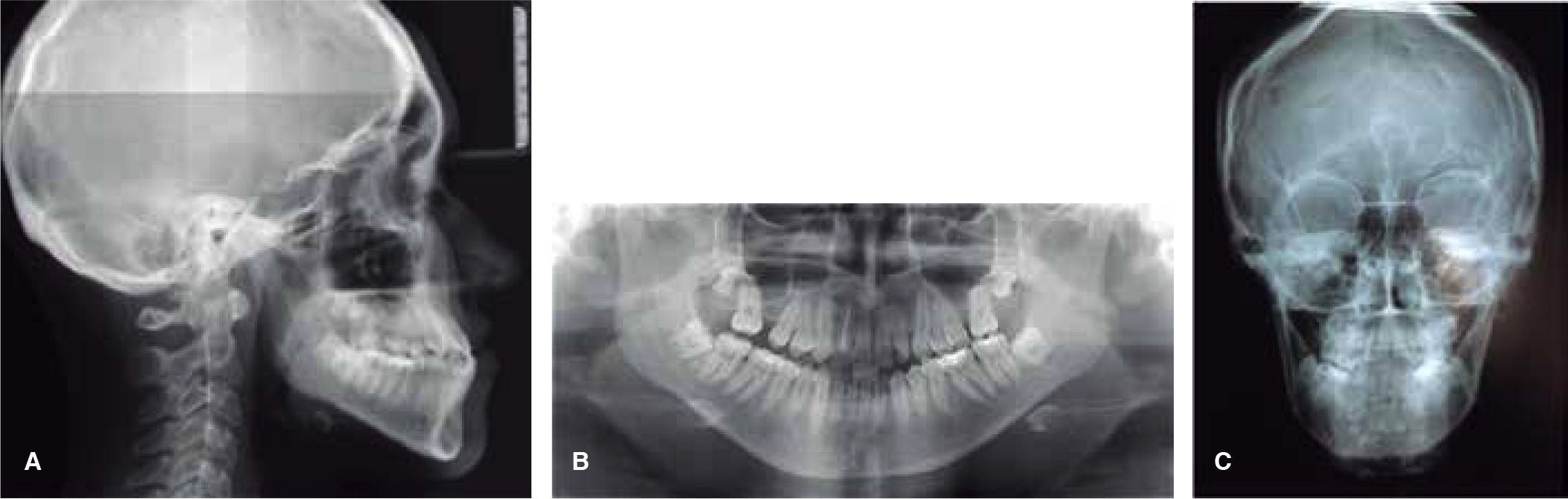
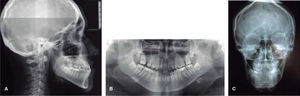
Female patient, 16 years of age, who attended the Department of Orthodontics at the National Autonomous University of Mexico. The main reason for consultation was: «I have a deviated jaw». Upon facial clinical examination, from the front view an oval and elongated face may be noted as well as an increased lower third, the chin deviated to the right, the facial midline did not match the dental midline, a non-consonant neutral smile and a 60% exposure of the incisor clinical crowns. On a lateral view: a straight profile, competent lips, acute nasolabial angle and increased mentocervical length may be observed. Intraorally there is an ovoid-shaped arch, non-coincident dental midlines, crowded teeth, anterior and posterior right crossbite, absence of the first upper molars (nonassessable molar relationship) right and left canine class III, -2mm overjet and a 2mm overbite. Radiographic records included a lateral headfilm, a posteroanterior radiograph and a panoramic radiograph as well. The cephalometric analysis revealed a skeletal Class III due to mandibular prognathism, a neutral growth pattern, proclined upper incisors and lower incisor retroclination. The posteroanterior radiograph showed a discrepancy of the maxillo-mandibular line of 4o and a postural asymmetry of 5o. In the panoramic radiograph asymmetric mandibular ramus, ACJ at alveolar crest level, 2: ¼ root-crown ratio, upper and lower third molars, absence of the first upper molars and maxillary lateral incisor root with endodontic treatment may be noted. Functionally, the patient presented without any apparent TMJ problems. Treatment consisted of three phase: pre-surgical orthodontic phase, surgical phase and post-surgical orthodontic phase. The objectives were: to correct in all three planes of space the skeletal disharmony presented by the patient, to provide functional occlusion and optimal facial and dental aesthetics as well as joint stability and periodontal health.
