Osseous dysplasias are idiopathic processes located in the periapical region of the maxillary-mandibular complex. They are characterized by the substitution of normal osseous tissue for fibrous tissue and metaplastic osseous tissue. Florid osseous dysplasia (FOD) describes a set of radio-lucid and radio opaque inter-radicular and periapical lesions, bilaterally found in the mandible and sometimes in the upper jaw. The present project presented a FOD case diagnosed by means of histological, radiological and clinical findings; there was presence of infection and painful symptoms. A 62 year old female patient treated at the Oral-Maxillofacial Surgery Unit of the General Hospital «Dr. Domingo Luciani», Caracas, Venezuela sought medical care. The patient reported onset of the condition two weeks before consultation, she experienced intense pain in the right mandibular posterior region with presence of intra-oral fistula and purulent discharge. X-ray examination revealed multiple radio-opaque lesions involving all four quadrants. Excision biopsy was undertaken, histopathological study indicated presence of florid osseous dysplasia. The patient was assessed during an 11 month asymptomatic post-operative period.
Las displasias óseas son procesos idiopáticos ubicados en la región periapical del complejo maxilar mandibular caracterizados por un reemplazo de hueso normal por tejido fibroso y hueso metaplásico. La displasia ósea florida (DOF) se refiere a un conjunto de lesiones periapicales e interradiculares radiolúcidas y radiopacas ubicadas en la región mandibular bilateral y ocasionalmente en el maxilar. El presente trabajo tiene como objetivo presentar un caso de DOF diagnosticada mediante hallazgos clínicos, radiográficos e histológicos, con presencia de sintomatología dolorosa e infección. Se presenta femenina de 62 años tratada en la Unidad de Cirugía Buco-Maxilofacial del Hospital General del Este, «Dr. Domingo Luciani», Caracas, Venezuela, quien refiere inicio de enfermedad actual dos semanas previas a la consulta presentando dolor intenso en región posterior mandibular derecha con presencia de fístula intraoral y secreción purulenta. Al examen radiográfico se observó múltiples lesiones radiopacas que involucraban los cuatro cuadrantes. Se realizó biopsia excisional y el estudio histopatológico concluyó dis-plasia ósea florida. La paciente fue evaluada durante un periodo postoperatorio de 11 meses asintomático.
Osseous dysplasias are idiopathic processes located at the periapical region of the upper and lower jaw. They are characterized by a substitution of normal bone for fibrous tissue and metaplastic bone.1 In 2005, the World Health Organization (WHO) subdivided osseous dysplasia into periapical bone dysplasia, when the lesion is observed in the mandibular anterior sector, focal dysplasia when similar lesions occur and are limited to a mandibular posterior quadrant, florid dysplasia, when it occurs bilaterally in the mandible, and can even when it occurs bilaterally in the mandible, and can even show participation of all four quadrants, and familial giant cementoma when it occurs at early ages, causing considerable lower jaw expansion. Clinical assessment cannot provide definite diagnosis of these entities, histopathological studies are required to reach this goal.1
Florid bone dysplasia (FBD) encompasses a set of radio-opaque and radio-lucid inter-radicular and periapical lesions bilaterally located in the mandibular region and occasionally in the maxillary region.2–4
FOD is classified by WHO as part of the fibrous osseous lesions.1 Melrose3 first described it with that name in 1976. At a later point, Waldron5 introduced the term florid osseous cement dysplasia due to the cement-like appearance exhibited by the dense sclerotic masses which are typical of that entity.
Presently the condition is known as florid osseous dysplasia, since this type of lesions are not considered cement-producing lesions.1
Presently the condition is known as florid osseous dysplasia, since this type of lesions are not considered cement-producing lesions.1
FOD exhibits multi-focal development in mandibular quadrants, sometimes in the upper jaw as well. It presents predilection for subjects of female gender, African ethnicity and in the fourth and fifth decade of life6. Lesions show a trend of symmetrical development and are generally accidentally detected when studying control X-rays.1,4,7
These lesions are generally asymptomatic, nevertheless, about 10% of them cause pain; exposition to the oral environment due to secondary infection, can additionally present intra oral or extra oral fistulae, with no evidence of bone expansion.8
Radiographically, radio-lucid, radio-opaque or mixed lesions can be observed. These lesions are bilaterally located in the mandible and are occasionally found in the maxilla. In certain cases, radio-opaque images thus generated can be confused with the normal aspect of the bone.9
Histologically, cellular fibrous tissue can be observed as well as lamellar bone, masses of cement- like material, absence of capsula, and calcified tissue is arranged in trabeculae and irregular masses.5–10 In cases when the lesion is infected there is presence of inflammatory infiltrate and fibrosis.
