The current COVID-19 pandemic has rendered up to 15% of patients under mechanical ventilation. Because the subsequent tracheotomy is a frequent procedure, the three societies mostly involved (SEMICYUC, SEDAR and SEORL-CCC) have setup a consensus paper that offers an overview about indications and contraindications of tracheotomy, be it by puncture or open, clarifying its respective advantages and enumerating the ideal conditions under which they should be performed, as well as the necessary steps. Regular and emergency situations are displayed together with the postoperative measures.
La alta incidencia de insuficiencia respiratoria aguda en el contexto de la pandemia por COVID-19 ha conllevado el uso de ventilación mecánica hasta en un 15%. Dado que la traqueotomía es un procedimiento quirúrgico frecuente, este documento de consenso, elaborado por tres Sociedades Científicas, la SEMICYUC, la SEDAR y la SEORL-CCC, tiene como objetivo ofrecer una revisión de las indicaciones y contraindicaciones de traqueotomía, ya sea por punción o abierta, esclarecer las posibles ventajas y exponer las condiciones ideales en que deben realizarse y los pasos que considerar en su ejecución. Se abordan situaciones regladas y urgentes, así como los cuidados posoperatorios.
Tracheotomy is a common procedure in intensive care units (ICU) in patients with respiratory failure requiring mechanical ventilation.1
The recent COVID-19 pandemic, in its most severe form, presents with a picture of acute respiratory failure that can evolve into acute respiratory distress syndrome (ARDS), which in many patients requires initiation of mechanical ventilation. In the different series, between 9.8% and 15.2% of these patients have required mechanical ventilation.2–4 Surgical tracheotomy is the most common surgical procedure among critically ill COVID-19 patients.5
The mortality of COVID-19 patients on mechanical ventilation is high, up to 50%.6 These patients require ventilatory strategies that in the initial stages involve deep analgesia and even relaxation, protective ventilation, recruitment manoeuvre and prone position.7 All this means that many patients will remain on mechanical ventilation for days, with a high risk of developing ICU- acquired weakness, making weaning them from mechanical ventilation difficult. The use of specific antiviral drugs may interact with sedatives and analgesics, prolonging their effects.8 The onset of delirium, frequent in this type of patient, may also influence successful withdrawal of mechanical ventilation.
SARS-CoV-2 has a demonstrated high rate of transmissibility, especially via the respiratory tract and droplet dispersion. Specific recommendations have been established on personal protective equipment (PPE), as well as on airway management related to intubation and mechanical ventilation. Undertaking procedures that generate aerosols involves a high risk of infection and intubation, fibrobronchoscopy and tracheotomy are among the highest risk procedures.9
There are different recommendations as to the technical procedure for tracheotomy in patients with COVID-19, but there is insufficient evidence as to the optimal timing of the procedure, the type of procedure (surgical versus percutaneous tracheotomy) or the subsequent treatment of these patients.
At present, although there are case series describing the experience of tracheotomy in COVID-19 patients, there is insufficient evidence to support firm recommendations, and therefore expert consensus and a literature review in the context of routine practice could help establish guidelines for this procedure in this disease.
The following recommendations are made by the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC), the Spanish Society of Otorhinolaryngology and Head and Neck Surgery (SEORL-CCC) and the Spanish Society of Anaesthesiology and Resuscitation (SEDAR). These recommendations are subject to changes in the scientific evidence and can be adapted to existing resources at any time.
Methodology of the RecommendationsSEMICYUC, SORRL-CCC and SEDAR formed an ad hoc group in light of the COVID-19 pandemic and the need to establish recommendations to help professionals make decisions regarding certain clinical procedures, in this case tracheotomy. A literature search was conducted, and recommendations based on it were drafted by consensus.
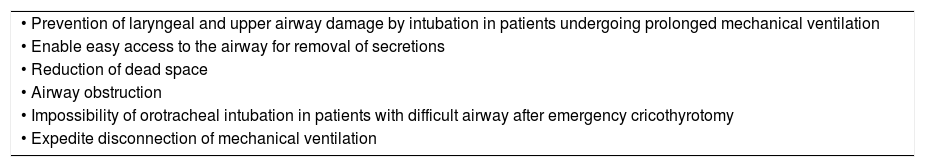
ResultsThe relative indications and contraindications for tracheotomy are described in Tables 1 and 2.
