To describe sociodemographic and diagnostic characteristics of indigenous patients (identified by determining whether they speak an indigenous language) hospitalised between January 2014 and January 2015 at the Hospital General de Mexico, and to analyse these characteristics using a vulnerability classification.
Materials and methodsA descriptive, cross-sectional study of hospital data and a bivariate analysis using vulnerability as a dependent variable and those variables described in the socioeconomic study as independent variables.
ResultsOf 47,733 patients hospitalised, 816 (1.7%) were speakers of indigenous languages, with Náhuatl being the most common indigenous language (31.3%); 98.6% did not have health insurance coverage and 45.9% were classified as vulnerable patients; 62% did not receive an income. 77% were from Oaxaca, State of Mexico, Veracruz, Puebla and Hidalgo; however, 59.1% were living in Mexico City and the State of Mexico. The most frequent diagnoses were neoplasms (21.4%), followed by diseases of the digestive system (16.3%). 53% reported that they had been dealing with their illness for more than 6 months. The household and family income variables were strongly linked to vulnerability.
ConclusionsThis study demonstrates the precarious living conditions of hospitalised indigenous peoples and the difficulties they face in fighting diseases given their socioeconomic conditions. Recommendations are made to address the way the indigenous peoples are identified in the hospital, on recognising them as a vulnerable population, as well as the need for records of sociodemographic and health information regarding this population in hospital settings, so that it is reliable and comparable and to serve as a strong case for the implementation of local actions which meet national and international standards.
Describir las características sociodemográficas y diagnósticas de pacientes indígenas (identificados con el criterio de hablar una lengua indígena) hospitalizados entre enero de 2014 y enero de 2015 en el Hospital General de México y analizar dichas características a partir de la clasificación de vulnerabilidad.
Materiales y métodosEstudio transversal descriptivo de datos hospitalarios y análisis bivariado tomando como variable dependiente el ser o no vulnerable y como variables independientes las descritas en el Estudio Socioeconómico.
ResultadosLos pacientes indígenas hospitalizados fueron 816 (1.7%). El náhuatl fue la lengua indígena más frecuente (31.3%); el 98.6% no tenían seguro social y el 45.9% fueron clasificados como pacientes vulnerables. El 62% de esta población no percibían un ingreso económico. El 77.9% reportaron ser originarios de Oaxaca, del Estado de México, Veracruz, Puebla e Hidalgo; sin embargo, el 59.1% vivían en Ciudad de México y el Estado de México. Las categorías diagnósticas más frecuentes fueron las neoplasias (21.4%) seguidas de los problemas digestivos (16.3%). El 53% reportaron padecer el problema de salud por más de 6 meses. Las variables relacionadas a la vivienda y los ingresos familiares se asociaron de manera significativa a la condición de vulnerabilidad.
ConclusionesEste estudio evidencia las condiciones de vida precaria de los indígenas hospitalizados y las dificultades para enfrentar la enfermedad dadas sus condiciones socioeconómicas; se recomienda atender a la manera como se identifican los indígenas en el hospital, al reconocimiento como población en condición de vulnerabilidad y a la necesidad de realizar registros de información sociodemográficos y de salud con respecto a esta población en contextos hospitalarios, que sean confiables y comparables para que sirvan de argumento sólido a la implementación de acciones locales que obedezcan a la normatividad nacional e internacional.
One of the major issues in relation to the healthcare of indigenous communities worldwide is the record of reliable and specific epidemiological data.1 In Mexico, the under-recording of morbidity in this group is apparent2 and there are few sources to provide in-depth knowledge of the health status of indigenous populations. In Latin America, indigenous health information is scattered and there are no databases documenting health outcomes, either in time or within specific communities,3 except for Chile.4–9 At present, there are no known differential hospital records in Mexico.
In order to prepare health records for these groups, individuals must first be identified as belonging to an indigenous group, which has been the subject of wide international and national debate.1,3,10–14 In Mexico, the criteria used for identification have been diverse: national censuses and surveys consider the language spoken and, recently, self-identification; in these terms, the population that speak an indigenous language in Mexico is 6.7 million people, representing 6.6% of the total population, while those who consider themselves indigenous reaches 15.7 million people, i.e. 14.9% of the population are aged 3 years or older.15 On the other hand, the National Commission for the Development of Indigenous Peoples of Mexico (CDI) identifies them as those who are part of an indigenous household, where one of the members claims to speak an indigenous language; as well as people who claimed to speak an indigenous language but are not part of these households.16 Different criteria generate differences in the number of Mexican indigenous people which could lead to forms of exclusion,17 or inclusion of others who, due to proximity, are considered indigenous. Despite the controversy, when it comes to healthcare, it is essential to identify this population under some explicit criteria, record information on social and healthcare quality differentials, and apply national and international recommendations to mitigate the inequality suffered by these people.
