To validate the technique of selective sentinel node biopsy for diagnosing and staging intermediate to high-risk prostate cancer by comparing the technique with conventional extended lymphadenectomy (eLFD) in a prospective, longitudinal comparative study.
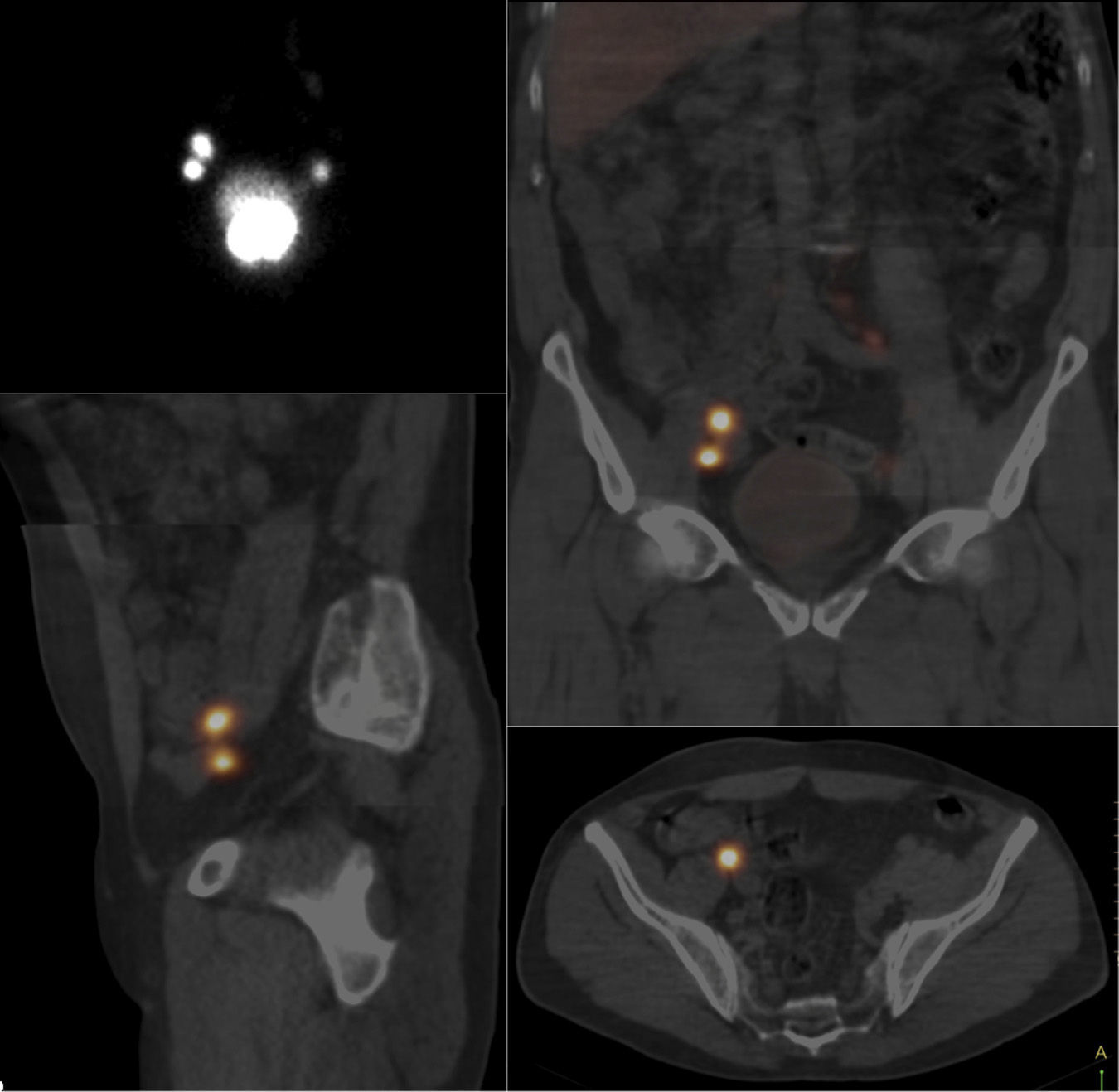
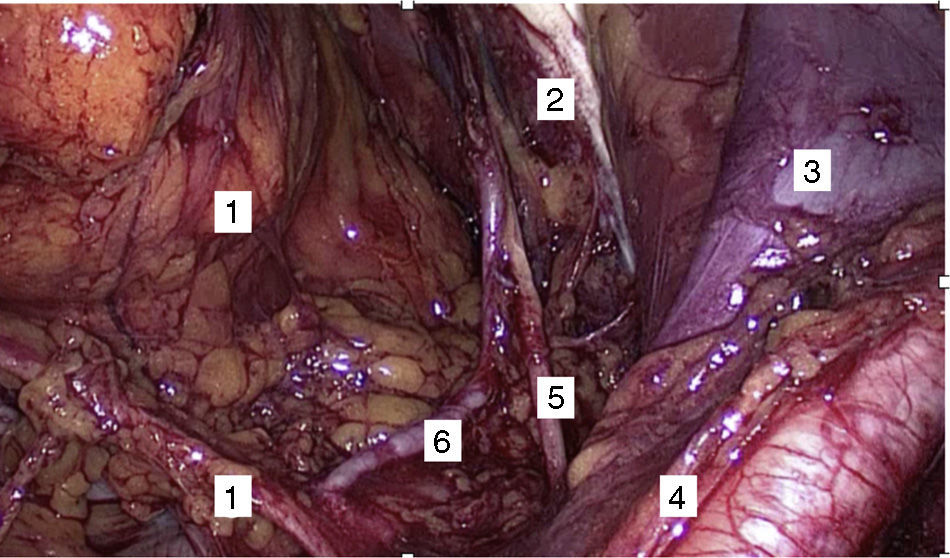
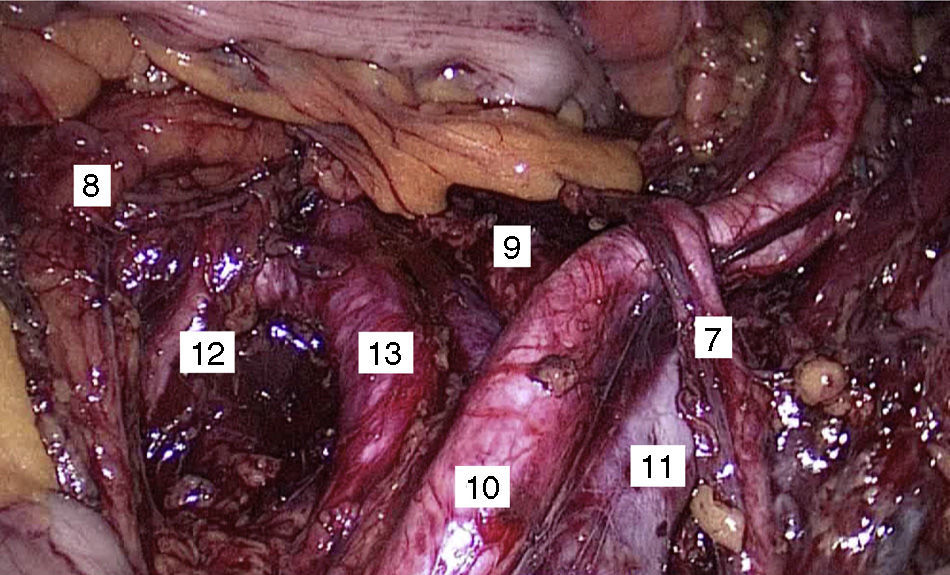
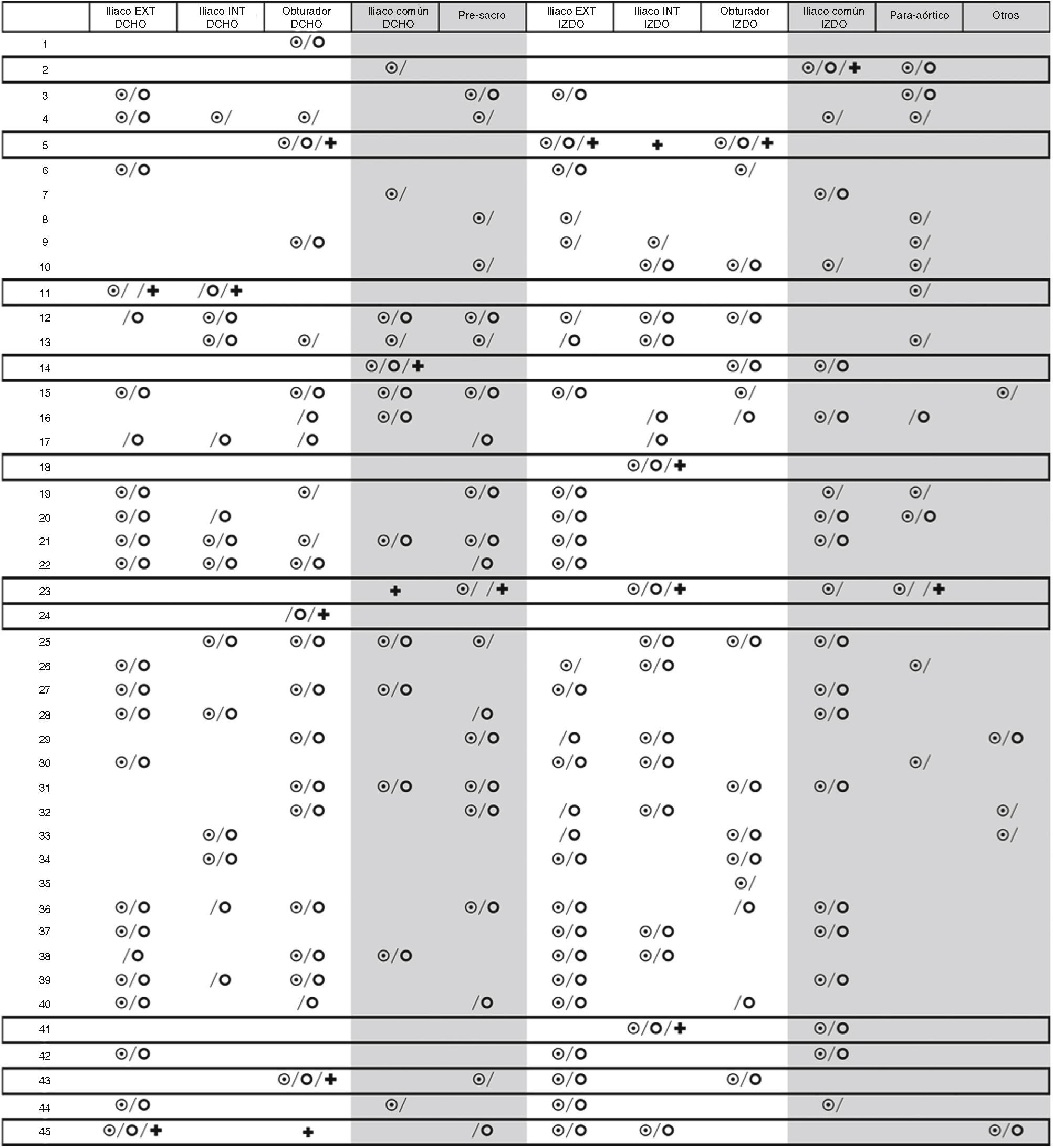
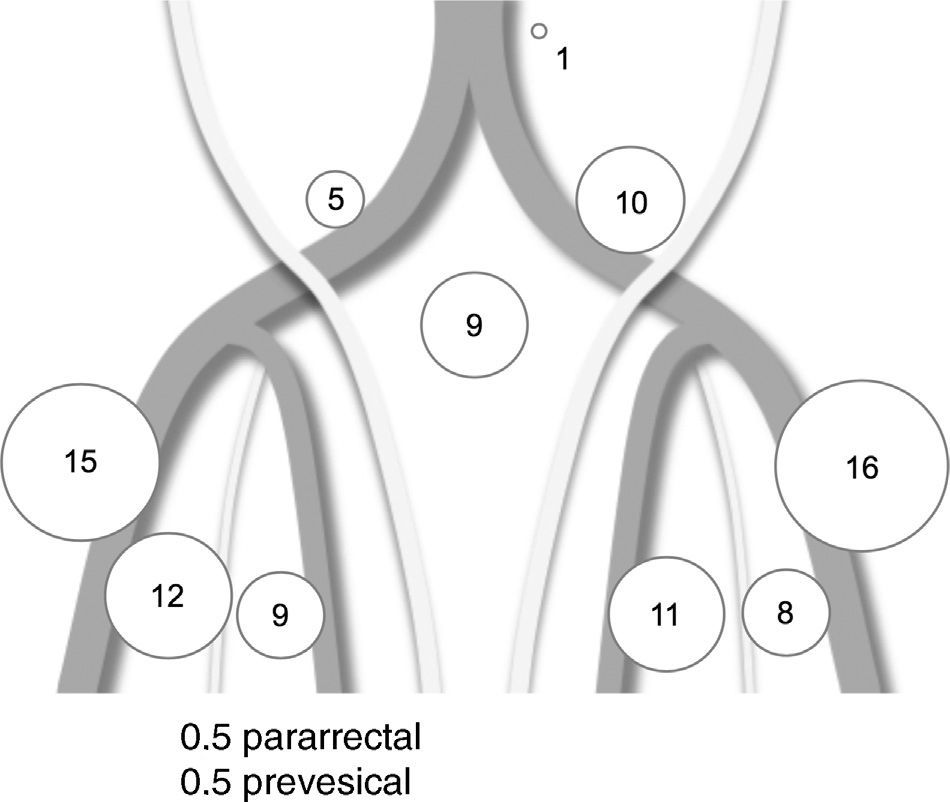
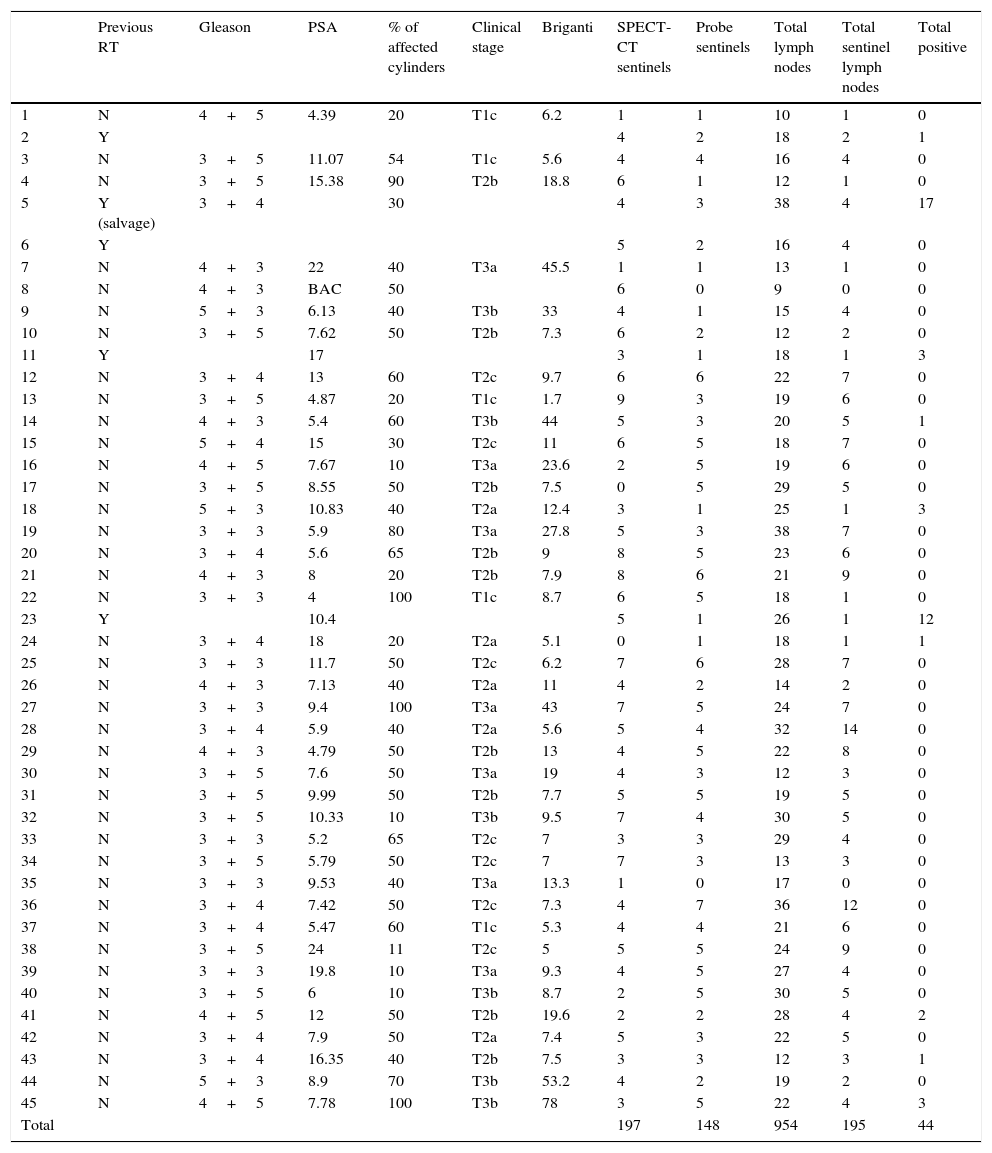
MethodsWe applied the technique to 45 patients. After an intraprostatic injection of 99mTc-nanocolloid and preoperative single-photon emission computed tomography (SPECT/CT), we extracted the sentinel lymph nodes, guided