed | 2 | 0 | 1 | |
| Days stay in ICU, median (IQR) | 2 (1-2) | 2 (1.25-2.75) | 2 (1.75-2.25) | 2 (2-3) |
| Days of admission, median (IQR) | 12.5 (9.75-17.75) | 19 (13-27.25) | 18 (10-22.75) | 31 (14-62) |
| Readmission | 3 (20%) | 1 (25%) | 2 (33.3%) | 0 |
| Days double J, mean (SD) | 32.88 (7.47) | 44.75 (9.64) | 34 (5.1) | 31.33 (4.27) |
| Renal function at discharge | ||||
| Mean Cr (SD), mg/dl | 1.76 (0.49) | 1.31 (0.44) | 2.18 (1.05) | 1.39 (0.54) |
| Mean GFR (SD), ml/min/1.73m2 | 45.3 (18.5) | 48 (11.1) | 41.67 (22.84) | 57.7 (27.11) |
Regarding postoperative complications, 66.7% of the patients had no complications, 26.7% Clavien I-II complications, and only one patient had a Clavien IV complication - arterial thrombosis of the kidney graft in the combined transplant - which involved transplantectomy of the kidney graft.
The median hospital stay was 12.5 days (IQR 9.75−17.75), requiring readmission in 3 cases: one patient due to fever and 2 patients due to deterioration of renal function in the context of acute rejection. Four patients (26.6%) had histologically confirmed acute rejection. In the case of humoral rejection, they were treated with 6 sessions of plasmapheresis and intravenous immunoglobulins. In the case of cellular rejection, they were treated with Thymoglobulin.
In the comparative analysis carried out for the period 2017–2019, no statistically significant differences were found in sex, age, or comorbidities of the recipients. Nonetheless, there were statistically significant differences in terms of the number of previous transplants (p = 0.014). In 2020, 73.3% of recipients had received at least one previous transplant, while in previous years 76.5% were first transplants.
Regarding donors, there are statistically significant differences in their origin (p < 0.05), with 93.3% coming from outside the autonomous community in 2020, compared to 23.5% in previous years.
No significant differences were found in terms of cold ischemia time (p = 0.77), delayed kidney function (p = 0.73), need for dialysis (p = 0.54), or appearance of surgical complications (p = 0.61) or medical complications (p = 0.78).
DiscussionThe health alarm situation has put our healthcare system to the test. Given the high occupancy of intensive care units, and the need for readaptation of the operating room or resuscitation areas for the treatment of patients in serious situations due to COVID-19, the need arose to prioritize those patients who were to undergo surgical intervention during the state of alarm.
The European Association of Urology (EAU) published a series of general recommendations for the management and prioritization of urological patients during the healthcare emergency.4 In line with this, those elective urological procedures were suspended in the HUMV, keeping only oncological or urgent/emergent surgery.
Furthermore, it cannot only be considered a question of occupancy. According to the experience described by Lei et al., elective surgery in asymptomatic carrier patients or in the incubation period of SARS-COV-2 could accelerate and exacerbate the progression of the COVID-19 disease, reaching a mortality of 20.5% in this scenario.8 These proportions are much higher than those reported for patients hospitalized for COVID-19 without previous surgery, with a mortality of 2.3% of the general population.9,10
Within urological surgery, kidney transplantation presents a series of peculiarities, which can make these patients more susceptible to developing a serious infectious disease.
The potential transmission of the virus through human organ and tissue transplantation is unknown; COVID-19 cases have not been described in recipients suspected of originating from the donor. However, given the potential risk, the strictest measures must be maintained.
To date, small series of COVID-19 cases have been reported in transplant patients. Clinically, it presents more frequently with fever, cough, and dyspnea. On imaging tests, it appears as patchy ground-glass areas, mostly bilateral, especially in more severely ill patients. Zhu et al. compare COVID-19 pneumonia in kidney transplant recipients versus their healthy cohabitants, describing that transplant patients develop pneumonia of greater severity, along with longer hospital stay and viral clearance.11 Mortality rates in this population due to COVID-19 vary from 10 to 67% depending on the series.11–14 In Spain, the team at the University Hospital 12 de Octubre (Hospital Universitario 12 de Octubre) reports 18 cases of COVID-19 in transplant patients, with a mortality of 27.8%.15
In light of this, some transplant teams expressed their concern about the safety of transplant procedures during the pandemic.16
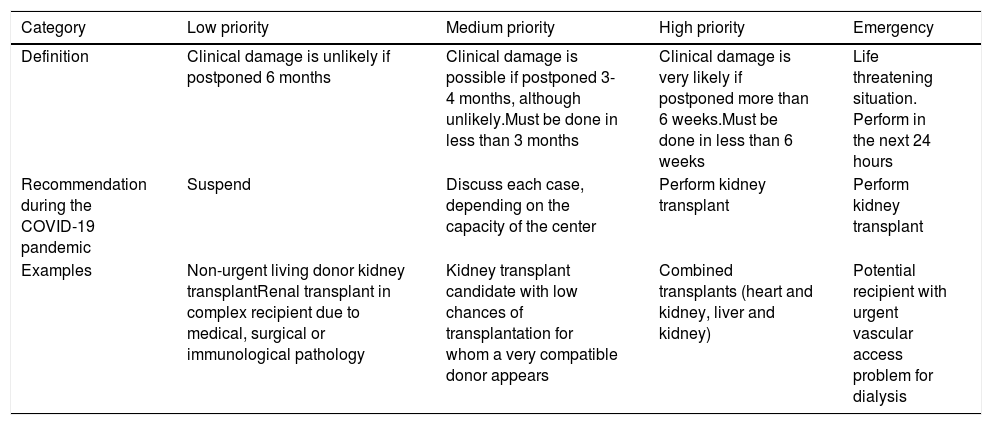
Scientific societies responded to the need for new measures and protocol. The EAU established a model for prioritizing transplant candidates during the pandemic,4 summarized in Table 3.
