Newborn hearing screening has as its main objective the early identification of hearing loss in newborns and infants. In order to guarantee good results, quality indicators for newborn hearing screening programs are used as benchmarks.
ObjectiveTo observe and describe the reality of national newborn hearing screening programs in Brazil, and to evaluate if they can be referred to as having quality indicators.
MethodsIntegrative literature review in databases such as MEDLINE, LILACS, SciELO, and Google.
Results22 articles were analyzed in relation to newborn hearing screening coverage, the place and period newborn hearing screening was performed, initial results, referral to diagnostic procedures, loss to follow-up, and occurrence of hearing loss.
ConclusionTransient otoacoustic emissions were the most often used screening methodology. Coverage varied widely, and only a few maternity wards achieved 95% of the cases screened. Referral to diagnostic procedures was under 4%, but lack of adherence can be considered a barrier to successful follow-up. The occurrence of hearing loss ranged from 0% to 1.09%. The involvement of government, physicians, and society is necessary, so that the goals of newborn hearing screening can be achieved.
a triagem auditiva neonatal (TAN) tem por finalidade a identificação, o mais precoce possível, da deficiência auditiva em neonatos e lactentes. Para garantir a eficácia e eficiência destes programas os índices de qualidade em relação à triagem, diagnóstico e intervenção servem como orientação e guia.
ObjetivoConhecer e descrever a realidade nacional dos serviços de TAN no Brasil, e avaliar se os mesmos podem ser considerados como detentores de indicação de qualidade.
MétodoRevisão integrativa da literatura em bases como Medline, Lilacs, Scielo e Google.
ResultadosNo total, 22 artigos foram analisados para esta revisão, referente à cobertura da triagem auditiva neonatal, o local e período onde a TAN foi realizada, resultados iniciais, encaminhamentos para diagnóstico, taxa de abandono do programa e ocorrência de perda auditiva.
ConclusãoEmissões otoacústicas transientes foi o método de triagem mais utilizado. A cobertura da TAN variou muito e poucas maternidades atingiram a marca dos 95%. O encaminhamento para diagnóstico ficou abaixo dos 4%, porém a não adesão ao programa pode ser considerada uma barreira para o sucesso. A ocorrência de perda auditiva variou entre 0%–1.09%. É necessário um maior envolvimento dos políticos, equipes hospitalares e da sociedade para atingir os objetivos da TAN.
Hearing loss impacts on the capacity to communicate, as well as on the social, emotional, and economic condition (lower education) of the individual; therefore, prevention is one of the strategies proposed to reduce this impact.
In this context, the newborn hearing screening (NHS) aims to identify, as early as possible, hearing loss in newborns and infants. It assesses auditory function through physiological and electrophysiological measures of hearing. The goal is the referral of infants at risk for developing hearing loss to audiological diagnosis, so that intervention can be initiated as early as possible. Therefore, this process should be part of the actions that comprise comprehensive hearing healthcare during childhood.1
In some countries, NHS is an important tool for early detection of hearing loss and, therefore, the effectiveness and efficiency of these programs should be analyzed and guaranteed.
Guidelines that outline recommendations and define quality measures as a method to evaluate the results of these programs have been created. They are the so-called quality indicators, which recommend that the scope of hearing screening should be considered universal, that it must assess at least 95% of newborns, and that NHS should be performed within the first month of life. They also recommend referral of a maximum of 4% of babies screened for diagnosis; diagnosis attendance of at least 90% of referred babies and follow-up at a maximum of three months later; diagnosis of permanent congenital hearing loss in 1%–3% of newborns; and use of hearing aid one month after attaining diagnosis, with rehabilitation starting at 6 months of life. The screening should preferably be performed in the maternity ward, before hospital discharge, and should be organized in two steps (test and retest).2,3
In Brazil, there are 267 hearing screening services in 30 cities and 13 Brazilian states,4 figures considered low for a country that currently occupies the fifth position in the world in terms of size and population; these services represent approximately 10% of neonates screened in the country.5 It seems that, unlike many developed countries, universal NHS remains a challenge for Brazil, as the socioeconomic situation and resource availability vary considerably from one region to another.