Due to socioeconomic conditions and lack of protection of their human rights, indigenous people have been considered as a vulnerable population. At present, the definition of vulnerability has a wide range of conceptual approaches and usage applications, as well as a variety of phenomena with which it is associated.18–23
Among the variety of definitions, in this article we opted for the concept of health vulnerability, which refers to “the relative vulnerability of a population group facing either potential damage to their health, threats to the satisfaction of their personal needs or violation of their human rights due to lack of personal, family, community, social, economic or institutional resources”.22
Since its foundation, Hospital General de México “Dr. Eduardo Liceaga” (HGM) has been a leading institution in Central Mexico, which serves members of the population living in poverty-stricken conditions. Since 79.3% of the indigenous-language speaking population in Mexico lives in conditions of poverty and extreme poverty,24 some of the patients who seek medical care at HGM may belong to these groups.
The purpose of this document is to describe the sociodemographic characteristics of the indigenous population that seek care in HGM and the diseases that afflict them; as well as to analyse the relationship between the variables studied and the vulnerability classification assigned by the hospital.
This information will provide an insight into their living conditions, as well as their social and healthcare needs, in order to make this group visible within the institution so that hospital authorities develop healthcare proposals according to the specific characteristics of this population. It also intends to highlight problems related to the identification and care process in this particular context and recommend any adjustments which should be made.
MethodsThis is a descriptive, cross-sectional, hospital-based study involving subjects who speak an indigenous language, and who were hospitalised and recorded in the HGM Comprehensive System of Hospital Administration (SIAH) during the period from January 2014 and January 2015. The SIAH records all the information from the Socioeconomic Study (SES) that uses Social Work and the discharge diagnosis, issued in accordance with the International Classification of Disease (ICD-10),25 as well as administrative data such as date of hospital admission and discharge. The information from the SES is collected by each social worker in the system. The diagnostic information is provided by the attending physician. The selection criterion was speaking an indigenous language and the variables studied were:
Individual variables: age, gender, marital status, education, occupation (classified by a list of trades in the system, and where this is not on the list, “other” is selected), religion, language (chosen from among all the indigenous languages of Mexico), state of origin, state of permanent residence, temporary residence (place different from permanent residence).
Family variables: relationship of the person responsible (relationship of the person, whether a family member or not, responsible for the patient to the institution and who provides information), occupation of the main family provider, family group (number of people who make up the patient's family, who are economically dependent on the same income and living in the same household), income (breakdown and total amount of monthly income of people who regularly contribute to the family income) and expenditures (average household monthly expenses reported by the patient) and the income-expenditure ratio (total expenditure multiplied by 100 divided by the total income; the percentage obtained, will automatically fall among 6 possible levels, where the higher the percentage, the lower the score).
Housing and public service variables: tenure (whether or not the property where the patient and family live is owned by them), type of dwelling (classification established based on the structure of the dwelling, from cave, welfare institution or house), extra-domiciliary services, intra-domiciliary services, construction materials, number of bedrooms, people per bedroom.
Health-related variables: duration of illness (self-report on how long the current health issue has persisted), comorbidities (other self-reported health issues that are not the reason for consultation), diagnosis (diagnostic category to which the disease belongs according to ICD-10, provided on the hospital discharge report).
Hospital care-related variables: access to healthcare (belonging to one of the social security institutions such as the Mexican Social Security Institute, the Institute of Security and Social Services of State Workers), vulnerability (classification at the discretion of the social worker; it is not described in the instructions for completing the SES) and the socioeconomic level (product of the automatic sum of the scores obtained in each of the variables registered by the SES). The allocation of the socioeconomic classification is mainly related to the following items: household income (55% weighting), occupation (10%), family expenses (10%), housing (20%) and family health (5%). The score obtained in the socioeconomic assessment does not exceed 100 points: 0–12 points is level 1X; 13–24, level 1; 25–36, level 2; 37–52, level 3; 53–68, level 4; 69–84, level 5; and 84–100, level 6. This classification will indicate the recovery payment that the patient will pay, where 1X is exempt from payment, 1 refers to the lowest payment amount and 6 to the highest.
