Wegener's granulomatosis is an autoimmune disease that may present as necrotising granulomatosis, vasculitis of the upper and lower respiratory tract, necrotising glomerulonephritis and diffuse vasculitis, mainly affecting the lungs, airway, and kidney.1 When the lung is affected, the clinical manifestations are nonspecific and include coughing, dyspnoea, and haemoptysis. Plain chest radiology usually shows areas of consolidation or single or multiple nodules, which are asymptomatic in a third of the affected patients. Cavitation of these nodules is common because of central necrosis. When this phenomenon affects the visceral pleura, a bronchopleural fistula occurs and pneumothorax or pyopneumothorax can appear. This complication is extremely rare and only 9 cases have been reported in literature worldwide.2,3 We present the case of a patient with pyopneumothorax due to Wegener's granulomatosis and its surgical resolution, treated in the Thoracic Surgery Department of our hospital.
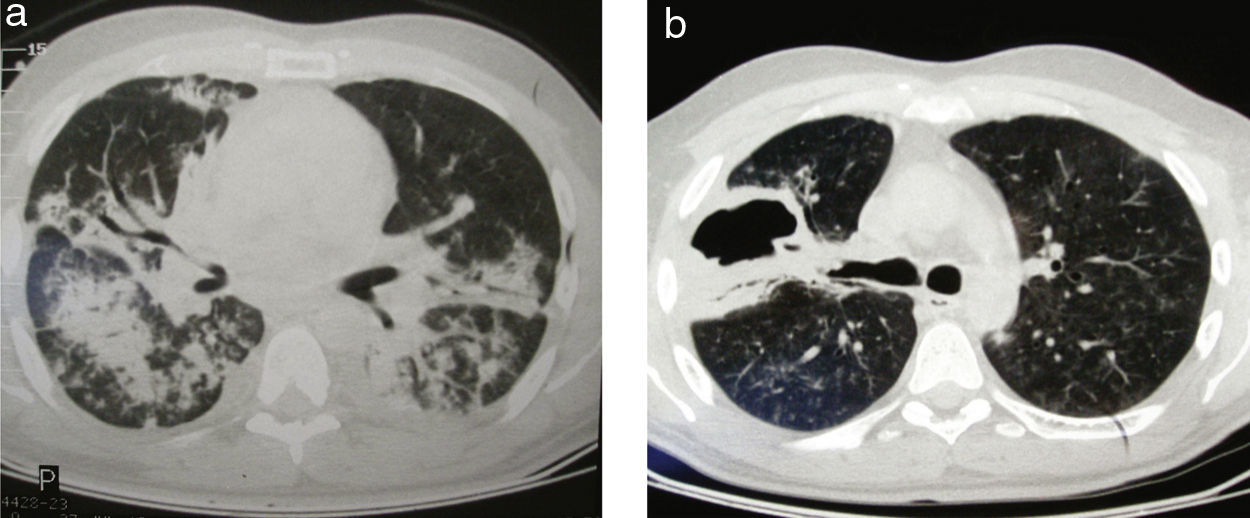
We report the case of a 35-year-old male patient who was admitted to the Internal Medicine Department for symptoms of fever associated with coughing and purulent sputum. A chest X-ray showed a right basal opacity and the initial diagnosis was community-acquired pneumonia. Forty eight hours after admission, the patient presented clinical deterioration with poor ventilatory mechanics, and required transfer to the intensive care unit and mechanical ventilation. A twenty point fall in haematocrit levels and associated kidney failure were found. C-ANCA and proteinase 3 were requested, which were positive, and the presumptive diagnosis of Wegener's granulomatosis was made. Treatment was started with 500mg of cyclophosphamide and plasmapheresis was carried out. The cough and mucopurulent sputum persisted, and chest axial CT scan was performed, which displayed predominantly right bilateral basilar infiltrates (Fig. 1a). Antibiotic treatment with vancomycin, meropenem, and colistin was started. Plasmapheresis was recommenced and due to a favourable response the patient was transferred to the general medical ward.