Studies indicate a prevalence of severe/profound congenital sensorineural hearing loss of 0.5–5/1000 newborns, which is higher in developing countries5,6 and thus, early diagnosis is of utmost importance for the appropriate communication development. Considering the few epidemiological studies that describe the NHS programs and the diagnosis of hearing loss in Brazil, it is necessary to perform a review of publications on the occurrence of hearing loss in infants in Brazil. The purpose of this review, therefore, was to analyze and describe the national reality of NHS services in Brazil, and assess whether they can be considered as having quality indication. The occurrence of hearing loss, diagnosed by the NHS, was investigated.
MethodsThe present review is characterized as an integrative review of studies describing the results of hearing screening programs in Brazil. An integrative review is a methodological approach that allows for the inclusion of several types of studies and enables conclusions in a particular area of study.7 To identify the studies, the following databases were used: MEDLINE, LILACS, SciELO, Google Scholar, and thesis databases of major universities.
The subject descriptors (DeCS) used were related to the intervention (neonatal screening, hearing screening, newborn) and the outcome (hearing, hearing loss, hearing disorder) in all possible combinations associated with the word “Brazil”. All periods until February of 2013 were included, with no restrictions regarding language of publication.
To ensure that the most studies would be identified, journals and abstracts of the congresses of the Brazilian Academy of Audiology, the Brazilian Society of Speech Therapy, and the Brazilian Association of Otolaryngology and Head and Neck Surgery between 2008 and 2012, and of the Brazilian Society of Pediatrics between 2006 and 2011 were manually researched. These dates were selected due to the availability of online abstracts. Subsequently, the titles and abstracts of articles were read by two reviewers, independently. Those that conformed to the inclusion and exclusion criteria were selected. After the selection, the reviewers met to agree upon the inclusion or exclusion of articles. A manual search for references was also performed.
The inclusion criteria used to describe NHS programs were: (a) population of neonates born in public or private maternity hospitals submitted to hearing screening with electrophysiological measurements (transient evoked otoacoustic emissions [TEOAE] and/or distortion-product otoacoustic emissions [DPOAE] or/and brainstem auditory evoked potential [BAEP]); (b) operation of hearing screening programs for at least five months to avoid inconsistent results that may occur during the initial operation of these programs.8 The NHS must have been carried out in the maternity hospital and before discharge; (c) description of the hearing screening process; rate of screenings performed in relation to the number of babies born in the maternity hospital, the number of babies who were unable to attain satisfactory results in the first evaluation, the number of neonates referred to retest, diagnosis and description of the number of those that did not complete the first phase of hearing screening, and percentage of hearing loss found.
Studies referring to a specific subpopulation and lower quality studies (inconsistent data or confusing discussion) were excluded.
Descriptive studies were evaluated, as the purpose of this review was to assess the quality of NHS services performed in hospitals in Brazil and the description of hearing loss prevalence as a result of NHS.
The presentation of the data is limited to descriptive information and a narrative summary, due to the heterogeneity of the articles. The description of the NHS and its results and the prevalence of hearing loss found in these studies were selected as outcomes.
ResultsBased on the search criteria, 195 citations were found, including articles, congress abstracts, masters degree dissertations, and doctoral theses. Of this total, 63 articles were duplicates and were excluded. Of the remaining 132 articles, the title and abstract were read, and 78 articles were read in full. A total of 22 met the inclusion criteria and were analyzed for this review.9–34
When searching for studies describing NHS programs in languages other than Portuguese, three articles and one summary in English,16,23,27,34 13 abstracts presented at congresses,10,16,17,19–22,24,27,30,31,33,34 and two dissertations11,26 were found.
