To describe a clinical report pre- and post-neurofunctional intervention in a case of agenesis of the corpus callosum.
Case descriptionPreterm infant with corpus callosum agenesis and hypoplasia of the cerebellum vermis and lateral ventricles, who, at the age of two years, started the proposed intervention. Functional performance tests were used such as the neurofunctional evaluation, the Gross Motor Function Measure and the Gross Motor Function Classification System. In the initial evaluation, absence of equilibrium reactions, postural transfers, deficits in manual and trunk control were observed. The intervention was conducted with a focus on function, prioritizing postural control and guidance of the family to continue care in the home environment. After the intervention, there was an improvement of body reactions, postural control and movement acquisition of hands and limbs. The intervention also showed improvement in functional performance.
CommentsPostural control and transfers of positions were benefited by the neurofunction intervention in this case of agenesis of the corpus callosum. The approach based on function with activities that involve muscle strengthening and balance reactions training, influenced the acquisition of a more selective motor behavior.
Descrever um relato clínico pré e pós-intervenção neurofuncional num caso de agenesia de corpo caloso.
Descrição do casoApós o nascimento prematuro foi detectada agenesia do corpo caloso e hipoplasia dos ventrículos laterais e vérmis cerebelar. Aos dois anos iniciou a intervenção proposta neste estudo. Uma avaliação neurofuncional, além da Medida da Função Motora Grossa e o Sistema de Classificação da Função Motora Grossa, foi utilizada para obter o desempenho funcional da criança. Na avaliação inicial havia ausência de reações de equilíbrio e de transferências posturais, e déficits no controle manual e de tronco. A intervenção foi realizada com enfoque na função, priorizando o controle postural e a orientação da familia para continuidade do tratamento em ambiente domiciliar. Após a intervenção houve melhora das reações corporais, controle postural e aquisição de movimentos de mãos e membros. A intervenção também mostrou melhora no desempenho funcional.
ComentáriosO controle postural e as transferências de posições foram beneficiadas por intervenção neurofuncional nesse paciente com agenesia de corpo caloso. O enfoque baseado na função com atividades que envolvem fortalecimento muscular e treinamento das reações de equilíbrio influenciaram a aquisição do comportamento motor mais seletivo.
The central nervous system (CNS) is responsible for the interpretation and transmission of sensory, cognitive, and motor information. In its central region lies the corpus callosum (CC), which transmits the information between the cerebral hemispheres1 through a single, exclusive tract used for integration.2
Alterations characterized by partial genesis (dysgenesis) or complete absence (agenesis) of the CC can generate an inter-hemispheric disconnection.3,4 The incidence of agenesis and dysgenesis of the corpus callosum (ADCC) is estimated at one per 1,000 live births,5 with a prevalence of 2.3% in North America and unknown in Latin countries.4
Congenital malformations of the CNS, in general, may be associated with other malformations (brain or other segments) in 21% of cases.6 In ADCC, for instance, extra- and intracranial abnormalities7 may occur concomitantly, such as hydrocephalus,8 seizures,9 syndromes,10 and CNS malformations,11 among others.
The associated diseases may potentiate or add other clinical characteristics to ADCC cases. Thus, cognitive, social, visual, auditory, motor, and somatosensory deficits12 are typically observed in affected individuals. Some children with CC dysgenesis may have a typical development, but with some deficiency in psychosocial behavior.13 However, it is observed that children with ADCC often have delayed motor development, which can be demonstrated by maladjustment in performing skills, bilateral coordination, and manual control deficits.11,14
The motor intervention aims to reduce alterations resulting from the neurological disorder, capitalizing on the plasticity of the CNS through specific interventions.15 In addition to seeking techniques that promote rehabilitation, there is a concern regarding the forms of intervention, which should aim at functional capacity.16 Considering that rehabilitation plays a pivotal role in promoting functionality and the stimulation of motor development, this study aimed to describe a case before and after a neurofunctional intervention in a child with agenesis of the corpus callosum (ACC).
Case reportThis study was performed at Clínica Escola de Fisioterapia do Centro de Ciências da Saúde e do Esporte (CEFID) of the Universidade do Estado de Santa Catarina (UDESC), and was approved by the Ethics Committee for Research in Human Subjects according to Edict 263/2009, after the child's guardian signed the informed consent.