Treatment depends on symptoms. When the lesion is asymptomatic, periodic X-ray controls should be undertaken along with prophylaxis and oral hygiene reinforcement.11 In cases of painful symptoms, paresthesia or other relevant clinical changes, local treatment of the wound should be undertaken with use of analgesics, antibiotics and hyperbaric chamber. Alveolar resection or enucleation would be recommended in cases when the lesion does not show improvement.12
This project presents a case of florid osseous dysplasia diagnosed with the help of clinical, radiographic and histological findings. In this case, presence of pain and infection led to a comprehensive study of the patient.
CASE REPORTA 62 year old female patient sought clinical care at the Oral-Maxillofacial Surgery Unit of the «Dr Domingo Luciani» General Hospital of the West. A housewife, born in San Fernando del Guapo, State of Miranda and residing in Caracas, the patient attended the clinic after experiencing for two weeks intense pain in the right posterior region of the lower jaw, with presence of an intra-oral fistula and purulent exudate.
The patient informed she had previously attended another care -giving center, where a treatment of amoxicillin with clavulanic acid (500/125mg every 8hours for seven days) was prescribed. No medical improvement was experienced. Medical history of the patient was non-contributory. At the time she was being assessed, the patient reported presence of painful symptoms.
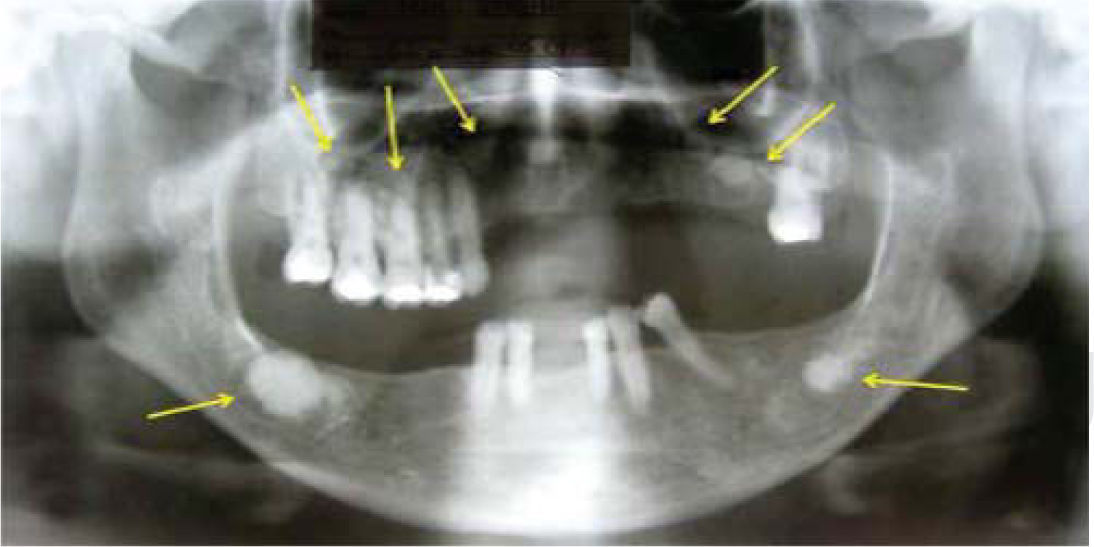
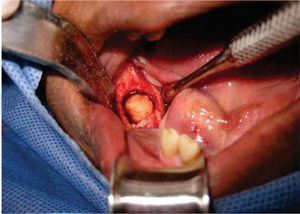
General physical exploration was non-contributory for the present condition. The patient informed of pain on palpation of the maxillofacial region, at the lower third of the right side of the face (Figure 1). Intra-oral examination revealed a partial bi-maxillary edentulous patient. Multiple restorations were observed in the maxillary posterior region, as well as presence of local irritation with a hyperemic lesion of approximately 5mm diameter in the right lower posterior alveolar ridge, with presence of purulent exudate upon palpation (Figure 2).