Newborns that did not have a satisfactory performance in the initial hearing screening are referred for retesting within seven to 30 days. If there is no improvement in the electrophysiological responses, they are referred to audiological diagnosis, which evaluates them through brainstem auditory evoked potential (BAEP), audiometric tests with visual reinforcement, and assessment of middle ear status. Most services use a two-phase protocol: the first phase is the initial hearing screening and the second, the retest. Babies who do not have risk indicators for hearing loss and performed well in the initial screening are discharged. If the neonate has a risk indicator for hearing loss, even after a good performance in the hearing screening, the baby will be referred for hearing follow-up.
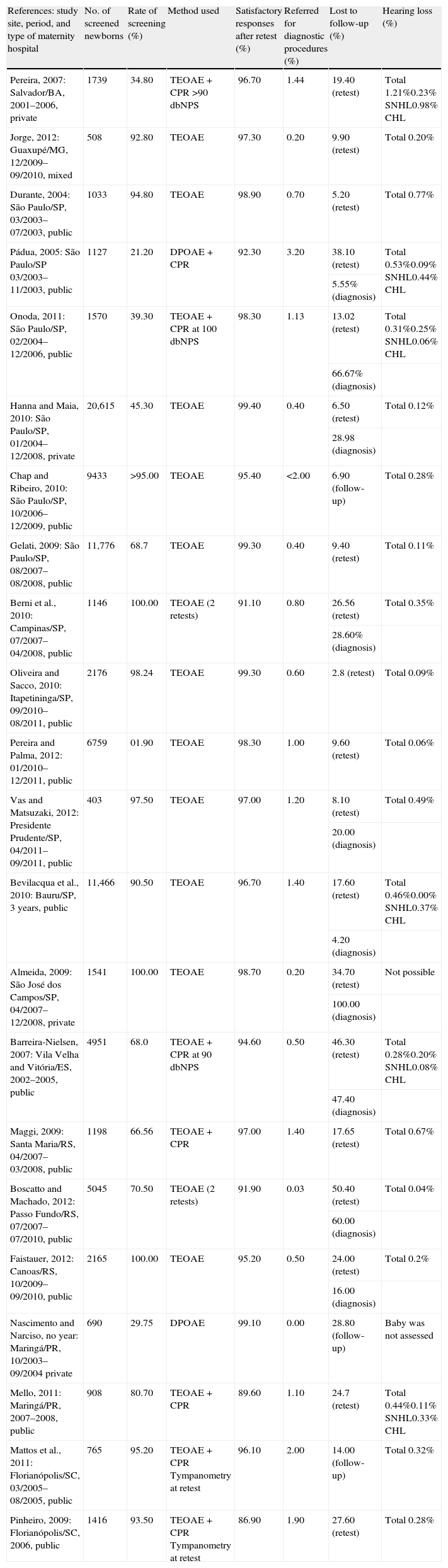
Table 1 shows a summarized description of all articles in relation to cities, maternity hospitals in which NHS was described, the period of study performance and results, NHS rates, the final outcome of the first phase, the number of newborns who did not attend retesting/diagnosis, and the percentage of babies referred for audiological diagnosis who demonstrated hearing loss.
Description of the NHS in relation to the type of maternity hospital, city/town, time period, percentage of babies screened in relation to number of live births in the same period, result of NHS after the first phase, percentage of infants referred for diagnostic procedures in relation to the total screened infants, percentage of babies that left the program at some stage, and percentage of hearing loss in relation to the total number of screened babies.
