Periprosthetic leakage of liquids is a common complication in patients rehabilitated with voice prostheses. Our objective was to describe and review the results of procedures for treating periprosthetic leakage.
Materials and methodsThis was a retrospective analysis of 41 patients rehabilitated with Provox® 2 voice prostheses between 1997 and 2015. We describe 3 techniques: periprosthetic silicon collar placement, injection of hyaluronic acid into the tracheoesophageal wall and the combination of the 2 techniques. We present a method to reduce the diameter of the tracheoesophageal fistula by removing the voice prosthesis and placing a nasogastric tube through the fistula.
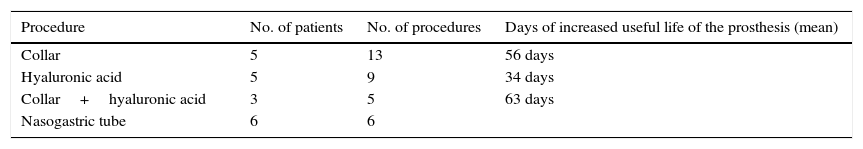
ResultsIn the 3 groups treated with silicone collar (n=5, 13 procedures), hyaluronic acid injection (n=5, 9 procedures) and the combination of both techniques (n=3, 5 procedures), we observed an increase in prosthesis lifespan of an average of 56 days (range 7–118 days), 32 days (range 3–55 days) and 63 days (range 28–136 days), respectively. The tracheoesophageal fistula diameter reduction was performed in 100% (n=6) of patients.
ConclusionsThe use of silicone collars, injection of hyaluronic acid into the tracheoesophageal wall and the combination of both techniques for the treatment of periprosthesis leakage increase the lifespan of the prosthesis. Temporary prosthesis removal and placement of nasogastric tube has also been shown effective in our experience. These techniques are simple, inexpensive and reproducible, thereby reducing healthcare costs.
La fuga periprótesica de líquidos es una complicación frecuente en pacientes rehabilitados con prótesis fonatorias. Nuestro objetivo es describir y revisar los resultados de procedimientos para el tratamiento de la fuga periprotésica.
Materiales y métodosAnálisis retrospectivo de 41 pacientes rehabilitados con prótesis fonatorias Provox® 2 entre 1997 y 2015. Descripción de 3 técnicas: colocación de arandela de silicona periprótesis, inyección de ácido hialurónico en la pared traqueal y la combinación de ambas técnicas. Se presenta un método para reducir el diámetro de la fístula fonatoria mediante retirada de la prótesis y colocación de sonda nasogástrica a través de la fistuloplastia.
ResultadosEn los 3 grupos tratados mediante arandela de silicona (n = 5, 13 procedimientos), inyección de ácido hialurónico (n = 5, 9 procedimientos) y la combinación de ambas técnicas (n = 3, 5 procedimientos), observamos un aumento de la vida útil de las prótesis en una media de 56 días (rango 7 a 118 días), 32 días (rango de 3 a 55 días) y 63 días (rango 28 a 136 días) respectivamente. La reducción del diámetro fistuloplastia se produjo en el 100% (n = 6) de los pacientes tratados.
ConclusionesEl uso de arandelas de silicona, inyección de ácido hialurónico en la pared traqueoesofágica y la combinación de ambas técnicas, para el tratamiento de la fuga periprótesis de líquidos aumenta la vida útil de las prótesis. La retirada protésica temporal y la colocación de sonda nasogástrica también se ha mostrado efectiva en nuestra experiencia. Estas técnicas son sencillas, económicas y reproducibles y reducen el gasto sanitario.
Total laryngectomy is routine treatment for advanced laryngeal carcinomas. It is intensive treatment that involves loss of larynx sphincter, voice1,2 and olfactory function. These patients also present difficulties in undertaking some physical activities and any activity which involves immersion in water, which has a major impact on their quality of life.2 Voice rehabilitation plays an important role in restoring these patients’ quality of life and social life. Many voice rehabilitation methods have been described, including erygmophony and electric laryngophones1 as non-invasive methods. The most accepted surgical method today is the creation of a tracheoesophageal fistula and the use of voice prostheses. This technique enables the ability to talk to be restored in a few days after surgery and therefore the patient's quality of life improves rapidly.3 However, there are several routine complications with the use of voice prostheses, the most common being leakage of fluids.4 The practitioner should be able to distinguish between central leakage, through the prosthetic valve which indicates that it is incompetent and therefore a change of prosthesis is required, from periprosthetic leakage which is caused by the prosthesis and the tracheoesophageal fistula being mismatched in diameter. In both cases, leakage of fluids results in aspiration with the consequent increased risk of lung infections. In this article we propose various simple, low cost and non-invasive techniques which might increase the useful life of voice prostheses after periprosthetic leakage.