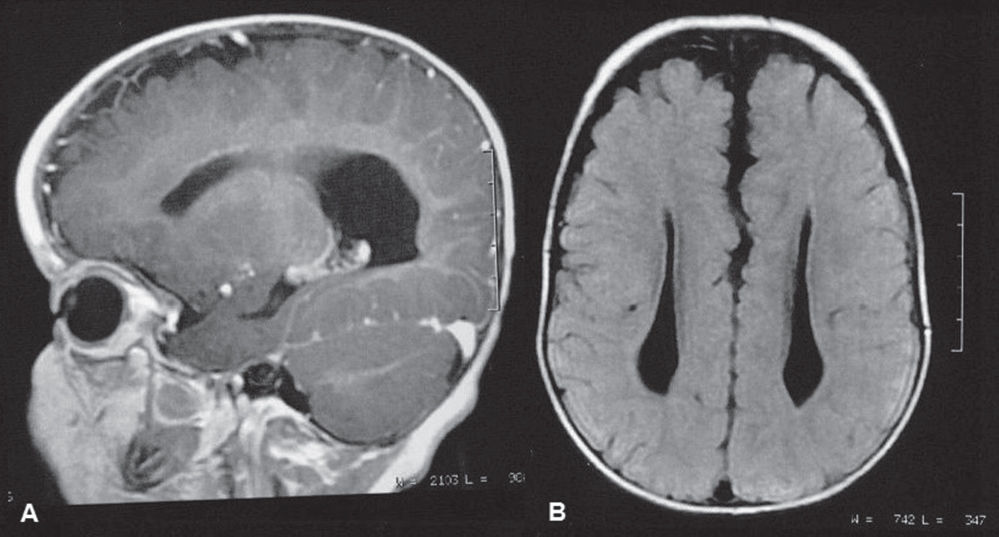
During prenatal care, the ultrasonography findings evidenced that the child had hydrocephalus. In the sixth month of pregnancy, the mother received a diagnosis of preeclampsia, which resulted in an emergency C-section delivery. The male child was born at 35 weeks and 4 days of gestational age, with Apgar score at 1 and 5 minutes of 7 and 8, respectively; weight of 2,020 g; length of 48 cm; head circumference of 34 cm; and small for gestational age. During the 17 days in the neonatal intensive care unit (NICU), agenesis of the corpus callosum (ACC) was detected, as well as hypoplasia of the lateral ventricles and cerebellar vermis (Fig. 1).
After NICU discharge, the infant was referred to early intervention at 3 months of corrected age at the Associação de Pais e Amigos dos Excepcionais in Florianópolis. During the first two years of life, he underwent surgical procedures for inguinal hernia removal, polydactyly repair, left testicle atrophy, and adenoids. At 2 years of age, he started presenting seizures, currently treated with anticonvulsants. The genetic study, although inconclusive, might be compatible with acrocallosal syndrome, according to the medical report.
At 2 years and 6 months of chronological age, he was admitted for treatment at the school clinic of CEFID/UDESC. To perform the patient's assessment, a child neurofunctional record was used, which consisted of: 1) identification (personal data); 2) personal history (past and current medical history, family history, associated diseases, and lifestyle); 3) motor behavior (reflexes and reactions, motor pattern involving the description of symmetries, transfers, movement, and postural adjustments in all positions); and 4) physical examination (muscle tone, deformities, postural deviations, and sensitivity). The Gross Motor Function Measure (GMFM-88)17 and the Gross Motor Function Classification System – Expanded & Revised (GMFCS-E&R),18 published in its Brazilian version19 – were applied to assess pre- and post-intervention functional performance.
At the initial assessment, the child had normal muscle tone in the upper limbs (UL) and fluctuating tone in the lower limbs (LL). Despite having no joint deformity, the patient showed a tendency to equinovalgus foot. Moreover, the following reflexes were absent: Landau, parachute, labyrinthine, neck and body straightening, and UL backward protective reaction. Balance on all fours, standing, and in the sitting position was also absent.