Indications for Tracheotomy in the Intensive Care Unit.10
| • Prevention of laryngeal and upper airway damage by intubation in patients undergoing prolonged mechanical ventilation |
| • Enable easy access to the airway for removal of secretions |
| • Reduction of dead space |
| • Airway obstruction |
| • Impossibility of orotracheal intubation in patients with difficult airway after emergency cricothyrotomy |
| • Expedite disconnection of mechanical ventilation |
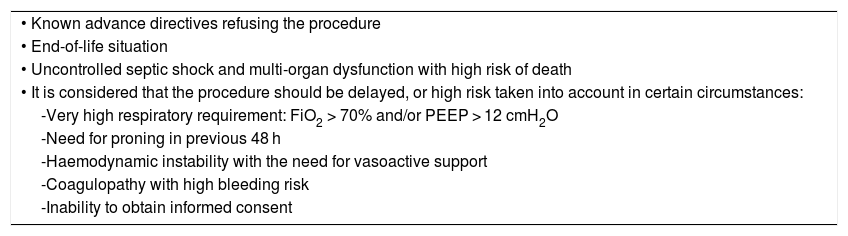
Contraindications for Tracheotomy.
| • Known advance directives refusing the procedure |
| • End-of-life situation |
| • Uncontrolled septic shock and multi-organ dysfunction with high risk of death |
| • It is considered that the procedure should be delayed, or high risk taken into account in certain circumstances: |
| -Very high respiratory requirement: FiO2 > 70% and/or PEEP > 12 cmH2O |
| -Need for proning in previous 48 h |
| -Haemodynamic instability with the need for vasoactive support |
| -Coagulopathy with high bleeding risk |
| -Inability to obtain informed consent |
In routine practice, outside the context of COVID-19, there are no conclusive findings as to the optimal time to perform a tracheotomy in critically ill patients. This is due to the heterogeneity of the patients included in the studies, the different definitions used of early and late tracheotomy, and even defects in the randomisation of patients in the clinical trials conducted. All of this means that the impact on the results of performing tracheotomy in critically ill patients cannot be definitively established. It could be appropriate in the context of COVID-19 patients to define early tracheotomy as that performed in the first 10 days, and late tracheotomy as that performed after that time.
Post-intubation laryngo-tracheal stenosis is a well-known risk of prolonged orotracheal intubation but has not been shown in systematic reviews to significantly reduce in patients treated with early tracheotomy.11,12
It could be that early tracheotomy does not provide benefits in variables such as mechanical ventilation-associated pneumonia or mortality, but it seems reasonable to perform it in patients with a high probability of prolonged mechanical ventilation, because of its benefits over intubation in terms of well-being, ICU stay and time on mechanical ventilation.13 A recent meta-analysis only showed results in reduction of sedative use in relation to the timing of tracheotomy.14
Early tracheotomy may increase the risk of infection in COVID-19 patients and positive PCR with higher viral load. Although the rate of viral clearance is not known exactly, in critical patients it may persist for 2–3 weeks.15 Therefore, there are recommendations from scientific societies that establish negative PCR criteria for the procedure, considering as an exception those patients whose orotracheal intubation does not secure the airway.16,17 In situations where there may be a shortage of certain equipment, such as ventilators, early tracheotomy could increase the availability of these, by reducing days of mechanical ventilation, which would facilitate access to a greater number of patients with an indication for mechanical ventilation. In these circumstances, early tracheotomy may facilitate treatment and nursing care.
In a recent study (data pending publication), tracheotomy has enabled removal of mechanical ventilation an average of 4 days later, in both early (<10 days) and late tracheotomies.
At the other extreme, late tracheotomy can better select patients in whom the procedure is not useful due to subsequent complications, such as dysfunction of other organs that increase the risk of death, or patients with a better prognosis who will progress equally favourably and can be extubated. It appears that patients who do not show clinical or radiological remission within 10 days may be more likely to require continuous ventilation and have a more severe disease course, even death.18
It is recommended that tracheotomy should be performed in patients with a positive PCR for COVID-19 from day 14 of orotracheal intubation, and that early tracheotomy is considered only for stable patients with low oxygen demand, where prolonged mechanical ventilation is planned for other reasons. Early tracheotomy could be considered to optimise intensive care resources.
Surgical Tracheotomy Versus Percutaneous Tracheotomy (PT)With regard to the type of procedure outside the context of COVID-19, it is considered that at the present time there is no evidence to establish recommendations for one tracheotomy method over others. The selection of one or another method can only be made on the basis of clinical criteria, experience and availability. In the current situation of high care burden, where intensive care resources are scarce, surgical tracheotomy performed by specific surgical teams may favour the procedure and avoid unnecessary delays. We recommend considering open tracheotomy or percutaneous tracheotomy (PT) at the discretion of the multidisciplinary team, according to the experience of the centre and the availability of the various resources. In the event that PT is chosen, based on experience and in a multidisciplinary team, the considerations already known should be considered.
Although the use of fibrobronchoscopy could reduce the risks related to PT,19 it would be inadvisable for COVID-19 patients, since it increases the number of participants and is a high-risk procedure for generating aerosols. If it is considered, it is recommended to use parts that produce a seal at the tube inlet and to evaluate the use of disposable fiberscopes.20,21
In these cases, although there is insufficient evidence to recommend its use, in order to reduce complications associated with the procedure, ultrasound may be useful to improve accuracy at the puncture site in patients who present difficulty in identifying anatomical structures.22
In both cases, care should be taken to clean the equipment used according to the established recommendations.
