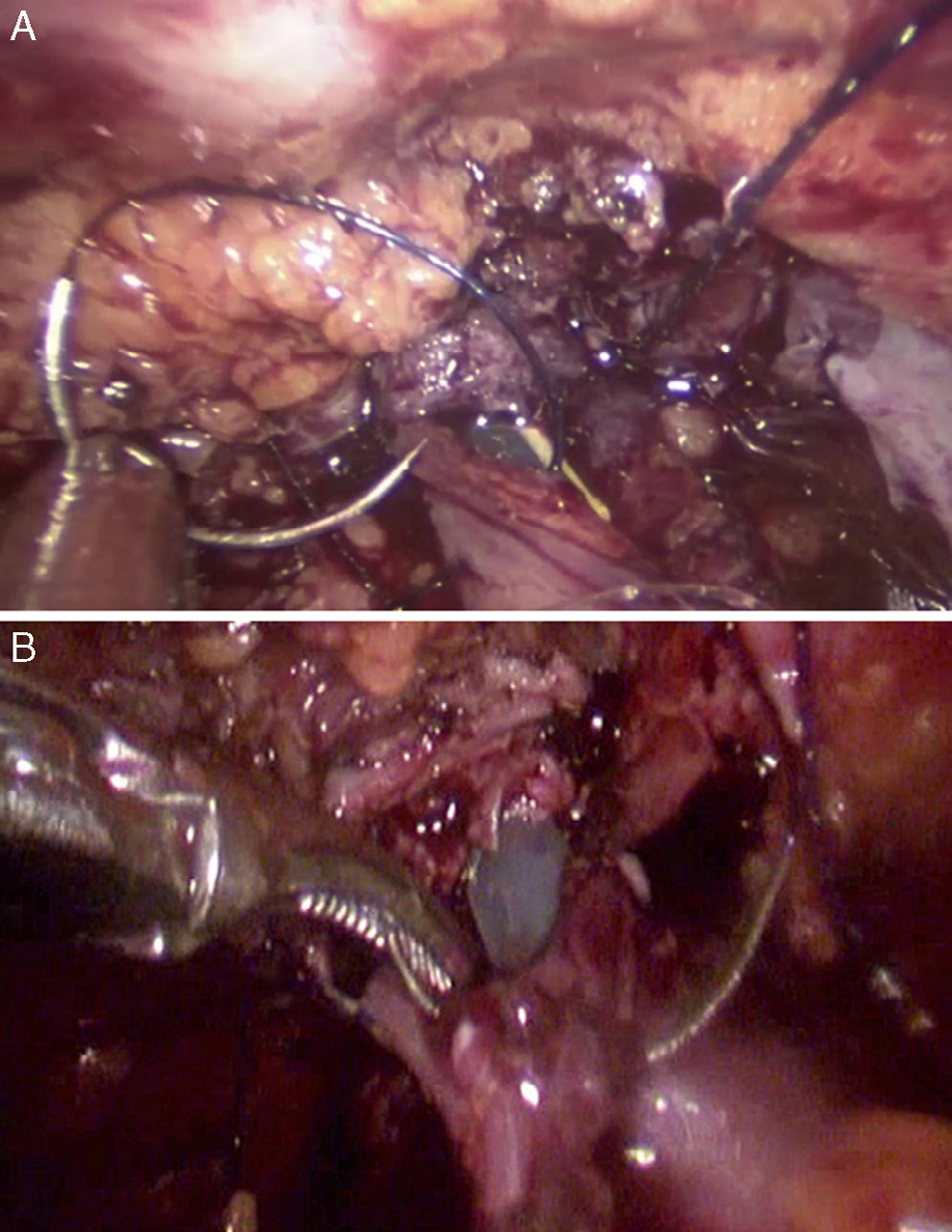
Probably, laparoscopic radical cystectomy with ileal neobladder and neovesicourethral anastomosis is one of the most complex procedures in minimally invasive surgery.
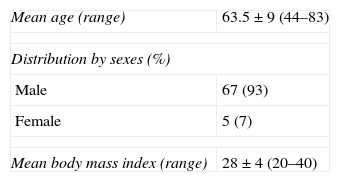
Materials and methodsProspective study carried out in 72 patients surgically treated for invasive bladder neoplasia between January 2008 and October 2013. Patients underwent radical cystectomy with ileal neobladder (open approach in 33 patients and laparoscopic approach in 39). The study assessed comparatively surgical outcomes, continence rate and postoperative complications.
