To compare displacement resistance of four cementing agents.
Material and methodsAn experimental, cross-sectioned prospective research was conducted to assess four cementing agents. Three agents were resinous, self-adhesive, dual polymerization cements containing MDP (10-metacryloxydecyl dihydrogen phosphate), and the remaining was a conventional glass ionomer cement. In the experiment, 40 samples of zirconia partially stabilized with yttrium were prepared. All samples were treated following their specific manufacturer's instructions. Samples were prepared, they were then stored at 100% humidity in a temperature chamber at 37 oC for 24 hours; after this, samples were subjected to shearing detachment mechanical tests at a 1 mm per minute speed in a universal machine for mechanical testing.
ResultsGlass ionomer samples failed before being taken to the universal testing machine. Remaining three cements did not show statistically significant differences.
ConclusionsAdhesion capacity of glass ionomer to zirconia is nil or extremely low. Likewise, resinous cements containing MDP in their formula, either in their bonding agent or in the cement formulation itself, are presently the best alternative to increase adhesion to a zirconia structure.
Comparar la resistencia al desplazamiento de cuatro agentes cementantes.
Material y métodosSe realizó una investigación prospectiva, transversal y experimental en la que se evaluaron cuatro agentes cementantes, tres de ellos resinosos autoadhesivos de polimerización dual y con contenido de MDP (10-metacriloxidecil dihidrógeno fosfato) y un ionómero de vidrio convencional. Se realizaron 40 muestras de zirconia parcialmente estabilizada con itrio, se dividieron en cuatro grupos, cada uno de ellos fue tratado de acuerdo con las indicaciones del fabricante del cemento a estudiar, se realizaron las muestras, se almacenaron en humedad al 100% en una cámara a una temperatura de 37 oC durante 24 horas para después ser sometidas a pruebas mecánicas de desprendimiento por cizallamiento a una velocidad de 1 mm por minuto en la máquina universal de pruebas mecánicas.
ResultadosLa muestras de ionómero de vidrio fracasaron antes de ser llevadas a la maquina universal, entre los otros tres cementos no existe diferencia estadísticamente significativa.
ConclusionesLa capacidad de adhesión de ionómero de vidrio a la zirconia es nula o muy baja. Igualmente los cementos resinosos que contengan en su fórmula MDP, ya sea en su agente de acoplamiento o en la fórmula misma de los cementos, son en la actualidad la mejor alternativa para incrementar la adhesión a una superficie de zirconia.
Zirconium oxide partially stabilized with yttrium (Y-TZP) better known as zirconia, has constituted a great success in the field of biomaterial research. Since the decade of the ‘70s, use of zirconia in dentistry was evidenced through studies proposing its use as a coating for implants.1 Nevertheless, it was only in the ‘90s when there were first reports of its use in implants.2 In 1991, there were reports of zirconia use in orthodontic brackets.3 Use of zirconia in the field of restorative dentistry began during the middle of this decade when it was used for manufacture of intra-root posts and crowns manufactured with CAD/ CAM as well as appliances for rehabilitation of dental implants and fixed partial prostheses.4–6 To the present date, zirconia treatments, due to their high values of fracture resistance, have become ideal candidates to manufacture ceramic prostheses in areas of high mechanical compromise.