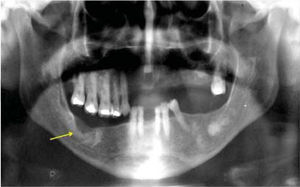
Dental sinus orthopantomographic X-ray study revealed multiple circumscribed (Figure 3), circular, radio-opaque images, involving all four quadrants. In the right mandibular body, a radio-opaque image of approximately 1.5mm surrounded by a radio-lucid image was observed which extended into the whole the basal portion of the lesion. This finding was compatible with an infectious process. Once clinical and radiographic data were gathered, the following possible differential diagnoses were proposed: florid osseous dysplasia, osteoma, sclerosing osteomyelitis and Paget's disease. Since the infectious process located under the lesion did not resolve with use of antibiotics, it was decided to conduct excisional biopsy of the lesion.
Sinus dental orthopantomography showing multiple circumscribed circular radio-opaque images involving all four quadrants (arrows). At the right mandibular body a radio-opaque image can be observed surrounded by a radio-lucid area which extends into all the basal portion of the lesion, compatible with an infectious process.
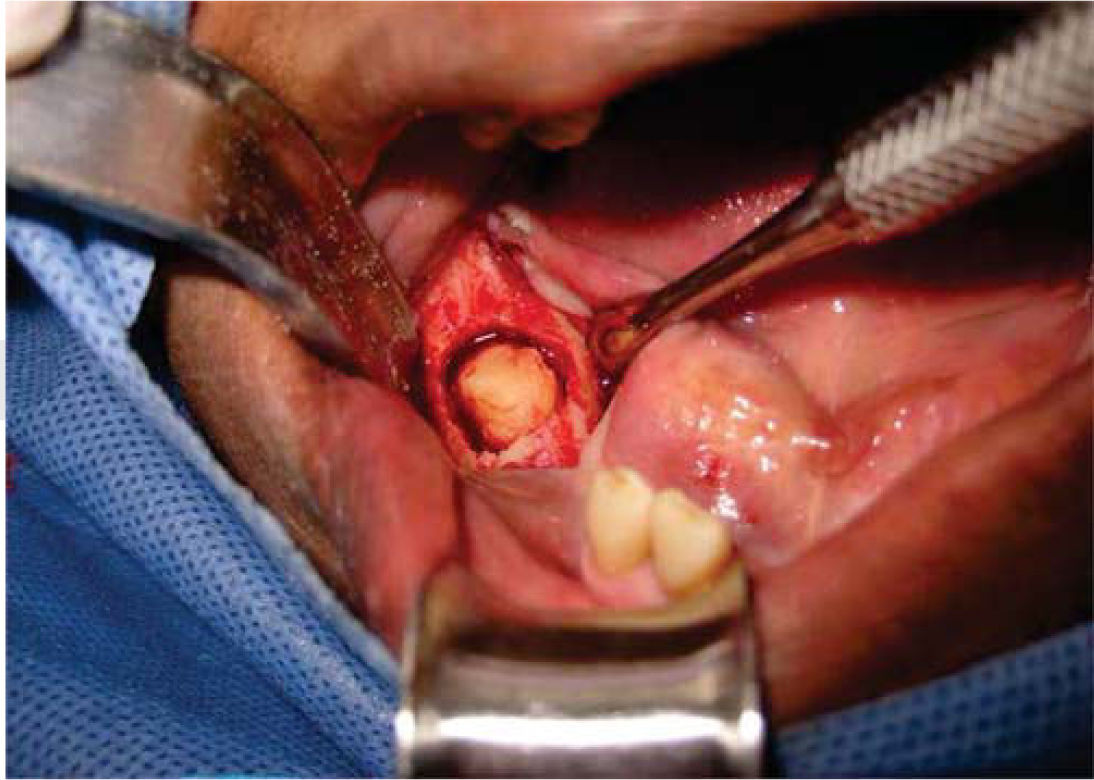
The lesion's excisional biopsy was executed under infiltrative local anesthesia with 2% lidocaine and 1:100.000 epinephrine (Figure 4). Surgical cleansing of the bed was conducted; from it an approximately 1.5cm sample of hard tissue similar to osseous tissue was harvested (Figure 5). Tissue synthesis was completed with 4-0 Nylon suture. Treatment with azithromycin (500mg every 24hours for three days) was prescribed.