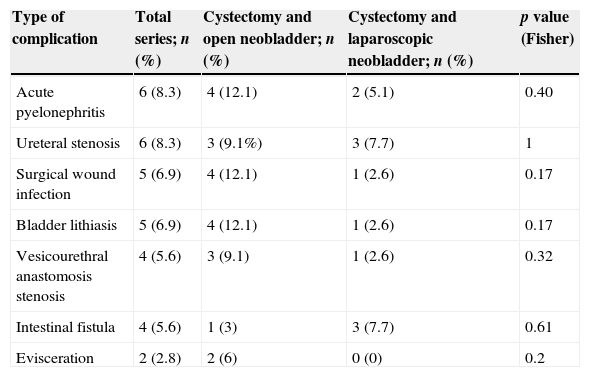
ResultsMean age was 63.5±9 years (64.3 open vs. 62.7 laparoscopic, p=0.46), mean surgery time 323.6±78.7minutes (321.3 vs. 326.5, p=0.77), average hospital stay 14.8 days±8.1 (16.2 vs. 13.6, p=0.2), transfusion rate 40.3% (66.7% vs. 17.9%, p<0.0001) and complications rate 47.2% (63.6% vs. 33.3%, p=0.01). Major complications were reported in 29.1% of cases (39.4% open vs. 20.5% laparoscopic, p=0.07). With a mean follow-up rate of 42.5±19.2 months (range 15–70), 50 (69.4%) patients remained alive and free of disease. Continence was evaluated in these patients: total continence rate was 38% (50% vs. 27%, p=0.09) and diurnal continence rate 58% (70.8% vs. 46.1%, p=0.07). Self-catheterization rate was 8% (4.2% vs. 11.5%, p=0.67). Total incontinence rate was 34% (25% vs. 42.3%, p=0.19).
ConclusionAccording to our experience, transfusion rate, number and severity of complications are lower in laparoscopic cystectomy with ileal neobladder. No statistically significant impact on operative time and on hospital stay was observed. In patients undergoing laparoscopic approach, continence rate is lower but not statistically significant.
La cistectomía radical laparoscópica con neovejiga ileal y anastomosis neovesicourethral realizada por laparoscopia posiblemente sea uno de los procedimientos más complejos de la cirugía mínimamente invasiva.
Material y métodosEstudio prospectivo realizado entre enero de 2008 y octubre de 2013 con 72 pacientes afectos de neoplasia vesical infiltrante, intervenidos mediante cistectomía radical con neovejiga ileal (33 mediante técnica abierta y 39 laparoscópica). Evaluamos de forma comparativa los resultados quirúrgicos, la tasa de continencia y las complicaciones postoperatorias.
ResultadosLa edad media fue 63,5±9 años (64,3 abierta vs. 62,7 laparoscópica, p=0,46), el tiempo medio quirúrgico 323,6±78,7min (321,3 vs. 326,5, p=0,77), la estancia media 14,8 ±8,1 días (16,2 vs. 13,6, p=0,2), la tasa de transfusión 40,3% (66,7% vs. 17,9%, p<0,0001), la tasa de complicaciones 47,2% (63,6% vs. 33,3%, p=0,01). Sucedieron complicaciones mayores en 29,1% (39,4% abierta vs. 20,5% laparoscópica, p=0,07). La media de seguimiento fue 42,5±19,2 meses (rango 15-70); 50 pacientes (69,4%) estaban vivos y libres de enfermedad y pudieron ser evaluados con respecto al estado de continencia. La tasa de continencia total fue 38% (50% vs. 27%, p=0,09) y la tasa de continencia diurna 58% (70,8% vs. 46,1%, p=0,07). La proporción de pacientes con autocateterismo fue 8% (4,2% vs. 11,5%, p=0,67). La tasa de incontinencia total fue 34% (25% vs. 42,3%, p=0,19).
ConclusiónEn nuestra experiencia la tasa de transfusión, el número y severidad de complicaciones es menor en la cistectomía radical con neovejiga realizada mediante abordaje laparoscópico, sin claro impacto en el tiempo quirúrgico y en la estancia hospitalaria. La tasa de continencia de los pacientes intervenidos mediante abordaje laparoscópico es inferior, aunque sin alcanzar significación estadística.