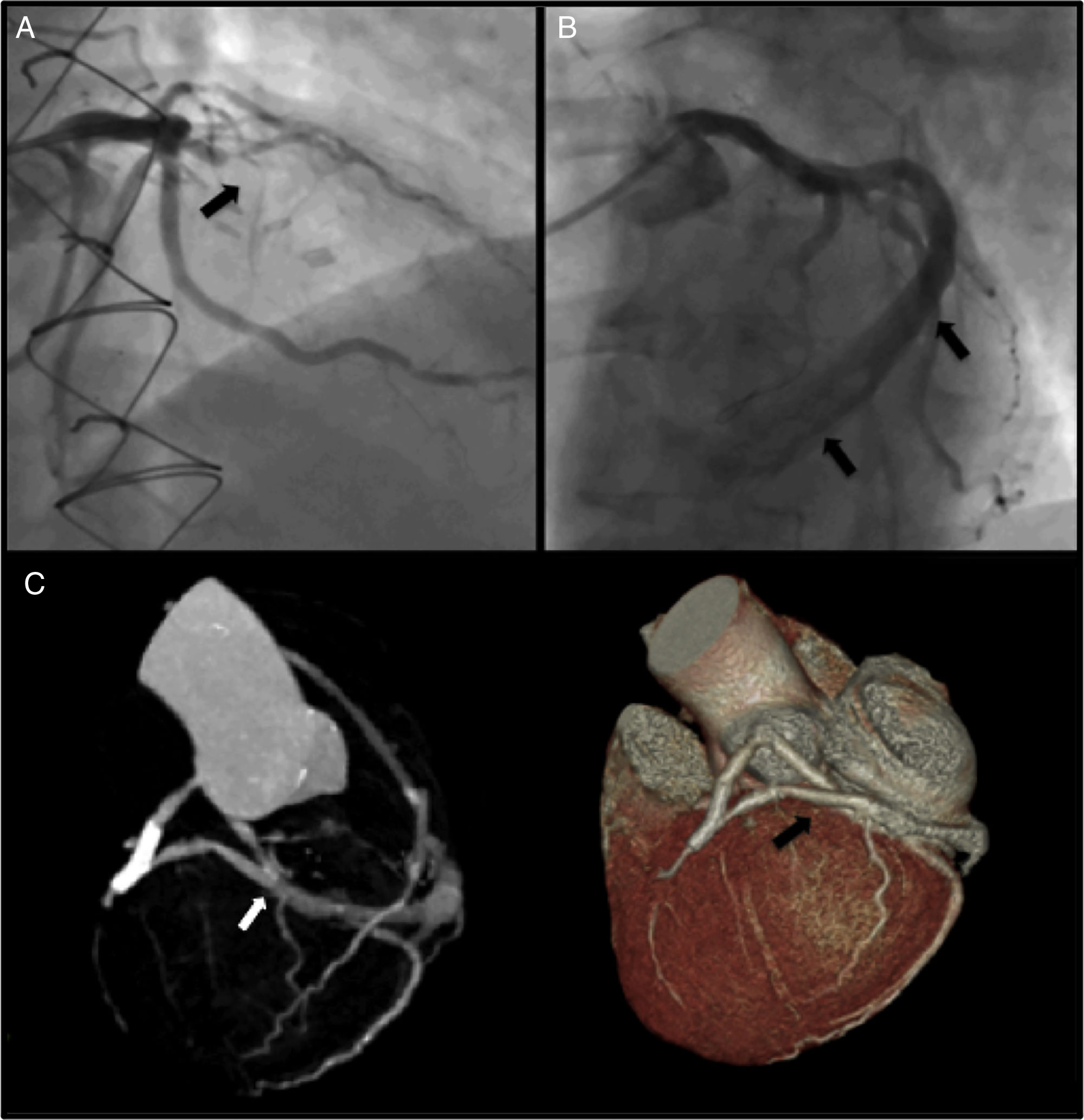
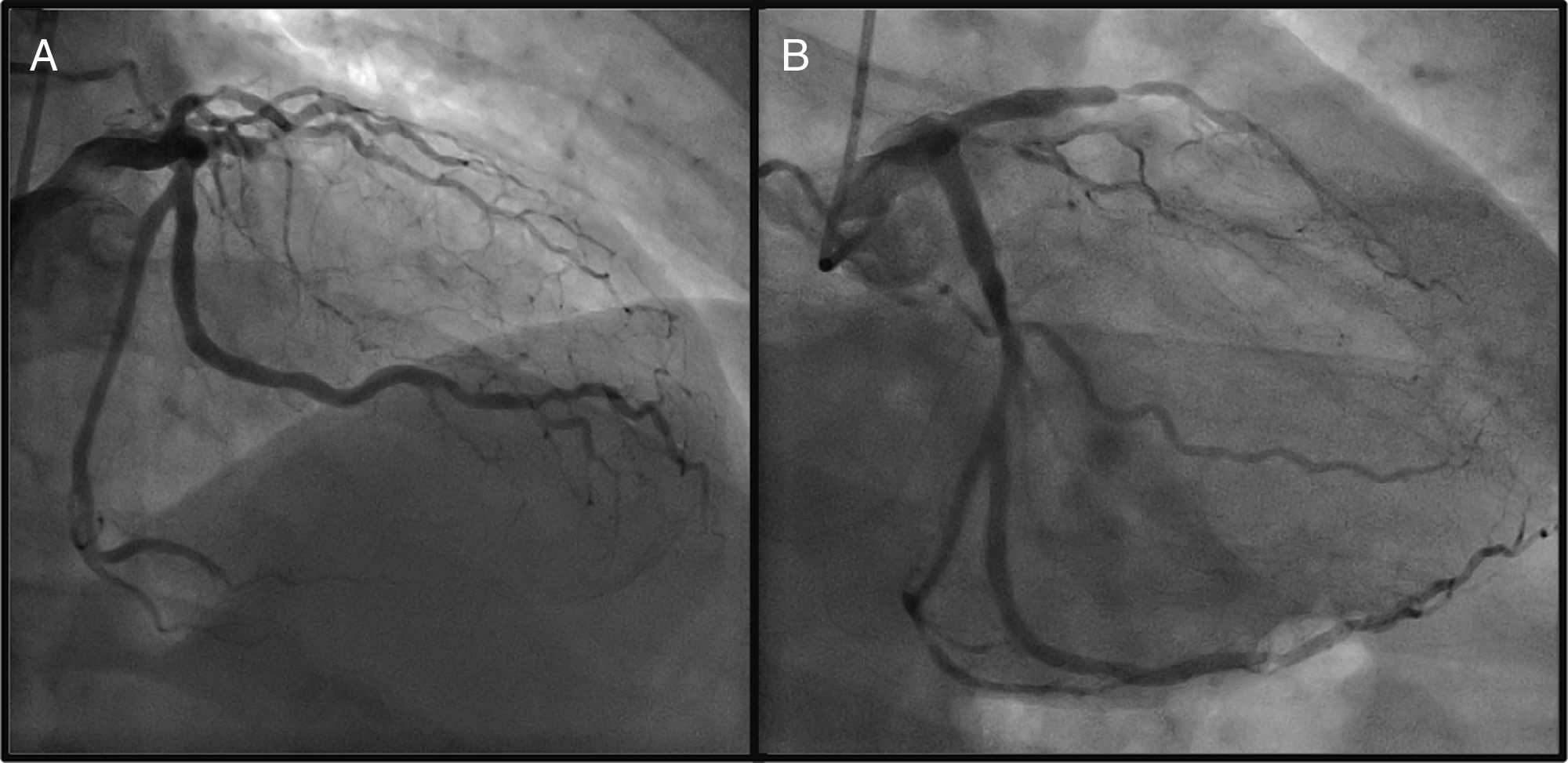
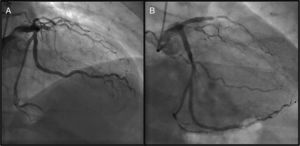
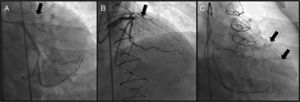
A 64-year-old Caucasian male with a history of coronary artery bypass grafting (CABG) [internal mammary artery (IMA) graft to the left anterior descending artery (LAD) and saphenous vein graft to right posterior descending artery (PDA)], presented with stable angina with a positive treadmill exercise test. Coronary angiography (CAG) documented occlusion of both middle LAD and IMA grafts (Figure 1, panel A); no significant lesions were found in the circumflex artery or the saphenous vein graft. The CAG performed prior to surgery is shown in Figure 2.