| References: study site, period, and type of maternity hospital | No. of screened newborns | Rate of screening (%) | Method used | Satisfactory responses after retest (%) | Referred for diagnostic procedures (%) | Lost to follow-up (%) | Hearing loss (%) |
| Pereira, 2007: Salvador/BA, 2001–2006, private | 1739 | 34.80 | TEOAE+CPR >90dbNPS | 96.70 | 1.44 | 19.40 (retest) | Total 1.21%0.23% SNHL0.98% CHL |
| Jorge, 2012: Guaxupé/MG, 12/2009–09/2010, mixed | 508 | 92.80 | TEOAE | 97.30 | 0.20 | 9.90 (retest) | Total 0.20% |
| Durante, 2004: São Paulo/SP, 03/2003–07/2003, public | 1033 | 94.80 | TEOAE | 98.90 | 0.70 | 5.20 (retest) | Total 0.77% |
| Pádua, 2005: São Paulo/SP 03/2003–11/2003, public | 1127 | 21.20 | DPOAE+CPR | 92.30 | 3.20 | 38.10 (retest) | Total 0.53%0.09% SNHL0.44% CHL |
| 5.55% (diagnosis) | |||||||
| Onoda, 2011: São Paulo/SP, 02/2004–12/2006, public | 1570 | 39.30 | TEOAE+CPR at 100 dbNPS | 98.30 | 1.13 | 13.02 (retest) | Total 0.31%0.25% SNHL0.06% CHL |
| 66.67% (diagnosis) | |||||||
| Hanna and Maia, 2010: São Paulo/SP, 01/2004–12/2008, private | 20,615 | 45.30 | TEOAE | 99.40 | 0.40 | 6.50 (retest) | Total 0.12% |
| 28.98 (diagnosis) | |||||||
| Chap and Ribeiro, 2010: São Paulo/SP, 10/2006–12/2009, public | 9433 | >95.00 | TEOAE | 95.40 | <2.00 | 6.90 (follow-up) | Total 0.28% |
| Gelati, 2009: São Paulo/SP, 08/2007–08/2008, public | 11,776 | 68.7 | TEOAE | 99.30 | 0.40 | 9.40 (retest) | Total 0.11% |
| Berni et al., 2010: Campinas/SP, 07/2007–04/2008, public | 1146 | 100.00 | TEOAE (2 retests) | 91.10 | 0.80 | 26.56 (retest) | Total 0.35% |
| 28.60% (diagnosis) | |||||||
| Oliveira and Sacco, 2010: Itapetininga/SP, 09/2010–08/2011, public | 2176 | 98.24 | TEOAE | 99.30 | 0.60 | 2.8 (retest) | Total 0.09% |
| Pereira and Palma, 2012: 01/2010–12/2011, public | 6759 | 01.90 | TEOAE | 98.30 | 1.00 | 9.60 (retest) | Total 0.06% |
| Vas and Matsuzaki, 2012: Presidente Prudente/SP, 04/2011–09/2011, public | 403 | 97.50 | TEOAE | 97.00 | 1.20 | 8.10 (retest) | Total 0.49% |
| 20.00 (diagnosis) | |||||||
| Bevilacqua et al., 2010: Bauru/SP, 3 years, public | 11,466 | 90.50 | TEOAE | 96.70 | 1.40 | 17.60 (retest) | Total 0.46%0.00% SNHL0.37% CHL |
| 4.20 (diagnosis) | |||||||
| Almeida, 2009: São José dos Campos/SP, 04/2007–12/2008, private | 1541 | 100.00 | TEOAE | 98.70 | 0.20 | 34.70 (retest) | Not possible |
| 100.00 (diagnosis) | |||||||
| Barreira-Nielsen, 2007: Vila Velha and Vitória/ES, 2002–2005, public | 4951 | 68.0 | TEOAE+CPR at 90 dbNPS | 94.60 | 0.50 | 46.30 (retest) | Total 0.28%0.20% SNHL0.08% CHL |
| 47.40 (diagnosis) | |||||||
| Maggi, 2009: Santa Maria/RS, 04/2007–03/2008, public | 1198 | 66.56 | TEOAE+CPR | 97.00 | 1.40 | 17.65 (retest) | Total 0.67% |
| Boscatto and Machado, 2012: Passo Fundo/RS, 07/2007–07/2010, public | 5045 | 70.50 | TEOAE (2 retests) | 91.90 | 0.03 | 50.40 (retest) | Total 0.04% |
| 60.00 (diagnosis) | |||||||
| Faistauer, 2012: Canoas/RS, 10/2009–09/2010, public | 2165 | 100.00 | TEOAE | 95.20 | 0.50 | 24.00 (retest) | Total 0.2% |
| 16.00 (diagnosis) | |||||||
| Nascimento and Narciso, no year: Maringá/PR, 10/2003–09/2004 private | 690 | 29.75 | DPOAE | 99.10 | 0.00 | 28.80 (follow-up) | Baby was not assessed |
| Mello, 2011: Maringá/PR, 2007–2008, public | 908 | 80.70 | TEOAE+CPR | 89.60 | 1.10 | 24.7 (retest) | Total 0.44%0.11% SNHL0.33% CHL |
| Mattos et al., 2011: Florianópolis/SC, 03/2005–08/2005, public | 765 | 95.20 | TEOAE+CPR Tympanometry at retest | 96.10 | 2.00 | 14.00 (follow-up) | Total 0.32% |
| Pinheiro, 2009: Florianópolis/SC, 2006, public | 1416 | 93.50 | TEOAE+CPR Tympanometry at retest | 86.90 | 1.90 | 27.60 (retest) | Total 0.28% |