In necks without significant anatomical abnormalities, percutaneous tracheotomy may be considered the technique of choice taking previous recommendations into account and the availability of trained professionals to perform it. The surgical technique, as opposed to percutaneous, would provide a more controlled and rapid approach to the airway in a patient at high risk of complications.23 It could be considered in the phases of the pandemic where there is the greatest burden on intensive care professionals.
Where the Tracheotomy Procedure Should Be PerformedBed-side PT reduces the need to move and disconnect mechanical ventilation if it can be performed in individual or negative pressure rooms.
It is recommended that the tracheotomy be performed in an ICU cubicle or nearby location (such as the operating theatre) that has an isolation and negative pressure system, with appropriate equipment for the procedure. It is not recommended that tracheotomy be performed in COVID-19 cohort spaces without isolation cubicles. If performed in the operating theatre, specific considerations should be made, with areas marked for circulation of patients and for carrying out the procedure.24
Surgical Technique25–28General Recommendations- •
Use of standard surgical tracheotomy material.
- •
As far as possible, limit the use of electrical, ultrasound or any other cutting and coagulation systems that can spread airborne macroparticles. Preferably use cold material and conventional haemostasis systems, unless it is considered that this will entail excessive delay in performing the technique.
- •
Use closed circuit suction systems with anti-viral filters.
- •
The number of personnel required for the technique must be kept to a minimum.
- •
Tracheotomy should be performed by the most experienced personnel available in the minimum time possible.
- •
Use appropriate protective measures. PPE: disposable, waterproof gown, cap and footwear; disposable, plastic, full-face, waterproof eye and face shield; FFP2 or FFP3 or equivalent (N95) protective mask and surgical mask overlay. Preferably use double surgical gloves.
- •
Goggles, coveralls and similar are usually waterproof systems. It is advisable to use anti-fogging or similar.
- •
Choose between percutaneous or standard surgical tracheotomy principally depending on the centre’s usual protocol.
- 1
Before opening the trachea:
- •
Establish adequate pre-oxygenation of the patient (100% oxygen, 5 min).
- •
Complete muscle relaxation of the patient during the entire procedure and especially at the time of withdrawal from intubation and decannulation, to prevent coughing and aerosolization.
- •
Before tracheal opening, mechanical ventilation should be removed.
- •
- 2
Perform the tracheotomy, withdraw the endotracheal intubation tube until the balloon cannula can be placed without removing it completely; inflate the cannula balloon.
- 3
Connect the ventilator and, when correct ventilation has been checked (preferably by capnography), withdraw the endotracheal tube and fix the tracheotomy cannula with tape and silk stitches. Never deflate the tracheotomy tube balloon once mechanical ventilation has begun.
- 4
Collect all the tracheotomy material.
- 5
Remove the protective equipment from the surgeon in the operating theatre or room according to current regulations.
- 6
Leave the operating theatre or room according to the regulations.
On occasion, as determined by the patient's ventilatory deterioration, tracheotomy may be required in emergency situations in previously unintubated patients. In these cases, a cricothyrotomy may be necessary by means of a set pre-designed for this purpose.
Emergency tracheotomy should be avoided as far as possible because it is performed under conditions that are not ideal. Good communication with the intensive care, anaesthesia and emergency services is recommended, and offer help with intubations expected to be difficult.
- 1
Establish appropriate pre-oxygenation of the patient (oxygen at 100%, 5 min).
- 2
Full muscle relaxation to prevent patient movement, as well as coughing.
- 3
Place the tracheotomy cannula and inflate the balloon.
- 4
Switch on the mechanical ventilator and stabilise the patient.
- 5
Attach the cannula.
- 6
If tracheotomy is not possible, a cricothyrotomy will be performed according to the standard technique.
- 7
If a cricothyrotomy has been performed, once the patient has been stabilised and the airway secured, a surgical tracheotomy will be performed using a different incision. The cricothyrotomy incision will be closed after removal of the previous cannula and placement of the cannula in the tracheotomy.
- 8
Same as points 4–6 above (elective tracheotomy).
The care of tracheostomised COVID-19 patients may increase exposure of healthcare workers to infection and the spread of infection.
- •
Place patients in cohort areas according to COVID-19 and the risk of contagion.
- •
Preferably in single and negative pressure rooms, if available.
- •
The appropriate use of PPE during care of tracheotomy patients should always be indicated for procedures with a risk of generating aerosols, especially in those who remain PCR positive; this includes the use of a waterproof gown, respiratory protection with FPP2 or FFP3 mask, splash protection and the use of gloves. Correct hand hygiene is essential before putting on and removing PPE.10
- •
In tracheostomised patients a surgical mask will be placed over the tracheostoma or over nasal goggles or oxygen mask if the tracheotomy is closed.