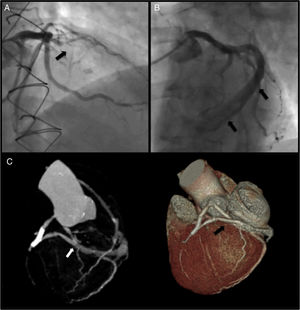
Panel A: coronary angiography (right cranial view) showing LAD occlusion; Panel B: large caliper vessel uncovered after LAD balloon pre-dilatation (left cranial view); Panel C: documentation of a fistula from the middle segment of the LAD into the coronary sinus by CT angiography.
After a myocardial perfusion scintigraphy confirming viability in LAD territory, an angioplasty was performed. A new large vessel was visible after mid-LAD dilatation (Figure 1, panel B, supplementary film 1). The images were suggestive of a fistula or a shunt. A 4.0×18-mm drug-eluting stent was successfully implanted. The patient remained stable throughout the procedure.
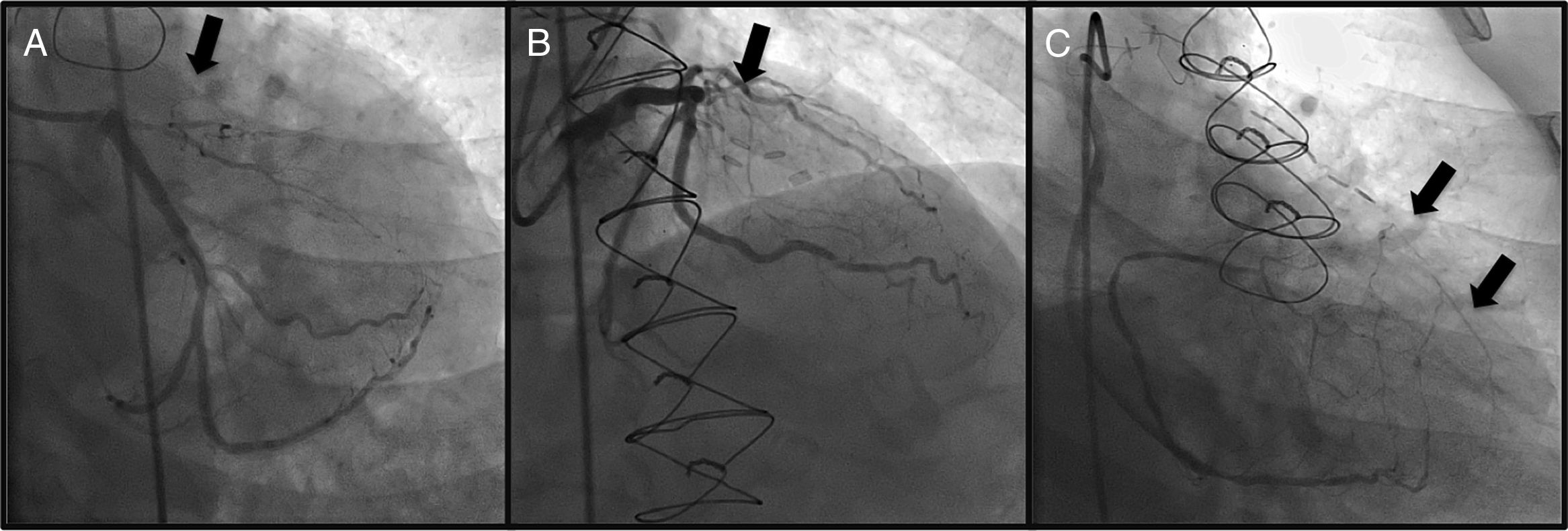
CT angiography showed a fistula from the middle segment of the LAD to the coronary sinus (Figure 1, panel C). Excluding the fistula by implanting a covered stent was then considered. However, when performing the initial CAG, complete stent restenosis had occurred, resulting in both LAD and fistula occlusion (Figure 3). A silent infarction had probably occurred. A new ischemia test was performed, documenting necrosis without viability. A conservative approach was therefore chosen.
Coronary artery fistulas (CAFs) are uncommon. Acquired fistulas are even rarer, and may occur after cardiac trauma, angioplasty, endomyocardial biopsies or cardiac surgery. We describe the rare case of fistula development after CABG. Although the majority of patients are asymptomatic, they can present with angina pectoris or myocardial infarction. In this particular case, due to steal phenomenon, this acquired CAF may have led to both IMA graft and LAD occlusion. Treatment should be considered for symptomatic patients or documented ischemia. Options range from a conservative approach to coil embolization, PTFE stent deployment or surgery.
Conflict of interestsThe authors have no conflicts of interest to declare.