SNHL, sensorineural hearing loss; CHL, conductive hearing loss; TEOAE, transient evoked otoacoustic emissions; DPOAE, distortion-product otoacoustic emissions; BAEP, brainstem auditory evoked potential; CPR, cochlea palpebral reflex.
All hearing health programs should be analyzed in relation to their cost–benefit ratio. Frequently, the difficulties faced for their implementation are not financial or technological. The lack of infrastructure and support services for family members, lack of quality control services and unified protocols, follow-up difficulties, and high costs may be responsible for frequent poor outcomes.9 An appropriate follow-up started at the moment of the hearing screening procedure, progressing through the audiological diagnosis, and thereby allowing an intervention to be implemented as early as possible is essential for an effective NHS program.35
The United States was the first country to perform NHS, subsequently followed by many other countries. The initial proposal intended to detect hearing loss in newborns at risk, but expanded to the early identification of hearing loss in all newborns.36 According to the standards established by JCIH and COMUSA,1,2 for an NHS program to be considered universal, it must reach, six months after its implantation, a minimum of 95% of infants assessed during postpartum admission, or before one month of life.
This integrative review included publications relating to NHS programs in Brazil that indicate the rates of screened newborns, results of NHS in the maternity hospitals, referrals for diagnosis, prevalence of hearing loss, and dropout rates at the follow-up.
The rate of screened newborns in this review varied significantly between studies, and only nine reached a 95% rate.16,18–20,22,24,29,32,34 Private hospitals showed lower rates, as NHS is not offered free-of-charge in most of them. Parents of newborns from the NICU represent a larger percentage who request the optional NHS service.9 The private maternity hospital that had greatest success in the screening rate was exclusive for treatment of insured pregnant women.24 The lack of 95% coverage observed in studies of public hospitals is caused by early discharge and a small number of audiologists employed to perform the hearing screening in these hospitals, making it impossible to assess hearing during at all times.16,17,21–24
The methodology used for the NHS was assessment through TEOAE,11,12,16–18,20–29,31–33 and DPOAE to a lesser extent.30 Reduced costs, better objectivity, and less invasiveness surely contributed to the preference for this method, compared to the use of BAEP, which evaluates the electrophysiological conduction of auditory stimuli to the peripheral portion of the brainstem.4 Some maternity hospitals have added the cochlea palpebral reflex (CPR), through the use of single or multiple bells in the NHS, but there is no consensus on the intensity to be used to elicit such reflex.9,10,13,14,25,26,31–33 The protocols differ broadly regarding the type and model of equipment used, as well as the follow-up criteria and protocols.
Most studies showed satisfactory NHS responses after the second phase of retesting, with more than 96% success rate. The lowest rate in the two studies31,33 can be attributed to unfavorable environmental conditions or to the inexperience of the NHS audiologist to properly perform the assessment.5 The percentage of infants referred for diagnosis remained below 4%, which is the recommended rate and an indicator of screening quality.