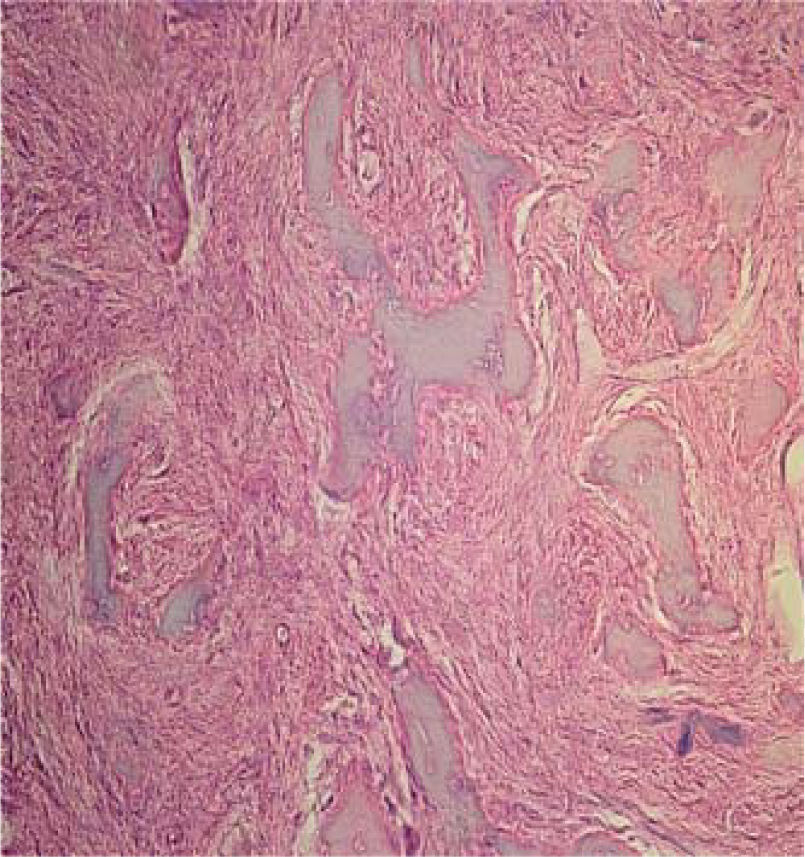
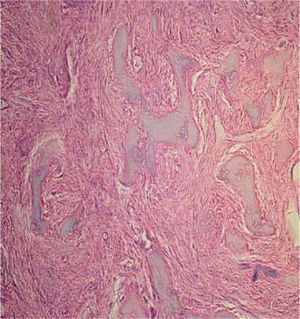
Histopathological study revealed a lesion formed by irregular bone tissue interspersed with fibroblasts and numerous endothelium-outlined blood vessels of normal appearance. The lesion was filled with erythrocytes with areas of dense lymphoplasmocytic inflammatory infiltrate (Figure 6).
Histopathological study with hematoxylin and eosin of the lesion composed of irregular bone tissue interspersed with fibroblasts and numerous blood vessels circumscribed with endothelium of normal aspect and replete with erythrocytes with areas of dense lymphoplasmocytic inflammatory infiltrate.
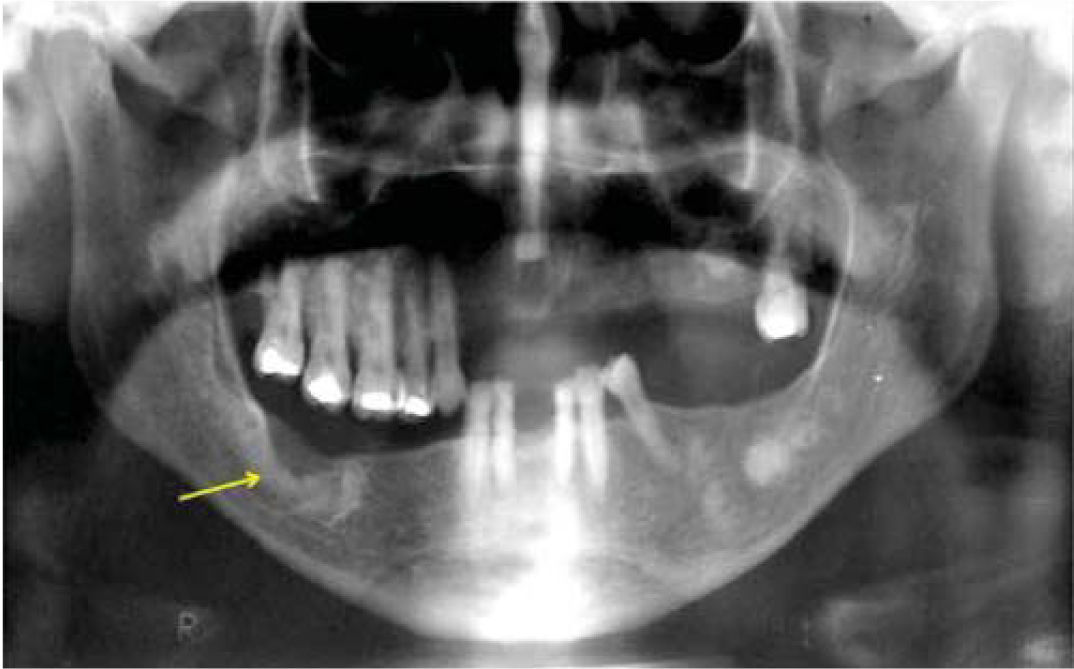
At an 11 month postoperative control, the patient exhibited lack of volume increase or mucosa coloring changes (Figure 7). Radiographic control revealed the operated area with suitable bone regeneration and the rest of lesions without any change in size (Figure 8). At that clinical examination, the patient denied presence of any pain.