Prioritization recommendations for kidney transplantation according to the EAU during the COVID-19 pandemic period.
| Category | Low priority | Medium priority | High priority | Emergency |
|---|---|---|---|---|
| Definition | Clinical damage is unlikely if postponed 6 months | Clinical damage is possible if postponed 3-4 months, although unlikely.Must be done in less than 3 months | Clinical damage is very likely if postponed more than 6 weeks.Must be done in less than 6 weeks | Life threatening situation. Perform in the next 24 hours |
| Recommendation during the COVID-19 pandemic | Suspend | Discuss each case, depending on the capacity of the center | Perform kidney transplant | Perform kidney transplant |
| Examples | Non-urgent living donor kidney transplantRenal transplant in complex recipient due to medical, surgical or immunological pathology | Kidney transplant candidate with low chances of transplantation for whom a very compatible donor appears | Combined transplants (heart and kidney, liver and kidney) | Potential recipient with urgent vascular access problem for dialysis |
The ONT published a document which outlines recommendations for the selection of donors and recipients in addition to SARS-COV-2 screening during the pandemic,7 which should be individually implemented according to the resources of each center and the clinical situation of the potential recipient. It is recommended to prioritize emergency transplant candidates or those with low transplant possibilities, as would be the case with hyperimmunized patients. Initially, they also recommended restricting donation activity to optimal donors with encephalic death or controlled asystole, postponing the uncontrolled asystole donation program, intensive care oriented to donation or donors with expanded criteria.
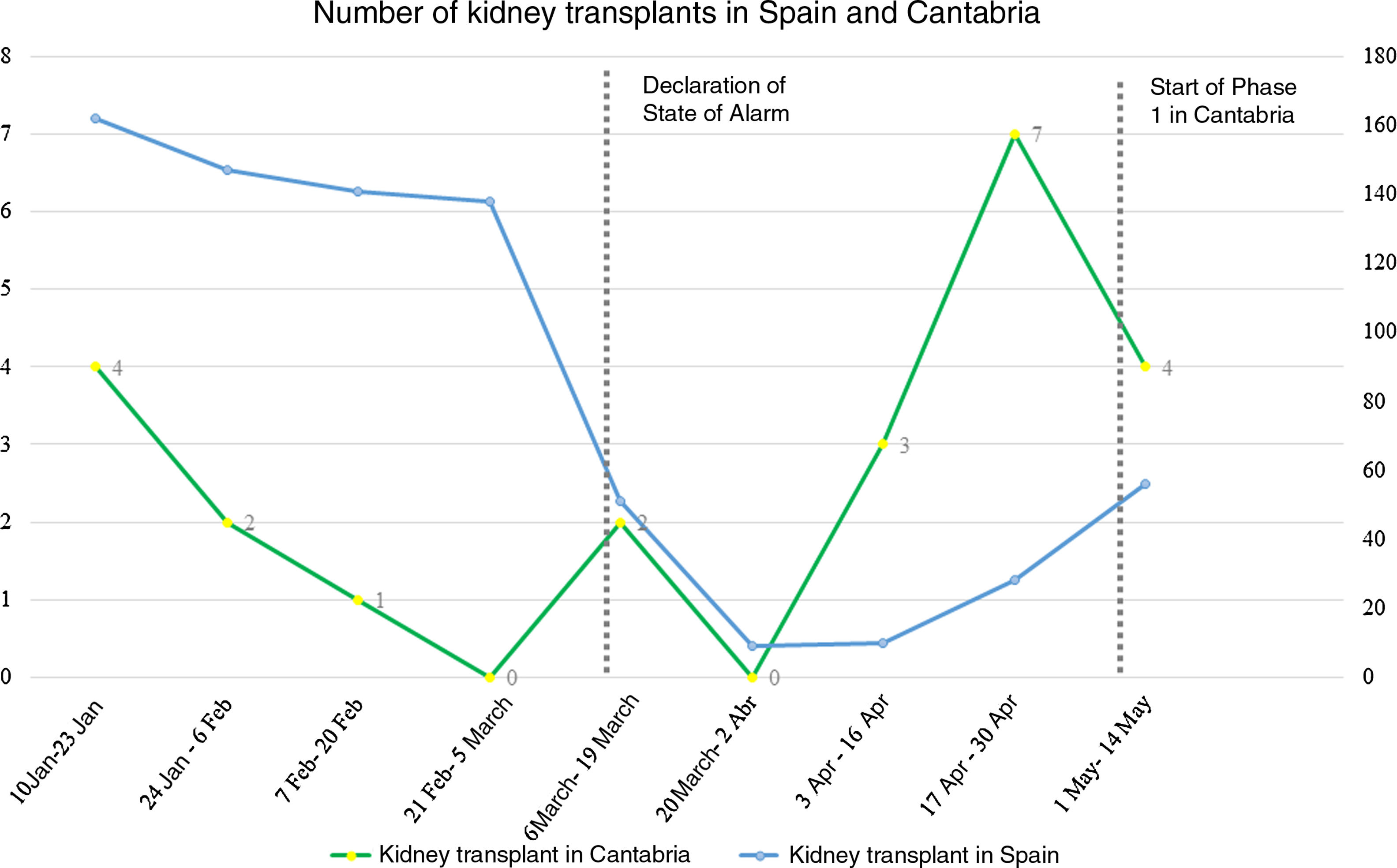
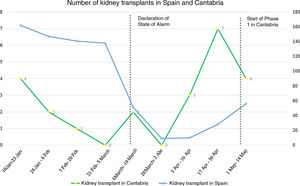
In Spain, the numbers of transplants decreased from an average of 16.1 transplants per day between January 1st and March 12th, to 2.1 daily transplants during the first 6 weeks of the state of alarm.16
In our center, given the risk of hospital saturation at the beginning of the pandemic, it was decided to reduce the transplant program to cadaver donors for patients within the PATHI. In this first period, only one kidney transplant was carried out in a hyperimmunized patient.
Similar to the proposals of Simonato et al.,17 the following measures were applied in order to continue offering safe care:
The hospital was divided into COVID and non-COVID zones, so that both areas were assisted by different personnel and followed different circuits and hospitalization areas. All patients were tested by nasopharyngeal swab prior to scheduled or urgent admission. The test was carried out in a specific area for this purpose, where they awaited the result before being transferred to the hospital ward. Surgery was suspended for those patients who required elective surgery and tested positive for SARS-COV-2. In those patients with a positive test but whose surgery was urgent, the intervention was performed under the appropriate protective measures. In addition, healthcare personnel with suspected/confirmed contact were also tested by PCR.