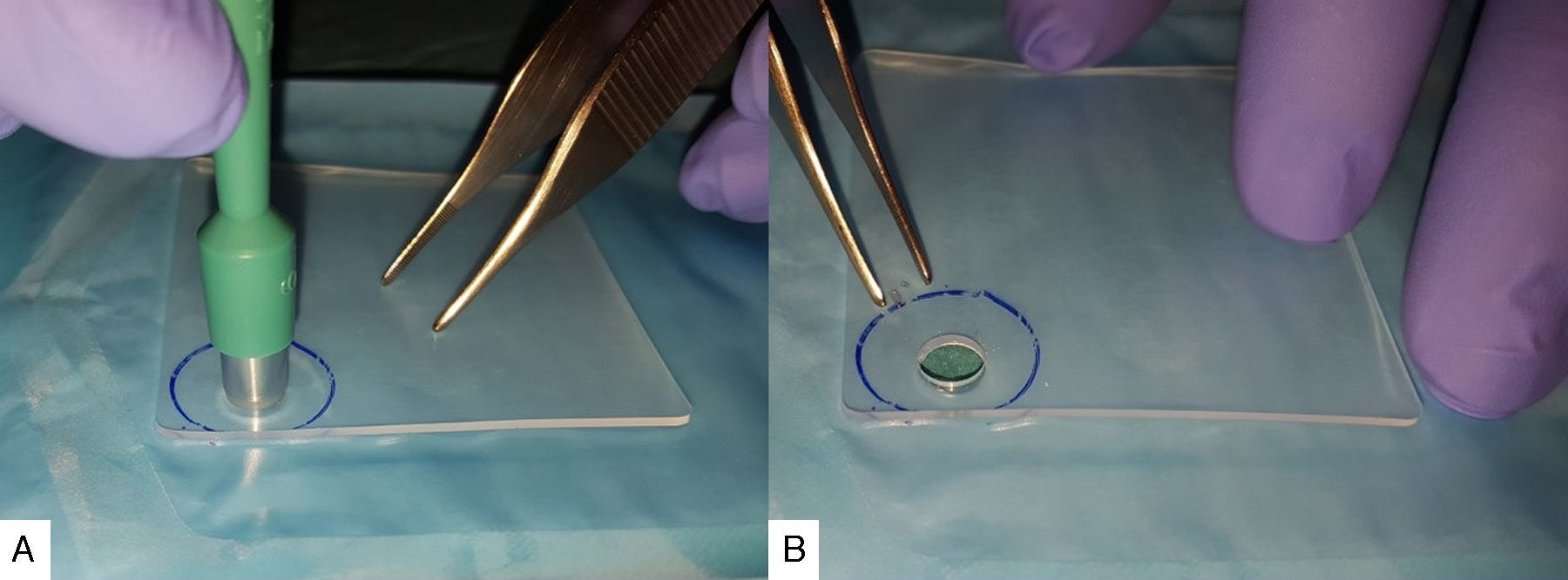
Material and MethodsWe performed a retrospective study reviewing the clinical histories of patients who had undergone total laryngectomy under voice rehabilitation with Provox® 2 (Atos Medical) type prostheses between 1997 and 2015. Our series includes 41 patients who were appropriately followed-up. Thirty-seven males (90.2%) and 4 females (9.7%) with an average age at which they underwent the fistuloplasty of 61 years (range from 37 to 74). A total of 42 tracheoesophageal fistulae were created of which 37 (88%) were primary and 5 (11.9%) secondary. In one case, the primary tracheoesophageal fistula was closed and a new secondary fistulaplasty created subsequently. A total of 286 prosthesis changes were recorded with an average duration of 206 days (range 5–602 days). Seventeen (41.4%) of the patients were treated with radiotherapy, 11 of them (26.8%) underwent this treatment prior to the creation of their tracheoesophageal fistula and the remaining 6 (14.6%) received radiotherapy as complementary treatment to surgery. A silicone collar was placed in five patients (13 occasions in total) around the prosthesis when the periprosthetic leakage was detected. The collar was designed using a sheet of silicone (Medtronic), 1mm thick, marking a circle of around 3cm in diameter on the sheet. Then, using a 6mm skin biopsy punch (Kai Medical), the centre of the circle was perforated to create a central orifice (Fig. 1). The collar was cut out and placed around the tracheal end of the prosthesis in order to eliminate the dead space between the voice prosthesis and the fistuloplasty through which the leakage was taking place. After periprosthetic leakage had been detected, five patients (9 occasions in total) were injected with hyaluronic acid (Macrolane® Galderma) into the tracheoesophageal wall at various points around the fistula which had been observed to be leaking in order to reduce the diameter of the fistuloplasty. A combination of the two aforementioned techniques was used in 3 patients (5 occasions in total) (Fig. 2A). On 6 occasions, the voice prosthesis was removed in patients who presented a clear increase in the diameter of their voice fistula, and a nasogastric tube, 4mm in diameter placed through the fistula (Fig. 2B). The patient was given an appointment 7 days later to replace the prosthesis after confirming that the diameter of the fistuloplasty had reduced.