With the passing years, diagnosis of FOD has been a subject of controversy. According to WHO, this diagnosis must be established through completion of histopathological studies.1 FOD is considered a lesion with particular clinical and radiographic characteristics which in most cases facilitate a clinical diagnosis. Several authors, such as Gündüz K et al13 reported that in several cases, in addition to radiographic evaluation, diagnosis is established by means of clinical assessment as well as evaluation of gender, age and ethnicity. This type of asymptomatic lesions are generally fortuitously detected through X-ray studies, therefore, taking biopsies is not considered pertinent.13
FOD exhibits ethnic, gender and age characteristics. It is most frequently observed in middle age women of African ethnicity. Venezuelan population is heterogeneous, considered by many as the American country with greatest ethnic blending. The case here presented was typical of epidemiological and clinical characteristics described for this type of lesion in scientific literature.
After accidental X-ray findings, patients are generally asymptomatic. Painful lesions are observed when they are related to infectious processes or associated to other lesions.4–14 There were similar findings in the present case, where the patient experienced painful symptoms related to local infectious processes.
From the radiographic perspective, diffuse, radio-opaque masses are observed in alveolar regions of multiple quadrants; this characteristic plays an important role in diagnosis establishment. Lesions are normally close to the teeth. In order to establish differential diagnosis, radiologic aspect, although not pathognomonic, is very characteristic and useful.13 Generally, no expansion of cortical bone is observed unless it were to be associated to cystic lesions.14 In the present case, lesions in the upper and lower jaw were found; they were related to areas of previous extractions and occlusal trauma, it could be therefore inferred that aggression can stimulate bone lesions.
After completing a comprehensive evaluation, possible differential diagnoses can be established. Among these we can count diffuse sclerosing osteomyelitis which appears as a generally unilateral, ill defined, radio-opaque mass in the mandibular region, while FOD appears as multiple radio-opaque areas involving both mandibular quadrants and in some cases maxillary quadrants as well.1–10 Paget's disease is characterized by presenting deformities in multiple bones and elicits biochemical changes in serum, such as high levels of alkaline phosphatase; this did not match our present case.
Treatment of histopathologically confirmed FOD depends on symptoms and other associations which might be exhibited by the lesion. In the case of asymptomatic lesions, routine clinical and radiographic control is recommended as well as prophylaxis in order to preserve suitable oral hygiene.11–13
We equally recommend patient's comprehensive care in order to preserve occlusal stability. In those cases when lesions are associated to local infections, enucleation is recommended as well as surgical cleansing of the area, since generally, these processes do not respond to antibiotic therapy.13
In our case there was infection under the lesion, which had been unsuccessfully treated with antibiotics, this prompted the decision to perform excision biopsy of the lesion and surgical cleansing of the area, these procedures resulted in disappearance of symptoms.
Fibrous-osseous lesions are considered common entities within the maxillofacial region. FOD is one of the most frequent lesions, for this reason, in order to achieve accurate diagnosis, we deem important to be acquainted with its clinical, radiographic and epidemiologic characteristics as well as its behavior.
As a conclusion it might be said that is of the utmost importance to possess necessary knowledge to diagnose and treat lesions in the maxillofacial region, especially when we face conditions which appear very similar to osseous dysplasia. These lesions are known to present very particular clinical and radiographic characteristics. Treatment plans will be varied and specifically dependent upon accurate diagnosis.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam