This was a 77-year-old woman from Argentina, specifically from a rural area in the north of the country, on the border with Bolivia. She attended the Accident and Emergency Department following years of persistent constipation that had been increasing over the last few months to the point of significantly limiting her quality of life. She reported being asymptomatic in the case history and anamnesis.
Although the patient presented with no cardiovascular symptoms, she was followed up for mild mitral and tricuspid regurgitation with biannual follow-up echocardiograms.
On arrival, the patient's blood pressure was 97/70mmHg and her heart rate was 74 bpm. Physical examination showed no pathological signs, only abdominal discomfort, with palpation of a mass in the mesogastric region. She exhibited no stigmata of cardiac decompensation.
Blood tests showed no leukocytosis or elevation of acute-phase reactants, with haemoglobin 12.4g/dl, MCV 94.1fl (78–100), MCH 31pg (27–32), normal platelet count and coagulation parameters in normal range. Renal function and ions were also not significantly abnormal. Liver profile and amylase were normal.
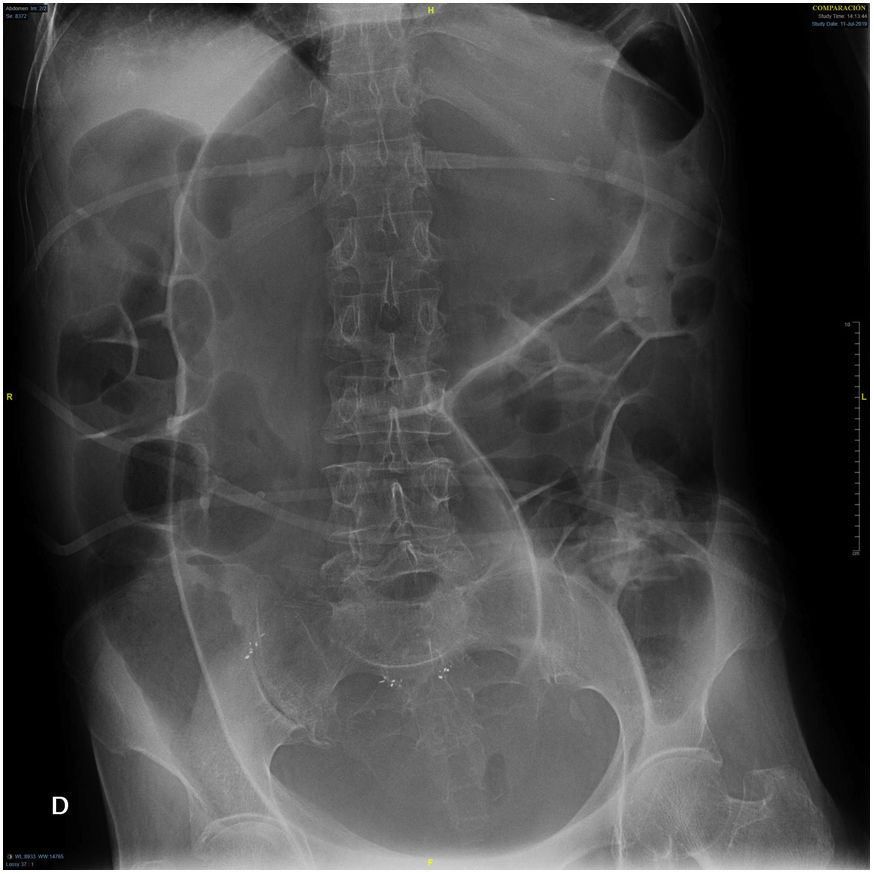
An abdominal X-ray was performed (Fig. 1), shown below. The objective findings allowed a diagnosis of certainty to be made.
Clinical course and diagnosisThe abdominal X-ray showed megacolon, without clear signs of intestinal obstruction.
Given the geographical origin and the findings, the differential diagnosis included Chagas disease and other possible causes of megacolon such as neurological disorders (Parkinson's disease, diabetic neuropathy), metabolic or autoimmune disorders such as systemic sclerosis. Other possibilities considered were toxic megacolon and mechanical obstruction.