Paciente femenino de 16 años de edad acude al Departamento de Ortodoncia de la Universidad Nacional Autónoma de México. Su motivo principal de consulta: «tengo la mandíbula chueca». Al examen clínico extraoral, en vista frontal se observó forma de cara alargada, ovalada, el tercio inferior aumentado y mentón desviado hacia la derecha, la línea media facial no corresponde con la línea media dental, sonrisa neutra no consonante, exposición dental del 60% de las coronas clínicas. En vista lateral, perfil recto, competencia labial, ángulo nasolabial agudo y longitud mentocervical aumentada. Intraoralmente, forma de arcada ovoidal, líneas medias no coincidentes, apiñamiento dental, mordida cruzada anterior y posterior derecha, ausencia de los primeros molares superiores, relación molar no valorable, clase III canina derecha e izquierda, sobremordida horizontal -2mm y sobremordida vertical de 2mm. Los registros radiográficos incluyen lateral de cráneo, posteroanterior y ortopantomografía. En el análisis cefalométrico reveló una clase III esquelética por prognatismo mandibular, patrón de crecimiento neutro, incisivo superior proclinado, incisivo inferior retroclinado. En la radiografía posteroanterior presentó una discrepancia de la línea maxilomandibular de 4o y la simetría postural de 5o. En la ortopantomografía se observaron las ramas mandibulares asimétricas, crestas alveolares a nivel de la unión amelocementaria, proporción corono-raíz de 2:11/4, presencia de los terceros molares superiores e inferiores, ausencia de los primeros molares superiores y el incisivo lateral superior derecho con tratamiento endodóntico. Funcionalmente, sin problema articular aparente. El tratamiento consistió en tres fases de tratamiento, la fase ortodóncica prequirúrgica, la fase quirúrgica y la fase ortodóncica postquirúrgica. Los objetivos del tratamiento fueron la corrección en los tres planos del espacio; la desarmonía esqueletal, proporcionar una oclusión funcional y una estética facial óptima, de igual forma obtener una buena estabilidad articular y salud periodontal para una mejor calidad de vida del paciente.
Dentomaxillofacial anomalies are complex and difficult to treat because they affect multiple structures and involve the lower third of the face. When these problems occur and changes in growth modification and orthopedic treatments are not able to solve them, the most favorable option is a combined surgical orthodontic treatment, which should be coordinated properly to get the most benefit for the patient.1
Skeletal class III malocclusion is the lack of harmony between the maxilla and the mandible distorting facial aesthetics and masticatory function.2
Facial asymmetry is a common manifestation in patients with class III malocclusion that affects functional occlusion as well as the aesthetic appearance of the face, decreasing the patient's quality of life. This is one of the main reasons for consultation.3
Generally patients who are candidates for orthognathic surgery have a natural compensation to their malocclusion. Therefore, it is of utmost importance to inform the patient that at the time of orthodontic decompensation, the asymmetry and the maxilofacial discrepancy will be more apparent.4
When deciding on treatment, it must be must considered the limits of orthodontics and surgery, which vary depending on several factors such as: (a) The necessary dental mobilization; Dr. Richard McLaughin mentions that the maximum dental inclinations for a class III patient are 10° higher than the norm for upper incisors and 10o lower for lower incisors, in order to achieve an acceptable stability, b) Limitations established by the soft tissues, c) Function and d) psychosocial and aesthetic considerations.5
Ackerman and Proffit recommend the clinician not to overlook the limitations of the soft tissues during treatment planning. These tissues involve several constraints: (1) the pressures exerted on the teeth by the lips, cheeks, and tongue are a major determinant for stability, (2) periodontal health, (3) temporomandibular joint and muscles have an important role in function, (4) the soft tissues of the face which determine aesthetics.6
The evolution in diagnosis and treatment of this kind of patients has developed extensively in recent decades. Obwegeser popularized the sagittal osteotomy of the ramus with a predictable intraoral technique for the correction of dentofacial problems, removing the facial scars left by the external approaches.7
In different articles8 it has been mentioned that with current surgical techniques the results and long-term stability for patients who undergo orthognathic surgery combined with orthodontics are highly successful.
Orthodontic treatment consists in dental alignment of both arches, decompensating the current dental positions and placing the teeth within their basal bone, so that after orthognathic surgery a good occlusion might be achieved. Surgical objectives focus on obtaining a good balance and facial harmony relating the maxilla and the mandible on the same plane.9
CASE REPORTA female patient of 16 years of age attended the Orthodontic Clinic of the Division of Post-Graduate Studies and Research in the Faculty of Dentistry of the UNAM. Her reason for consultation was: «I have a deviated jaw». Apparently, the patient was healthy.
Clinical features. The facial clinical examination revealed in the front view an elongated oval- shaped face, an increased lower third, her chin was deviated to the right, the facial midline did not correspond with the dental midline; a neutral non-consonant smile and 60% tooth display. In the profile view, a straight profile, lip competence, acute nasolabial angle and an increased mentocervical length. Intraorally, the patient presented an ovoid arch form, non-coincident dental midlines, crowding, anterior and posterior right cross bite, absence of the first upper molars, non-assessable molar relationship, canine class III, a -2mm overjet and an overbite of 2mm. The radiographic records included posteroanterior and panoramic radiographs as well as a lateral head film. The cephalometric analysis revealed a skeletal III due to mandibular prognathism, a neutral growth pattern, proclined upper incisors and retroclined lower incisors. In the posteroanterior radiograph, the patient showed a discrepancy of the maxillomandibular line of 4o and a 5o postural symmetry corroborating the facial asymmetry of the lower third and laterognathia. In the orthopantomography asymmetric mandibular ramus, alveolar crest at the level of the enamel-cementum junction, root-crown ratio of 2:11/4, presence of the upper and lower third molars, absence of the first upper molars and the upper right lateral incisor with endodontic treatment were observed. Functionally, there was no apparent joint problem (Figures 1 to 3).
Treatment planThe patient was referred to the Department of Oral and Maxillofacial Surgery of the Division of Post-Graduate Studies and Research in the Faculty of Dentistry of the UNAM for the removal of the upper and lower third molars.
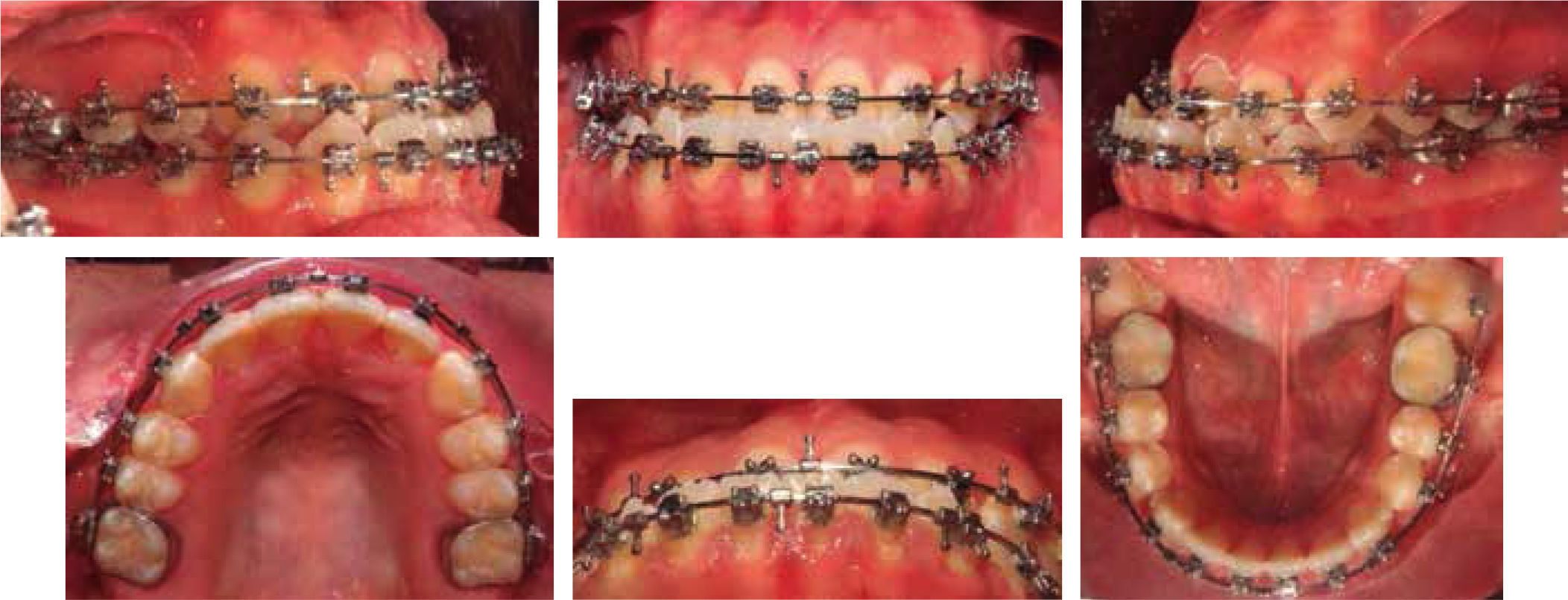
Orthodontic phase-before surgery: treatment was begun with 0.022” × 0.028” slot Roth system. The phases of alignment, leveling, second and third order movements, elimination of the curve of Spee, Wilson and arch coordination were performed. Subsequently, neuromuscular deprogramming was conducted for three months before the surgery (Figure 4).
Pre-surgical records were obtained; the surgical prediction and models surgery were performed according to protocol.