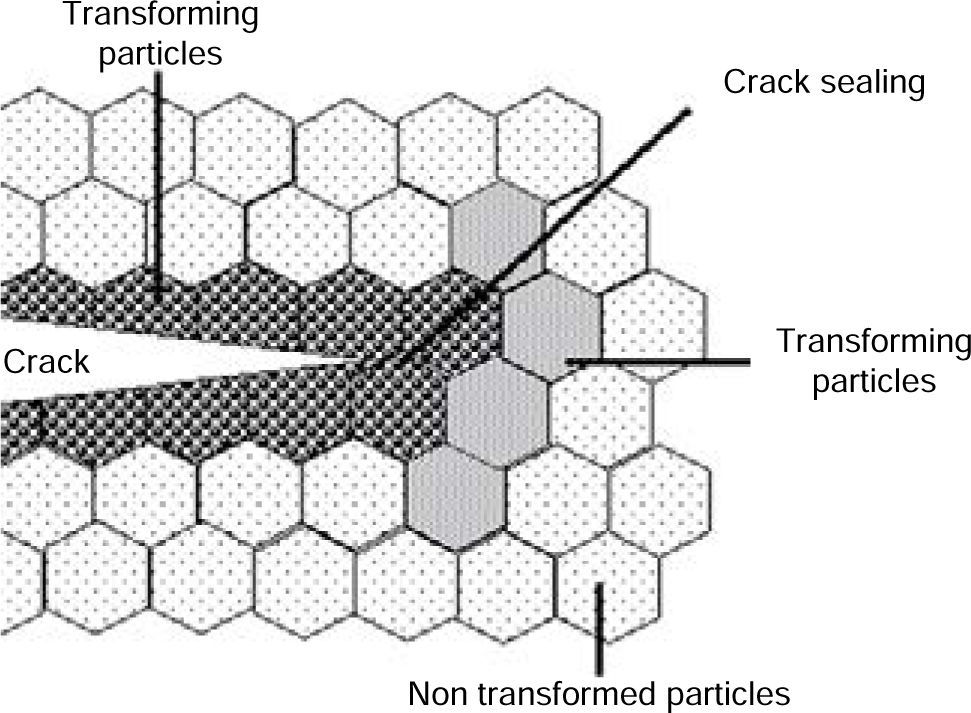
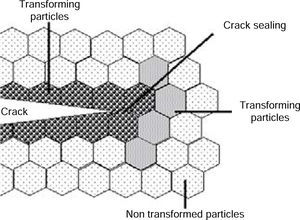
The main attribute of Y-TZP (Yttria tetragonal zirconia polycrystalline) was described by Garvie in 1975, when he described the resistance to transformation phenomenon, in which, partially stabilized zirconia in tetragonal phase, in the presence of a high stress area such as the extreme of a crack, suffers phase change in that area, passing to crystalizing that area in the monoclinic phase. This change involves an approximately 5% volume increase of the zirconia particle, able to seal the crack. Thus, healing of the area is ultimately achieved arresting crack increase (Figure 1).7
Y-TZP is a fracture-resistant material with excellent mechanical properties, it is considered to be biotolerable, and provides flexural strength of more than 900-1200 MPa, these are values two to three times higher than maximum mastication forces (200 to 400 N in anterior teeth and up to 600 N in posterior teeth). This flexural strength is higher than that exhibited by any other previously developed ceramic materials for dental use.8 It also exhibits a yield strength higher than almost all metallic alloys used in dentistry, its elasticity module (205 GPa) is somewhat lower than that exhibited by stainless steel (210 GPa) and similar to that of titanium alloys (Ti6Al4V);9 it presents thermal conductivity lower than alumina (zirconium 2.5 W 7 Mk versus alumina 30 W7mk at 37°C),8 therefore, probability of triggering hypersensitivity in the case of sudden thermal changes is decreased.
It is a highly biotolerable material10 with low radioactivity, with radio-opacity similar to that of metals,11 allowing thus excellent radiographic contrast.
Nevertheless, zirconia is not devoid of problems, among them we can count spontaneous degradation (related to hydro-thermal transformation) and stress derived from manufacturing process.12 With respect to an ideal cementing agent, even though many research projects have been conducted, to this date, there are no strong results to help us determine which cementing system can be more suitable or more effective, therefore, protocols with resinous cements as well as glass ionomer protocols are recommended.13,14
Zirconium is an acid-resistant ceramic material, differing from vitreous porcelains, it does not react to acid etching, moreover, it is quite unstable when subjected to thermal and mechanical changes.15 Traditional protocols of acid etching with hydrofluoric acid and silanization used to adhere other ceramic structures to dental structure are not applicable to zirconia, since there is absence of vitreous matrix and its nature is relatively inert; this renders it a low reactivity surface.16,17 Development of selective acid etching methods, sanding or infiltration have been attempted in order to prime zirconium surfaces to chemically or micromechanically adhere to dental structure with the use of resinous cements, targeting improvement of their mechanical properties without generating stress on the structure which might cause fractures and thus lead to failure.14,18 Nevertheless, to the present date, there are no studies to support effectiveness and durability of new protocols proposed for roughness generation (sanding, three-fold mechanical/chemical treatment, porcelain pearls, plasma spray) and thus chemically activate the zirconia surface (silanization, acrylization, silicon tetrachloride vaporization, MPD silanes and cements).19
Presently the most widely used technique to cement zirconia restorations would be use of sanding with aluminum oxide micro-spheres (50-110μ, 2 to 3 pressure bars, 3 to 4 cm distance) along with cementing agents which contain phosphate monomers (MDP)8,19 are perhaps the technique more frequently used to cement zirconia restorations. It has been shown that cements containing monomer 10 metacryloxydecyl dihydrogen phosphate (MDP) exhibit particular affinity to metallic oxides such a zirconium dioxide, alumina and metal. MDP is a relatively hydrophobic monomer, due to its 10 carbons chain; it contains a hydrophil phosphate terminal which chemically adheres to zirconium oxide, and a polymerizable methacrylate terminal which adheres to resin.20
It is important to point out that tooth preparation is paramount among multiple factors leading to success of fixed restorations, as a factor of great influence in the retention degree of the restoration irrespectively of used material. Preparation of an abutment with convergence angles oscillating from 4o and 15o21,22 is widely found in the descriptions of clinical procedures of several follow up studies of zirconia restorations. It has been shown that decreasing the preparation's convergence degree to 10o exponentially increases retention degree,23 irrespectively of used cement.
MethodResistance to displacement of four cementing agents was compared, out of them, three agents were self-adhesive, dual polymerization cements with MDP content, and the remaining one was a conventional, glass ionomer cement. All cements were commonly used at the final stages of a zirconia rehabilitation. Cements were compared in order to determine which one would represent the best option for the aforementioned process.
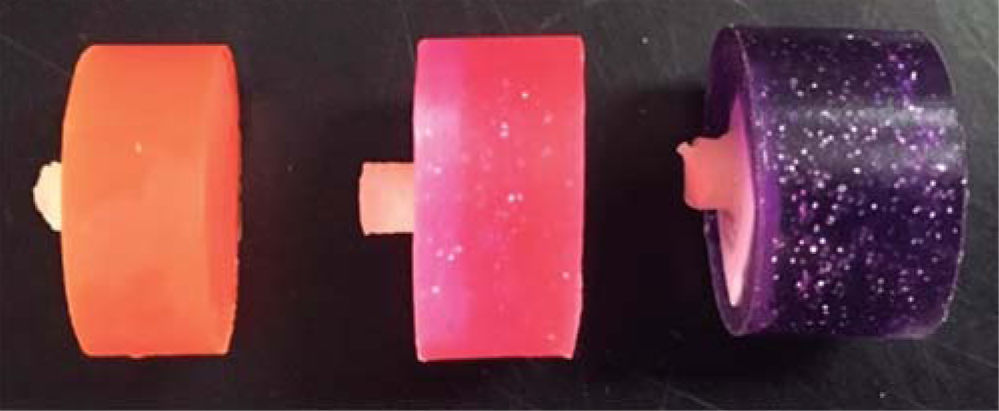
The following cements were studied (Figure 2):
RelyXTM Ultimate with Single Bond® Universal, 3M™ ESPE™.
Multilink® Automix with Monobond® Plus, Ivoclar Vivadent.
PANAVIA™ SA Cement Automix, Kuraray Noritake Dental Inc.
Ketac Cem, 3M™ ESPE™.
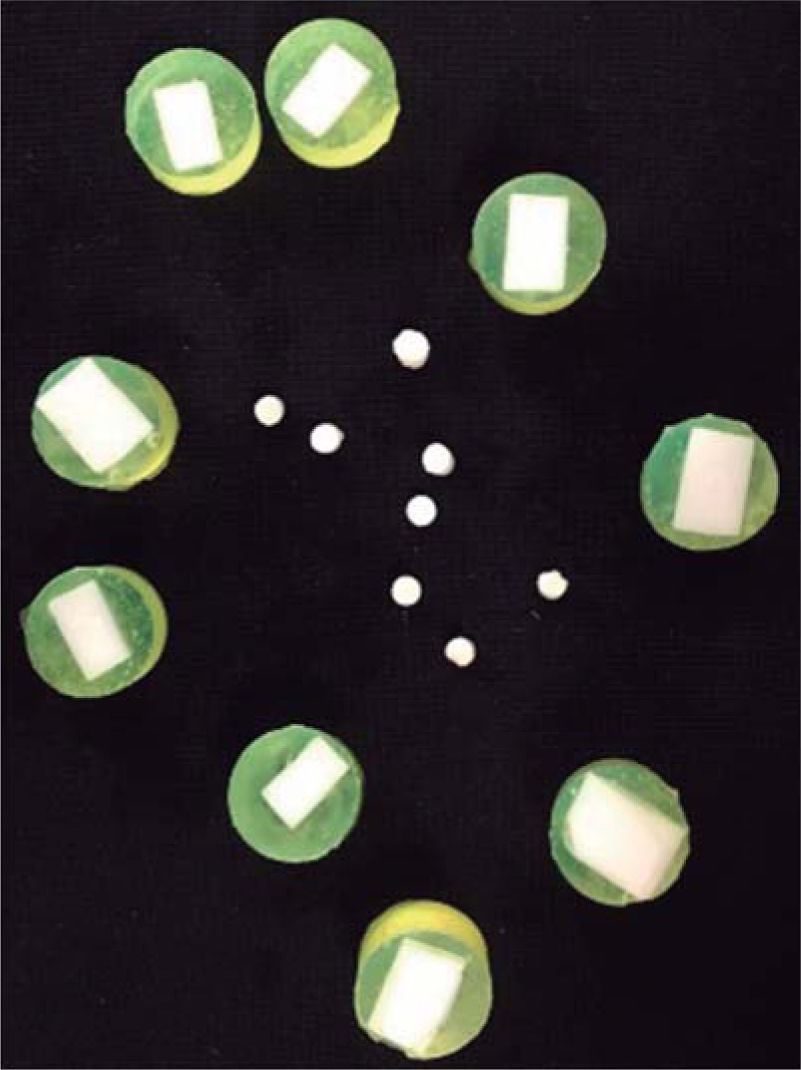
Forty 7 x 7 mm square samples of Zirconia LavaTM Plus, 3MTM ESPETM were obtained. They were sintered at 1,450 o C for 8 hours, according to manufacturer's instructions in an oven program S1P1600, Ivoclar Vivadent. Zirconia samples were soaked with PMM (methyl polymethacrylate), in 25 mm diameter polypropylene rings, using a different color for each study group (Figure 3). All samples were sanded with 50μ aluminum oxide spheres; as part of the cleansing process; samples were taken to a Branson 2510 ultrasound appliance for one minute. A Teflon shaper with a 4 mm orifice was used; with a press, cements to be tested were placed on the zirconia. In the first group, Multilink® Automix (Ivoclar Vivadent) was placed, after having applied bonding agent Monobond® Plus, of the same commercial brand.
Group 2 was previously treated with Single Bond® Universal (3MTM ESPE) as previous bonding agent, same procedure as previous group was undertaken with cement RelyX Ultimate 3MTM ESPETM.
Group three was achieved with PANAVIATM SA Cement Automix, Kuraray Noritake Dental Inc.
Group four was undertaken with Ketac Cem (3MTM ESPETM).
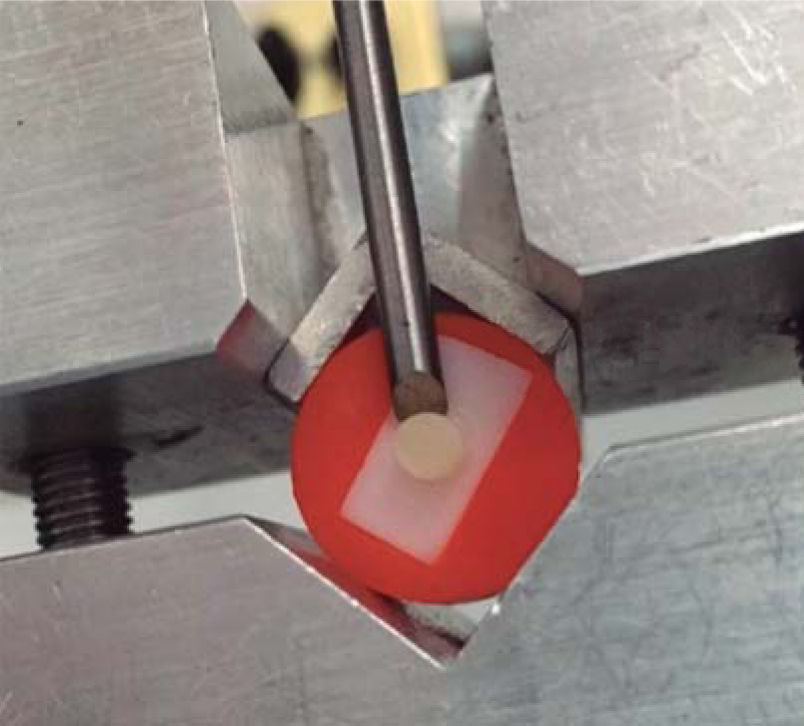
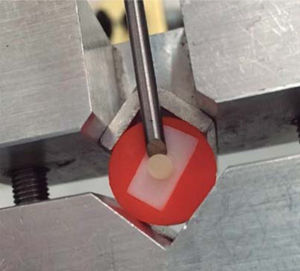
All cements were handled according to manufacturer's instructions. Light-polymerizing cements were cured with an Ultradent Products Inc lamp at 600 mW/cm2 power, measured with a Demetron brand radiometer and following timing established by manufacturer of each cementing agent. Specimens were then stored at 100% humidity in a chamber at 37 oC for 24 hours. In each sample area was calculated with the formula π x r2, area of all specimens was obtained in this manner. Mechanical test of dislodgment by shearing was conducted at a 1 mm per minute speed, in order to observe adhesion strength , a universal machine for mechanical tests Instron® model 5567 USA was used (Figure 4).
Result analysisOnce obtained, results were subjected to variance analysis test of one factor (ANOVA). Informative package SigmaStal® was used.
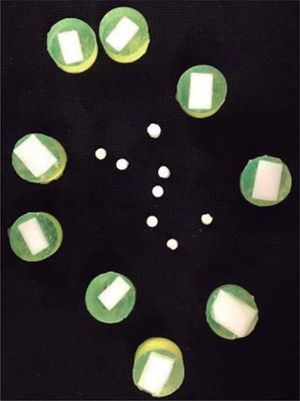
Ketac Cem (3MTM ESPETM) glass ionomer samples were discarded, since during manufacturing, all 10 samples failed (Figure 5).
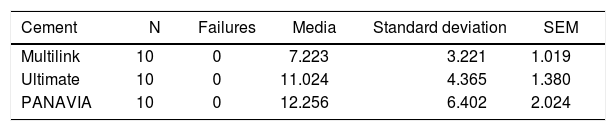
According to standard deviation, the study was reliable for the following cements: Multilink® Automix Ivoclar Vivadent. Relyx TM Ultimate 3MTM ESPE. PANAVIATM SA Cement Automix (Kuraray Noritake Dental Inc). Average values of retention forces of 7.223 MPa, 11.024 MPa and 12.256 MPa, respectively were reported (Table I).