- •
In life-threatening emergencies, priorities should be given to placement of PPE and seeking help.
- •
Extra PPE should be available in tracheostomised patient areas.
- •
Minimise handling of the tracheotomy and the number of professionals involved.
- •
Consider delaying the first change of tracheotomy tube and make subsequent changes after the virus detection test is negative.
- •
The use of internal cannulas should always be considered.
- •
Always keep the balloon inflated.
- •
Use closed suction systems.
- •
Adjust the frequency of liner change or cleaning the tracheostoma, assessing risks and benefits.
- •
Avoid active humidification and assess the risks and benefits in relation to obstruction of the cannula.
- •
Use high-efficiency antimicrobial filters and heat exchangers to disconnect mechanical ventilation.
- •
Preferably avoid T-tubes, fenestrated cannulas and deflating the balloon until the virus detection test is negative.
- •
Multidisciplinary teams trained in the handling of tracheostomas are recommended for the care of these patients.
- •
Specific equipment should be available to redo the tracheotomy in case of decannulation failure.
- •
There must be an alarm system to the ENT department.
- •
PPE can make vision and communication between the team difficult. Tracheostomy procedures should be anticipated, and short briefing sessions should be held.
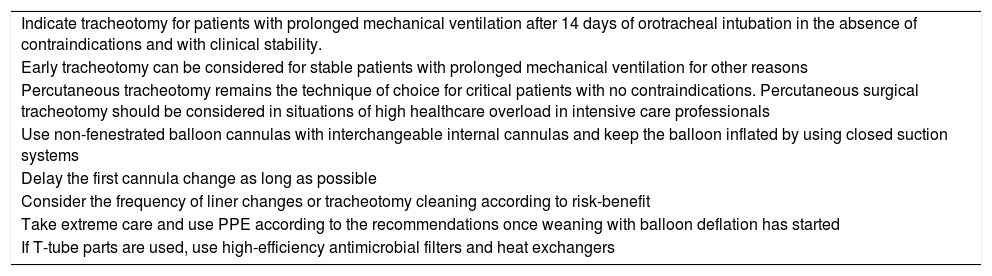
Table 3 summarises the main conclusions of the consensus on tracheotomy in COVID-19 patients.
Tracheostomy Recommendations for COVID-19 Patients.
| Indicate tracheotomy for patients with prolonged mechanical ventilation after 14 days of orotracheal intubation in the absence of contraindications and with clinical stability. |
| Early tracheotomy can be considered for stable patients with prolonged mechanical ventilation for other reasons |
| Percutaneous tracheotomy remains the technique of choice for critical patients with no contraindications. Percutaneous surgical tracheotomy should be considered in situations of high healthcare overload in intensive care professionals |
| Use non-fenestrated balloon cannulas with interchangeable internal cannulas and keep the balloon inflated by using closed suction systems |
| Delay the first cannula change as long as possible |
| Consider the frequency of liner changes or tracheotomy cleaning according to risk-benefit |
| Take extreme care and use PPE according to the recommendations once weaning with balloon deflation has started |
| If T-tube parts are used, use high-efficiency antimicrobial filters and heat exchangers |
All these recommendations are based on evidence and the current knowledge of the specialists involved regarding acute respiratory failure secondary to COVID-19 pneumonia, and some indications are likely to change or need to be adapted to the resources available in care centres during the course of the pandemic.
Conflict of InterestsThe authors have no conflict of interests to declare.
Rosa Villalonga Vadell and María Cruz Martín Delgado have contributed equally as senior authors.
Please cite this article as: Bernal-Sprekelsen M, Avilés-Jurado FX, Álvarez Escudero J, Aldecoa Álvarez-Santuyano C, de Haro López C, Díaz de Cerio Canduela P, et al. Documento de consenso de la Sociedad Española de Medicina Intensiva, Crítica, y Unidades Coronarias (SEMICYUC), la Sociedad Española de Otorrinolaringología y Cirugía de Cabeza y Cuello (SEORL-CCC) y la Sociedad Española de Anestesiología y Reanimación (SEDAR) sobre la traqueotomía en pacientes con COVID-19. Acta Otorrinolaringol Esp. 2020. https://doi.org/10.1016/j.otorri.2020.04.002
This article is published simultaneously in Medicina Intensiva (https://doi.org/10.1016/j.medin.2020.05.001), in Acta Otorrinolaringologica Espanola (https://doi.org/10.1016/j.otorri.2020.04.002) and in Revista Española de Anestesiología y Reanimación (https://doi.org/10.1016/j.redar.2020.05.001), with the consent of the authors and editors.