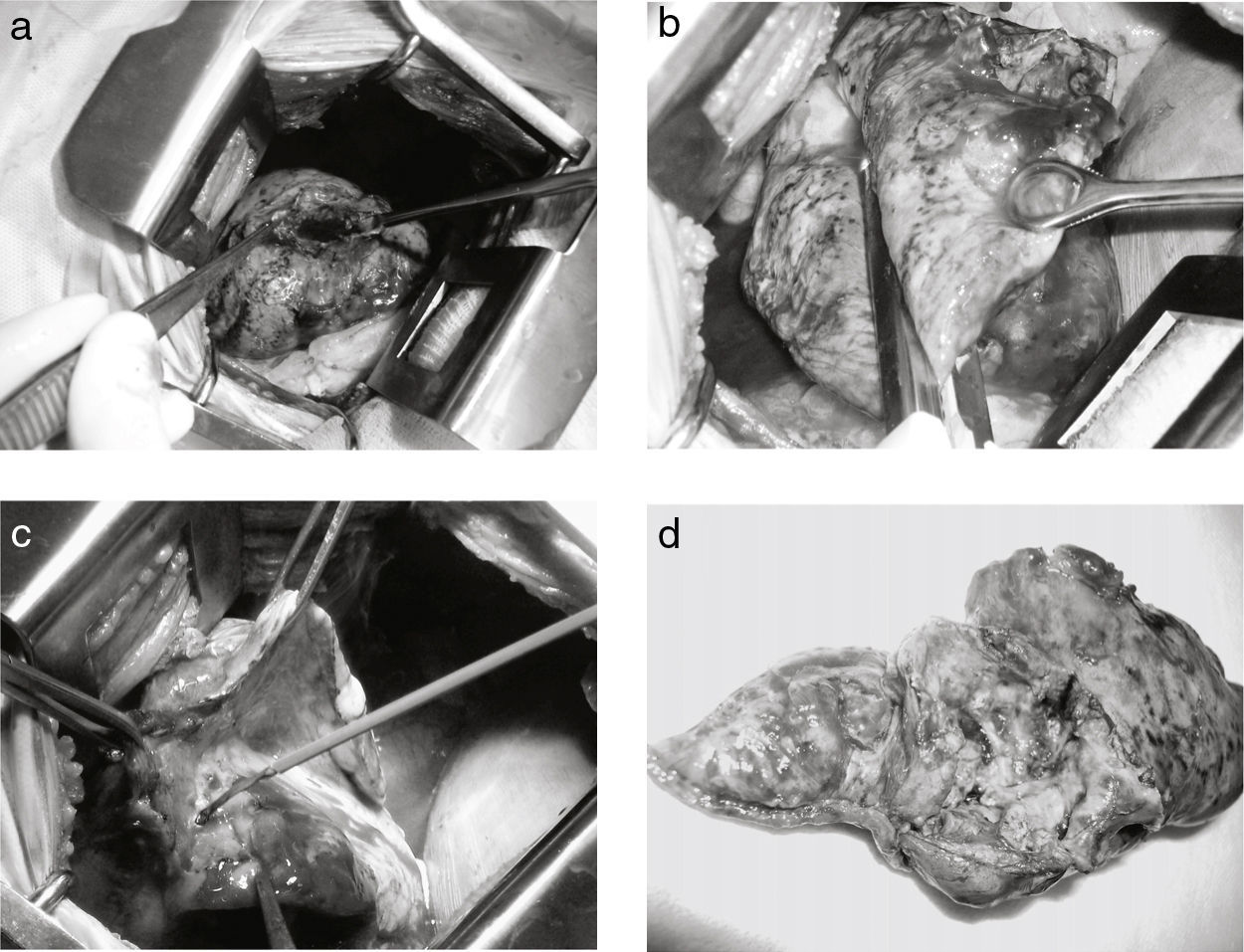
The fever persisted, and therefore treatment was rotated to colistin and imipenem for 14 days due to the isolation of Klebsiella pneumoniae and Pseudomonas aeruginosa in the bronchoalveolar lavage. The clinical course was favourable and the patient was discharged with 60mg/day of prednisone. At home, he started feeling a penetrative rib pain associated with dyspnoea, and went to the Emergency Department. In the chest X-ray, a right grade II pneumothorax was observed and pleural drainage was performed. A subcutaneous emphysema appeared and a persistent bronchopleural fistula with air-leak and purulent sputum. Axial computed tomography was requested, and showed pyopneumothorax and a lung mass abscess and cavity in the right upper lobe (Fig. 1b). Given the persistence of purulent sputum and lung expansion failure, surgical treatment was performed. The approach was a posterolateral thoracotomy and an abscessed and fistulised pleural granuloma was identified, of 11cm in diameter, located in the right upper lobe (Fig. 2a). A complete resection was performed with mechanical suture (Fig. 2b), completing the surgery with pulmonary decortication (Fig. 2c). Following the operation, he was immediately transferred to the intermediate care unit for 48h, and was discharged 6 days after surgery with a favourable postoperative course. The histopathology report of the surgical specimen (Fig. 2d) confirmed the diagnosis of Wegener's granulomatosis.
Pneumothorax or pyopneumothorax is an extremely rare manifestation of Wegener's granulomatosis (WG), with only 9 cases reported in literature worldwide.2 There was predominance in males, as in our case, and an average age of 48.9 years was observed. On admission, pneumothorax was present in 6 of the 9 patients, pyopneumothorax in 3, and associated empyema in 1.3,4
Lung nodules represent over 70% of lung lesions in patients with Wegener's granulomatosis.3 These are usually subpleural and can cavitate in nearly 50% of cases. Pleural involvement, however, is infrequent, being less than 10%. The lungs are the most common location of nodules in this disease and the contact between these nodules and the pleura is frequent,3 which coincides with our case.
On admission, our patient had small subpleural nodules and a partially cavitated solid lesion in the right lung; this is the most common radiographic image of Wegener's granulomatosis.3
Bronchopleural fistula and necrotic granulomatous lesions with expansion to the pleura have been previously reported.2 Lung expansion failure, which did not improve with continuous aspiration, has also been reported and is associated with infection and pyopneumothorax,1which was the case for our patient.
Pleural drainage was performed in 5 of the 9 cases and lobectomy in one. It was decided not to conduct surgery in 2 of the 9 cases (22.2%). In our case, the initial surgery was pleural drainage for pyopneumothorax. Its failure led us to perform a posterolateral thoracotomy on the patient and resect the lesion.
Postoperative mortality associated with patients admitted with pyopneumothorax was observed in 66.6% (2 out of 3 patients).3
Immunosuppressive therapy, particularly with cyclophosphamide, has undoubtedly improved survival rates.1
Please cite this article as: Ruiz CA, et al. Pioneumotórax por enfermedad de Wegener. Cir Esp. 2013;91:54–63.