Surgical phase. In coordination with the Department of Oral and Maxillofacial Surgery, it was decided to perform an anterior segmental osteotomy with a 3mm rotation, bilateral sagittal osteotomies of the mandibular ramus and an advancement genioplasty of 4mm (Figure 5).
Postsurgical orthodontics phase: immediate control, leveling, consolidation, stabilization of the case, settlement and occlusal balance was performed. For retention it was indicated an upper fixed retainer and a lower circumferential retainer (Figure 6).
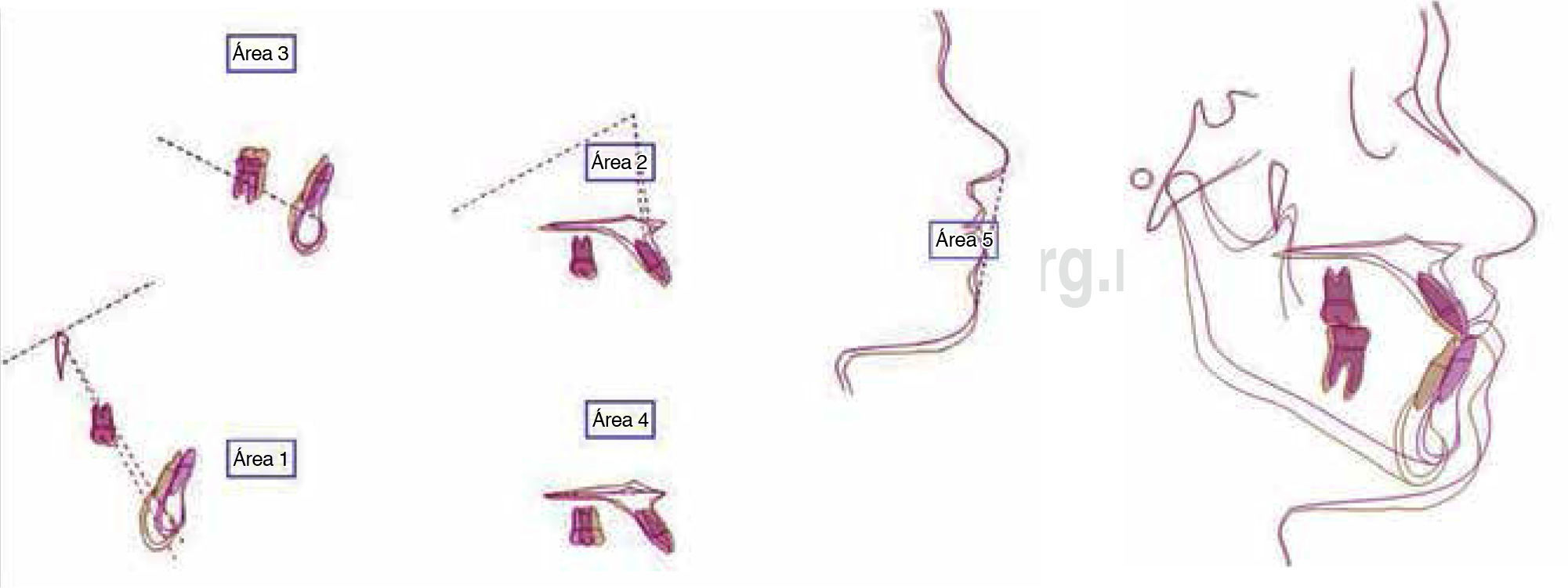
Final X-rays and photographs were obtained and changes with the treatment were assessed by superimposition. The obtained dental, skeletal facial and functional results were satisfactory (Figures 7 and 8).
RESULTSTreatment time was 29 months. Interdisciplinary coordination was favorable. It was possible to correct the facial asymmetry, a skeletal class I was obtained as well as a straight profile, a positive, consonant Treatment time was 29 months. Interdisciplinary smile thus providing facial balance and harmony of the coordination was favorable. It was possible to correct soft tissues.
A correct functional occlusion was achieved, molar and canine class I, a normal overjet and overbite and coincident dental and facial midlines.
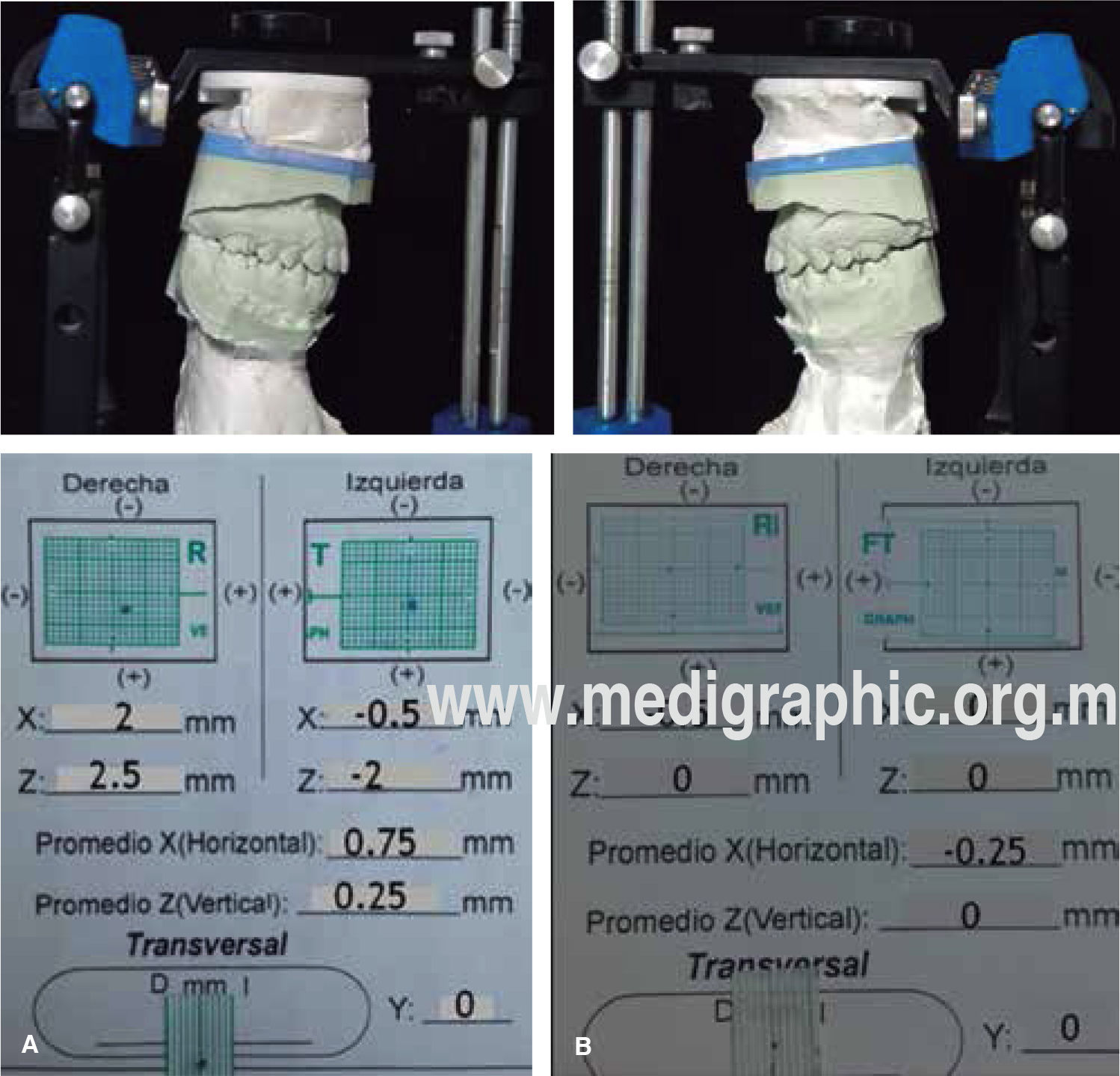
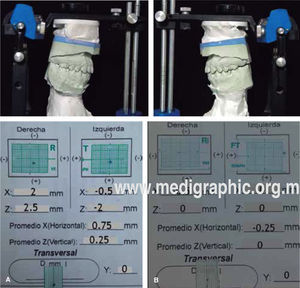
A record of condylar position was taken five months after appliance removal and it showed a coincidence of centric relation and centric occlusion (Figure 9).
At the end of treatment there was a notable increase of self-esteem in the patient.
DISCUSSIONIt is believed that Class III malocclusion is a polygenic disorder that results from an interaction between susceptible genes and environmental factors.
Many authors propose that treatment effectiveness should be assessed on the basis of the objectives for soft, dental and skeletal tissues. It has been reported that the ranges of post-treatment cephalometric values are acceptable.10
Proffit reports that a correct overjet is obtained in 95% of patients.11
Bimaxillary surgery is a procedure that is used in 75% of patients who have a severe skeletal and dental discrepancy.
In surgical orthodontic treatments an interdisciplinary work and adequate communication must be maintained in order to be able to fulfill the objectives of each treatment.12
CONCLUSIONSIt is important to perform a thorough diagnosis to determine the appropriate treatment for each patient to obtain functional, harmonic and aesthetic results. Patient cooperation is essential.
In the treatment of class III malocclusion with asymmetry a good diagnosis, treatment plan, presurgical orthodontic preparation, orthognathic surgery and postoperative control are required. Thanks to this it was possible to obtain optimal results in order to meet the expectations of the patient.
The success of this clinical case was based on good interdisciplinary communication and treatment planning.