Regarding the motor patterns, the following was observed: a) the UL remained under the body when transferring from supine to prone positions; b) there was lack of support from the UL in the prone position, with incomplete cervical extension, poor range to grab objects, and lower limb extensor pattern; c) the patient was not able to transfer from the supine to the sitting position; d) the patient did not remain seated with trunk control and hands free for long or at backward movements; e) the patient did not perform transfers from the sitting position; f) the patient demonstrated weight-bearing in the standing position, and simulated steps with support from the pelvic girdle; g) the patient showed self-locomotion for short distances using the rolling movement, and, when prone, tried to crawl without alternating movement of the lower limbs; and h) absence of bimanual control with large objects, unimanual control deficit, and incoordination to reach objects.
At the initial GMFM, the points obtained were primarily in lower positions (prone, supine, and sitting); however, even in these positions, he did not achieve the maximum score, as he did not attain postural transfers, balance, and selective control of the limbs. According to the GMFCS-E&R, the child was classified as level IV (self-mobility with limitations) for the corresponding age group (between 2 and 4 years).
Based on this assessment, the goals of the neurofunctional intervention were: to improve UL support in the prone position; to achieve uni- and bimanual coordination and handling of objects; to promote the extension of the lower limbs in the sitting position; to acquire new postures (on all fours, kneeling, semi-kneeling, and standing positions); and to promote the active transfer between them. Other goals were developing balance, protective, and weight-bearing reactions in all positions, as well as strengthening of the limbs and abdominal muscles. During the intervention, the authors sought to prevent range of motion alterations and deformities.
The neurofunctional intervention was based on the use of kinesiotherapy, as well as sensory and proprioceptive resources, in 40-minute sessions twice a week.
The kinesiotherapy consisted of muscle strengthening, stretching, and mobilization of upper and lower limbs, training postural maintenance and change, weight bearing, and stimuli for balance, correction, and protection reactions. The mother actively participated in the intervention, giving feedback to the therapist by describing the child's activities, continuing the treatment at home, performing the exercises taught by the therapist, and offering her child greater freedom of movement. The intervention was conducted using a wooden platform, mats, benches, toys, wedges, support rolls, and Swiss balls.
The reassessment used the same initial tools and was conducted after 15 interventions, when the child was 2 years and 10 months of age. It was observed that the tendency to equinovalgus deformity of the foot persisted, but the stretching, positioning, and instructions given to the caregiver prevented the deformity. The balance reactions were favored by the intervention, so that they were acquired on all fours, as well as in the standing and sitting positions. The protective, labyrinth, and neck and body correction reactions were acquired.
In relation to motor behavior, movement acquisition was achieved and postural permanence time improved. The following were achieved: a) in the prone position: full support of upper limbs on hands, and ability to reach out; b) sitting: improved backward balance, allowing the patient to sit on a bench and on his side, handling objects; c) on all fours: the patient remained with extended elbows and crawled with the lower limbs; d) kneeling: actively sustained trunk with pelvic girdle support or support of a low stool; e) semi-kneeling: actively remained in the position for a short time; f) in the standing position: gait was started with support from the therapist's hands or pelvic girdle. After training, postural transfers from supine to sitting, from sitting to kneeling (actively assisted), from kneeling to semi-kneeling (actively assisted), and from kneeling to standing with support of a low stool were achieved (Fig. 2).
Post-intervention results: (A) While sitting on the low stool, the patient maintained trunk control performing uni- or bimanual object handling; (B) Patient can transfer from the sitting to the kneeling position using a low stool support; (C) Patient remains on all fours and performs decoupling of limbs; (D) In the standing position, patient walks with the therapist's support
The child began to handle small and large objects with better coordination and handgrip, which helped improve his daily activities and playing, according to the mother. This improvement in movement control was demonstrated by the GMFM, as positions requiring control or weight bearing on hands and UL were achieved.