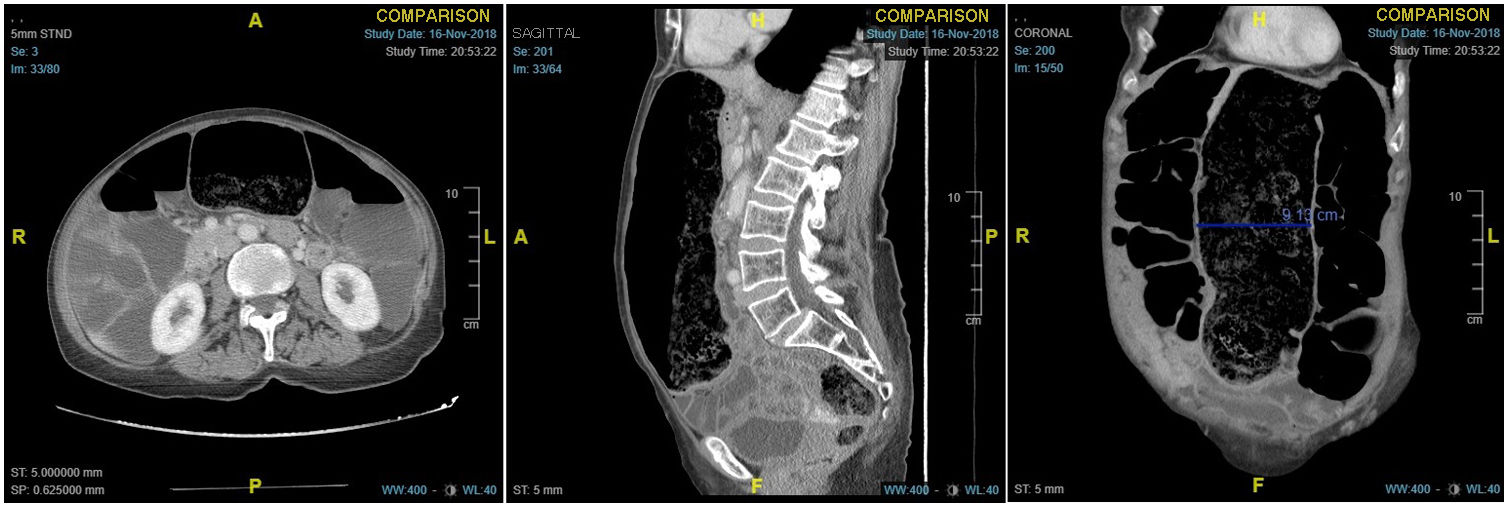
The study was completed with serology and PCR for Trypanosoma cruzi, the former being positive (ELISA and indirect immunofluorescence) and the latter negative. Transthoracic echocardiography showed no pathological findings. Oesophagogastroduodenal transit showed no morphological abnormalities, although there was a modest decrease in oesophageal peristalsis. The barium enema showed increased sigmoid calibre with loss of haustration. Finally, abdominal computed tomography (Fig. 2) showed severe dilatation of the entire colon, predominantly in the sigmoid, with no involvement of other organs.
With the diagnosis of chronic Chagas disease with gastrointestinal involvement and despite the advanced stage at diagnosis, benznidazole was administered for 60 days. Constipation became increasingly pronounced and unmanageable. Probably because of the patient's very phlegmatic diagnosis, she finally had to undergo a total colectomy with ileostomy, with the subsequent implications that surgery of this magnitude can have (in our case, severe malnutrition).
Chagas disease is a parasitic disease endemic to Latin America caused by Trypanosoma cruzi. According to the latest estimates, some six million people are infected. Due to globalisation, American trypanosomiasis is also becoming a health problem in non-endemic countries. A high level of suspicion is therefore necessary in patients from endemic areas who consult for cardiac or gastrointestinal symptoms, as in the case of our patient.
The infection has a biphasic course, with an initial acute parasitaemic phase which, if untreated, progresses to a chronic phase that in about 10–30 years leads to visceral cardiac (15%–45%) or gastrointestinal (10%–21%) involvement.
Gastrointestinal manifestations vary according to the area of origin, and appear in relation to the denervation of the enteric nervous system, producing megaviscera (megacolon 70%–87% with preferential involvement of the sigmoid, oesophageal disease 16%–30%). Some studies have investigated the influence of the microbiota on susceptibility, progression and response to parasiticides in this disease.1
In the initial evaluation of these patients, it is advisable to screen for cardiovascular disease with an echocardiogram in addition to dynamic gastrointestinal tests.
The benefits of administering antitrypanosomal treatments (benznidazole and nifurtimox) in the chronic phase are disputed given the lower parasite cure rates achieved and that sometimes organ damage is sufficiently established compared to the benefit to be gained from treatment with a significant incidence of side effects. Surgical treatment is rare and the main indication is for severe persistent constipation refractory to treatment, or secondary complications.2 The most commonly-performed surgery is anterior rectosigmoidectomy, while total colectomy is rare (around 5%–6% according to some series).3
In conclusion, there should be high clinical suspicion in patients from an endemic area consulting for symptoms. Early treatment can prevent later complications that are very difficult to manage. Every late diagnosis is a missed opportunity.