by a portable Sentinella® gamma camera and a laparoscopic gamma-ray detection probe. The eLFD was completed to establish the negative predictive value of the technique.
ResultsSPECT/CT showed radiotracer deposits outside the eLFD territory in 73% of the patients and the laparoscopic gamma probe in 60%. The mean number of active foci per patient was 4.3 in the SPECT/CT and 3.2 in the laparoscopic gamma probe. The mean number of extracted sentinel lymph nodes was 4.3 (0–14), with 26% outside the eLFD territory. The lymph nodes were metastatic in 10 patients (22%), 6/40 (15%) when the prostatectomy was the primary treatment. In all cases with metastatic lymph nodes, there was at least one positive sentinel node. Metastatic sentinel lymph nodes were found outside the eLFD territory in 3/10 patients (30%). The sensitivity was 100%, the specificity was 94.73%, the positive predictive value was 81.81%, and the negative predictive value was 100%.
ConclusionSelective sentinel node biopsy is superior to eLFD for diagnosing lymph node involvement and can avoid eLFD when metastatic sentinel lymph nodes are not found (85%), with the consequent functional advantages.
Validar la técnica de biopsia selectiva de ganglio centinela en el diagnóstico y estadificación del cáncer de próstata de riesgo intermedio y alto mediante comparación con la linfadenectomía extendida convencional (eLFD) en un estudio prospectivo longitudinal y comparativo.