In the postoperative period, 37 patients (90.2%) managed to use their prostheses successfully. With regard to managing periprosthetic leakage, the group treated with silicone collar alone achieved an increase in the useful life of their prosthesis of a mean 56 days (range from 7 to 118 days). The group treated with hyaluronic acid injection in the tracheoeosophageal wall had an increased useful life of a mean of 32 days (range from 3 to 55 days). In the group treated with both methods, the prosthesis remained competent for a mean of 63 days (range from 28 to 135 days). Placement of a nasogastric tube through the fistula to reduce the diameter of the fistula proved satisfactory in the 6 cases where this was performed (100%) and enabled a new prosthesis to be placed without detecting any leakage (Table 1).
DiscussionVoice rehabilitation in laryngectomised patients using voice prostheses is common practice, with satisfactory results achieving high percentages of voice production after surgery.3 Trans and periprosthetic leakage of liquids, granulation tissue growth and colonisation by Candida spp. are the most commonly observed complications.4,5 While leakage of transprosthetic liquids requires the prosthesis to be changed, periprosthetic leakage is more complex to manage as the diameter of the fistula and that of the prosthesis are mismatched. Op de Coul et al.5 in a series of 318 patients using a Provox® prosthesis report perisprosthetic leakage in 18% of patients. Imre et al.6 observed an increase in the diameter of the tracheoesophageal fistula in 19.1% of their patients. The aetiology of the increase in fistula diameter has not been completely clarified. Possible causes include atrophy of the perifistula tissue as a consequence of radiotherapy, trauma to the free edge of the fistula due to micromovements of the prosthesis, the procedures for changing the prosthesis or organic alterations as a consequence of gastroesophageal reflux.7
Bunting et al.8 described the use of periprosthetic silicone collars in the tracheal end of the prosthesis for the first time in 2004. Hilgers et al.9 placed silicone collars 0.5mm thick in 107 patients and reported control of leakage in 88% of their patients with a mean duration of the prosthesis of almost 2 months. The use of silicone collars adapted to the oesophageal end of the prosthesis has also been described.7 These collars increase the tracheal and/or oesophageal surface of the ends of the prosthesis which encourages better sealing of the fistula. There are products on the market to prevent periprosthetic leakage such as Provox® Xtraflange, but in our experience these are of limited use due to their lack of thickness. Designing a silicone collar using the aforementioned method is simple, economical, safe and effective, with the great advantage of being a non-invasive technique. Collars can be placed easily in the surgery or even in the emergency department as the procedure only requires topical anaesthesia to prepare the patient.
The injection of various materials into the tracheoesophagial wall is described in the literature. The most commonly used of these materials are autologous centrifuged fat and collagen.7 In 1999, Luff et al.10 published for the first time a case of a patient who was rehabilitated with a Provox® 2-type prosthesis with untreatable leakage that was injected with hyularonic acid in order to adapt the wall to the diameter of the prosthesis with a good result. Our experience was satisfactory on 9 occasions and we consider that the injection of hyaluronic acid, under topical anaesthesia is a useful and minimally invasive technique which has proved effective, increasing the useful life of our patients’ prostheses by a mean of 32 days.
The combination of hyaluronic acid injection and placing a collar has not been described before in the literature. Despite the limited number of occasions that we have performed this technique, because of its good results we believe it could be another tool to be considered in the management of persistent periprosthetic leakage.
For periprosthetic leakage resistant to the aforementioned techniques and especially for very wide fistuloplasties, removal of the prosthesis and the placement of a nasogastric tube through the fistuloplasty is a reasonable alternative. In the literature, several authors propose removing the prosthesis for 14 days in an attempt to reduce the diameter of the fistuloplasty with the consequent risk of its complete closure.7,11 In our opinion it is important to place a nasogastric tube through the fistuloplasty in order to prevent excessive or even complete closure of the fistula. On the 6 occasions that we have performed this procedure we have achieved satisfactory and lasting results.
ConclusionsPeriprosthetic leakage of liquids is a common complication in patients who use voice prostheses. This complication requires different management to others that are resolved by a change of prosthesis. The use of collars improves the sealing of the prosthesis at the tracheal and/or oesophageal end, reducing the existing space between the trachea or the oesophagus and the prosthesis and also increasing the contact surface between both. It is easy to reproduce these devices in-house, they are economical, easy to place and cause the patient minimum discomfort. Hyaluronic acid injection in the tracheoesophageal wall increases the wall volume and enables it to adjust better to the diameter of the prosthesis. The combination of both techniques is also effective for treating periprosthetic leakage. In cases of leakage that is resistant to the aforementioned treatments and in cases of increased fistuloplasty diameter, it is possible to reduce the diameter by removing the fistula, minimising the risk of excessive or complete closure by placing a nasogastric tube through the fistula. These procedures extend the useful life of voice prostheses reducing the healthcare costs of managing these patients.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Friedlander E, Pinacho Martínez P, Poletti Serafini D, Martín-Oviedo C, Martínez Guirado T, Scola Yurrita B. Manejo práctico de fugas periprótesis en pacientes rehabilitados con prótesis fonatorias tipo Provox®2 tras laringectomía total. Acta Otorrinolaringol Esp. 2016;67:301–305.