ANOVA test with p = 0.170 to compare displacement resistance of the three cements revealed that there was no statistically significant difference with value p = 0.070. Post hoc tests were additionally performed, and likewise, it could be observed there were no statistically significant differences among groups, even though there was a 5 MPa difference range among cements of greater and lesser retention.
Null hypothesis was accepted based on results obtained in the present research project which had proposed that «there is no difference in resistance to displacement among cementing agents».
DiscussionBased on data obtained from the tests, it was decided to exclude glass ionomer from the statistical analysis. Ernest et al (2005),16 Marchan et al (2005)24 and Uo et al (2006)25 reported that conventional ionomer showed very low retention values when used with zirconia. When comparing 5.8 MPa PANAVIA with Ketac Cem, Shahin and Kern reported results that showed that PANAVIA 21 exhibited best behavior as adhesion agent in the retention of zirconia structures without surface treatment and reported approximately 2.8 MPa.26
Results of the present research confirm that null hypothesis; results obtained were similar to those of Palacios et al (2006)15 who tested three cements (PANAVIA F 2.0, Kuraray; RelyX Luting, 3M ESPE and RelyX Unicem, 3M ESPE), when they reported bonding to zirconia with no statistically significant differences.
Cements used in the present work are resinous cementing agents containing MDP in their formula. Kern and Wenger, in 199827 were the first to report long term adhesion strength of MDP-containing resinous cements; this was later confirmed in numerous studies.28–31Bonding agents have been developed in recent years. They have been introduced to improve bonding strength of ceramic to zirconium. When using RelyX ® Elite and Multilink ® Automix, the manufacturer recommends, in an alternative manner, to use systems with imprinters or bonding agent Single Bond® Universal, 3MTM ESPETM and Monobond® Plus, Ivoclar Vivadent respectively. In both cases, imprinters contain dihydrogen phosphate 10-methacryloxydecyl (MPD) and silanium. Numerous studies such as those of Amaral et al, Ozcan at al and Yoshida et al support the use of imprinters with MDP on zirconium oxide surfaces, since obtained results have shown that phosphate monomers are securing chemical agents in order to improve bonding to zirconia.20,30,31
It has been concluded that roughness and activation of zirconia are important in order to achieve bonding of resin to the restoration. Many researchers (Bopna, Kern, Blatz among others), used abrasion techniques with aluminum oxide particles sanding on the restorations surface so as to increase surface energy, adhesion area and humectability.32
McLauglin (1984) Corts (2003 and 2010) reported that either way and regardless of preparation to the zirconia surface, it is important to know that there will be no «integration» or «fusion» of restorations to the dental structure, as would be the case when using restorations with vitreous phase, treated with hydrofluoric acid and later silanized.33–35
ConclusionsWithin limitation of the present study and taking into account it was conducted both in vivo and in vitro, it is possible to conclude the following:
- •
Glass ionomer adhesion capacity to zirconia is nil or extremely low.
- •
Presently, the best alternative to increase adhesion to a zirconia surface are resinous cements containing MDP in their formulation, either in their bonding agent or in the cement formula itself.
- •
To this date no statistically significant differences have been found among the three studied cements. PANAVIA offers a simplified placement technique, that is to say, it does not require bonding agents, thus decreasing probability of failure during cement manipulation. • No studies have been found that support satisfactory cement adhesion to zirconia or in a similar manner to that achieved by vitreous phased ceramics.
- •
It is important to mention that in addition to technique or treatment applied to zirconia surfaces, long term success of the restoration is related to application of basic principles in the design preparation.
- •
We recommend conducting long term in vivo research projects in order to observe behavior of cementing agents used in zirconia oxide restorations.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
Graduate and Research School. National School of Dentistry, National Autonomous University of Mexico
Health and Biological Science Division, Healthcare Department, Metropolitan Autonomous University, Xochimilco campus
Division of Professional studies. National School of Dentistry, National Autonomous University of Mexico