MétodosHemos aplicado la técnica a 45 pacientes. Previa inyección intraprostática de 99mTc-nanocoloide y SPECT-TC preoperatoria, se han extraído los ganglios centinela guiados con gammacámara portátil Sentinella® y sonda detectora de rayos gamma laparoscópica. Se completó la eLFD para establecer el valour predictivo negativo de la técnica.
ResultadosLa SPECT-TC mostró depósitos del radiotrazador fuera del territorio de la eLFD en el 73% de los pacientes y la gammasonda laparoscópica en el 60%. La media de focos activos por paciente en la SPECT-TC fue de 4,3 y con gammasonda laparoscópica de 3,2. La media de ganglios linfáticos centinelas extraídos fue 4,3 (0-14), el 26% fuera del territorio de la eLFD. En 10 pacientes (22%) se encontraron ganglios metastásicos, 6/40 (15%) cuando la prostatectomía fue el tratamiento primario. En todos los casos con ganglios metastásicos hubo, al menos, un ganglio centinela positivo. Se encontraron ganglios centinela metastásicos fuera del territorio de la eLFD en 3/10 pacientes (30%). La sensibilidad fue del 100%, la especificidad del 94,73%, el valour predictivo positivo del 81,81% y el valour predictivo negativo del 100%.
ConclusiónLa biopsia selectiva del ganglio centinela es superior a la eLFD en el diagnóstico de afectación ganglionar, y puede evitar la eLFD cuando no se encuentren ganglios centinela metastásicos (85%), con las consecuentes ventajas funcionales.