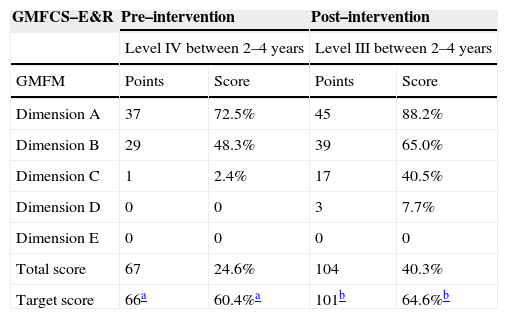
The results obtained when applying the scales at the final assessment were positive, as shown in Table 1. Due to low or zero values acquired in dimensions C, D, and E, the authors chose to present the target score of dimensions A and B at the initial assessment. After the intervention, dimension C was added to this score. At the GMFCS-E&R, the patient progressed from level IV to III. At this level, he could crawl on his hands and knees, pull himself up to stand, and walk with assistance from others. Although he performed activities related to level II, such as crawling alternately, this level could not yet be considered, because the child needed assistance when transferring to the sitting position and still required gait aids for locomotion.
Pre– and post–intervention function
| GMFCS–E&R | Pre–intervention | Post–intervention | ||
|---|---|---|---|---|
| Level IV between 2–4 years | Level III between 2–4 years | |||
| GMFM | Points | Score | Points | Score |
| Dimension A | 37 | 72.5% | 45 | 88.2% |
| Dimension B | 29 | 48.3% | 39 | 65.0% |
| Dimension C | 1 | 2.4% | 17 | 40.5% |
| Dimension D | 0 | 0 | 3 | 7.7% |
| Dimension E | 0 | 0 | 0 | 0 |
| Total score | 67 | 24.6% | 104 | 40.3% |
| Target score | 66a | 60.4%a | 101b | 64.6%b |
The rehabilitation goal in patients with ACC is to improve the individual's overall function through a multidisciplinary team and trained caregivers.15 The patient in this study had inguinal hernia, as well as left testicle and adenoids atrophy, which are not part of ADCC. He also had polydactyly, seizures, and hydrocephalus, which may be associated with CC malformation.
These alterations, whether associated or not, emphasize the need for a multidisciplinary intervention. The present patient demonstrated delayed motor development, which is common in this population.14 However, children with ACC may also have a typical development, within the normal range of intelligence.13 Early intervention allows for a more effective prevention of the factors that can cause or enhance development alterations. Thus, it is important to start treatment as early as possible in order to prevent secondary physical or mental complications, thus capitalizing on the plasticity of the CNS as much as possible.15
In the present case, the child showed no orthopedic deformities or limitations in range of motion. However, muscle weakness and altered muscle tone determined the need for preventive intervention, which, in the long term, could result in the onset of deformities. Deformities and functional limitations impair the performance of motor skills and should be prevented.
Studies11,20 have demonstrated that individuals with ACC have significant deficits in handgrip, manual dexterity, and coordination. It is essential that early intervention considers such aspects, aiming at the stimulation of functionality. In this case report, the child showed great improvement in manual and bimanual motor skill acquisition in handling objects.
Joint stability, stretching, and muscle strength should be associated with central control, involving functional activities of movement, acquisition, and maintenance of different postures.21 The therapeutic approach based on prevention of functional limitations; muscle strengthening; and training of correction, protection, and balance reactions influenced the development of functional capacity throughout the analyzed period.
The motor intervention focused on functionality was shown to be effective, because both the GMFCS-E&R and the GMFM evidenced an improvement in gross motor function after a short intervention period. However, the intensive participation of the child's mother was crucial for the intervention's success. It is imperative to emphasize the importance of family involvement in promoting child development in the home environment.
Parents of children with ACC can help in improving deficit characteristics that affect the daily lives of their children.22 Evidence suggests that, in children with congenital or acquired disorders, a family-centered therapy focused on early identification of functional compensation, adapting the environment and tasks through feedback and advising those responsible for the child, will help improve the quality of the child's performance.23
ACC has been rarely addressed in scientific studies, and one reason for this fact may be the small number of cases worldwide. Furthermore, of the existing cases, no study had proposed a neurofunctional intervention regarding postural control in patients with ACC. Therefore, this report can be used as basis for future studies involving motor intervention in children with ACC, in order to develop the topic and support these results.
Conflicts of interestThe authors declare no conflicts of interest.
To Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes), for the grant received.