The rates describing the lack of feedback for retest varied between 5% and 50% in public hospitals and between 9% and 34% in the private and mixed hospitals. The lack of adherence for diagnosis showed high rates, between 5% and 66% in public hospitals and between 28% and 100% in the private and mixed hospitals; they are noteworthy, as the diagnostic follow-up showed lower adherence compared to retest, perhaps because it is be performed outside of the maternity hospital. The cities in the countryside of the Southeast clearly showed higher diagnosis adherence rates; one explanation would be that hospitals in smaller cities facilitate the organization of NHS programs. São Paulo was the pioneer city in the implementation of NHS, and the initial discussions for improving the structure of the NHS programs have been developed for a longer period of time.37
The World Health Organization has identified some key elements for the effectiveness of NHS programs. They include providing information to parents, physicians, audiologists, politicians, and educators about the importance of hearing and the consequences of a late diagnosis, the development of an NHS screening and follow-up system at all stages, and family centered support.5
The present review found a proportion of hearing loss that ranged from 0% to 1.09%. This result differs from rates found in other studies in developing countries, which reported percentages of hearing loss between 1% and 53%.36 The NHS was implemented in some hospitals and regions in Latin America, but there are no programs at a national level in the countries from this region.37
The lack of systematization in the collection and analysis of data makes it difficult to determine the actual prevalence of hearing loss in these newborns.37 Another explanation for the low rate of hearing loss in newborns found in this study is the lack of a significant number of mothers who return for retesting and/or diagnosis. The follow-up for the audiological diagnosis is essential for an NHS program to succeed. The percentage of those who return for retesting and/or audiological diagnosis after discharge is an index that demonstrates both the efficiency of the monitoring program in the newborn, in the subsequent hearing assessment phases, as well as the willingness of parents to complete the NHS program.
Income, low educational level, and low number of prenatal consultations are reported in the literature as obstacles to NHS completion.35,38,39 The lack of awareness by the mother can result in forgetfulness and lack of adherence to the follow-up.15,40 Studies have shown that adherence in all stages of NHS can be attained when the medical staff of the hospital, as well as nurses, social workers, and speech therapists are involved in the NHS.23,41–43 One of the suggestions found in the literature to reduce the dropout rate of the program is the aggregation of the NHS into other federal programs such as neonatal screening tests, or growth and development monitoring programs performed in outpatient clinics.23
Another suggestion is to advise mothers about the NHS and hearing loss in newborns individually, trying to maintain a favorable and peaceful environment for the emergence of doubts. The vocabulary between the professional and parents should be simple and clear, and the advice can be given by a social worker.41
The interpretation of hearing loss prevalence should be considered carefully, especially as there was no heterogeneity in the methodology used for hearing screening, and the dropout rate in the retest or diagnosis was demonstrated to be very high in some studies.10,13–15,18,24,25,27,28,30,33,34
While countries with well-established NHS services are currently concerned with diagnosis follow-up and rehabilitation, Brazil is still in its infancy for the implementation of NHS programs. It is essential to discuss and organize all phases in order to achieve the goal of early diagnosis.
ConclusionThis literature review showed that most NHS screening procedures occurs at public hospitals, and less than 50% were able to reach the rate of 95% of screened newborns. Protocols vary from service to service, hindering comparisons and the establishment of quality standards. Non-adherence to the audiological diagnosis compromises the quality of service and represents one of the major challenges. The occurrence of hearing loss was lower than that expected when compared to the literature. One factor responsible for this result may be the non-adherence to audiological follow-up. Specific adaptations to the cultural context are necessary to enable effective hearing screening programs.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Cavalcanti HG, de Melo LP, Buarque LF, Guerra RO. Overview of newborn hearing screening programs in Brazilian maternity hospitals. Braz J Otorhinolaryngol. 2014;80:346–53.