In the case of kidney transplant, the screening measures proposed by the ONT7 were applied, ruling out SARS-COV-2 infection in all donors, using bronchoalveolar lavage PCR, and in all recipients, using nasopharyngeal swab. During the study period, a potential renal recipient tested positive for SARS-COV-2 and was therefore rejected for transplant at that time.
As reflected in Fig. 1, after the application of the previous measures, and once the peak of hospitalization for COVID-19 had been exceeded, the decision was taken to restart the transplant activity using cadaveric donation. One exception was uncontrolled asystole, seeing as the extreme urgency of this activity did not ensure the security of the donation.
While national transplant activity continued to be very low (Fig. 2), activity at our center increased from one transplant in the first 3 weeks of the state of alarm to an average of 2.4 transplants/week in the subsequent weeks.
In the end, a total of 15 transplants were performed in the study period, while the average for the same periods of the previous 3 years was 5.6 transplants. Furthermore, these transplants were performed through donations from outside the autonomous community, in contrast to the mostly local donations in previous years. This reflects the impossibility of much of the national territory to take on transplants due to the enormous health overload that certain areas of Spain have experienced, which in this case has made it possible for Cantabria to almost triple the numbers of transplants compared to previous years.
During the study period, none of the recipients had COVID-19 symptoms, and the 2 cases that presented postoperative fever tested negative for SARS-COV-2 by nasopharyngeal swab. In addition, the early results of transplants are comparable to those of previous years.
Our study has different limitations. The retrospective nature of data collection may lead to some loss of information. Furthermore, the study sample is small, and the follow-up presented represents only the first postoperative month, without being able to predict what percentage of these patients may develop COVID-19 in the future.
Nevertheless, we believe that this reactivation period of the national transplant program it is encouraging. By taking the appropriate protective measures and following the SARS-COV-2 screening protocol, the kidney transplant program can be safely maintained.
ConclusionsThe adoption of rigorous measures and the low incidence of COVID-19 in our region made it possible to restart the kidney transplant program during the state of alarm safely for both staff and patients. The number of kidney transplants performed has increased compared to previous years, maintaining comparable early results.
Conflict of interestThe authors certify that there is no conflict of interest.
Please cite this article as: Calleja Hermosa P, Varea Malo R, Campos Juanatey F, Rodrigo Calabia E, Aguilera Fernández A, Fernández Guzmán E et al. Actividad y resultados a corto plazo del trasplante renal durante la pandemia COVID-19. Actas Urol Esp. 2021;45:116–123.