A descriptive analysis of the variables was performed, reporting central tendency and dispersion measures of continuous variables and absolute and relative frequencies in ordinal, nominal or categorical variables. A bivariate analysis was also performed, taking the vulnerability classification as the dependent variable and those variables described in the SES as independent variables, using one and two-way variance analysis (ANOVA) for continuous variables and Chi square variable analysis for ordinal, nominal or categorical variables with a significance level of 0.05. STAT A software (v 11.2) was used.
Ethical mattersThis study was approved by the Ethics and Research Committees of HGM (DI/13/404D/04/081).
ResultsThe total number of patients hospitalised during the studied period, who said they spoke an indigenous language was 816, i.e. 1.7% of the total number of patients hospitalised in HGM in the same period (47,733 individuals).
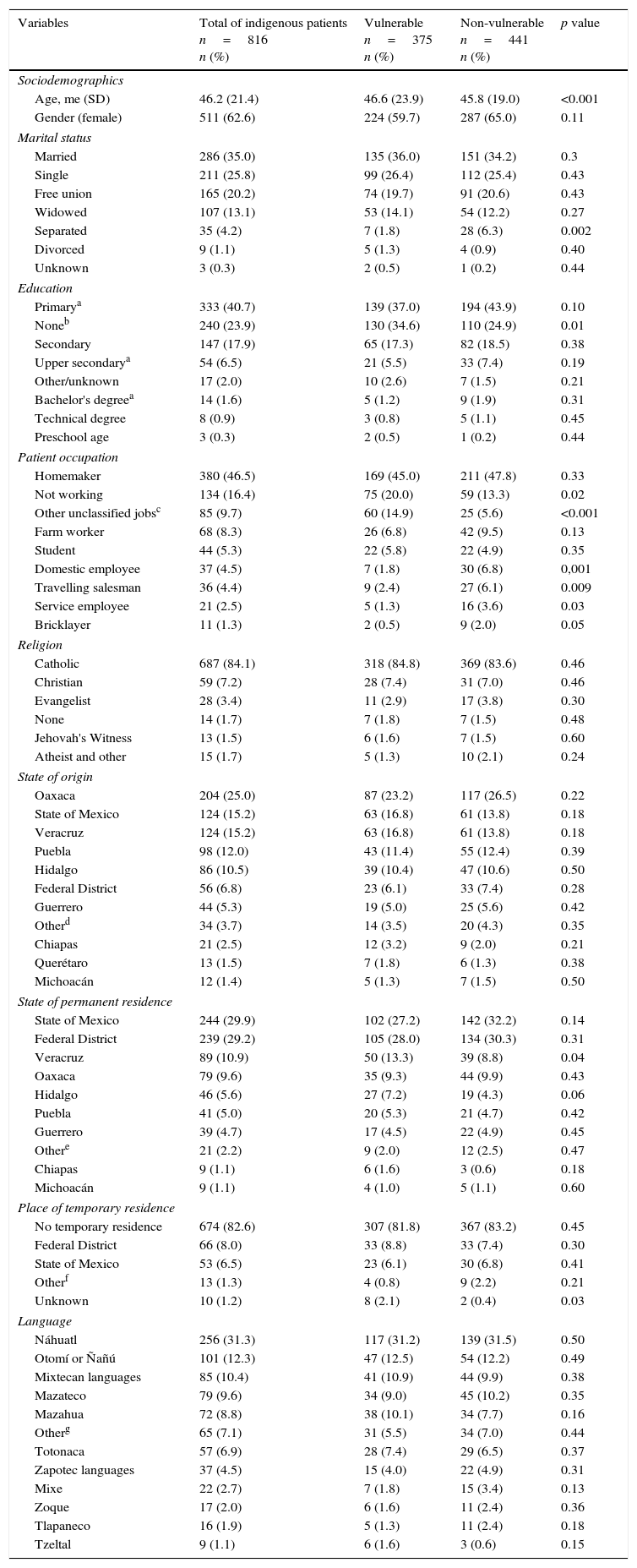
The average age (x¯) was 46.2 years with a standard deviation (SD) of 21.4 years; there were 511 (62.6%) women; from the total, 451 (55.2%) people were married or in a free union. Regarding education, 333 (40.7%) people said they had studied basic primary education (completed or unfinished); 240 (29.3%) did not attend school—this includes both those who know and do not know how to read and write. Regarding the patient's occupation, 380 (46.5%) were homemakers; 134 (16.4%) were without work; 2 (0.2%) were professionals. The detailed description of all individual variables is included in Table I.
Comparison between vulnerable and non-vulnerable indigenous patients hospitalised in HGM between January 2014 and January 2015, taking into account individual variables.
| Variables | Total of indigenous patients n=816 n (%) | Vulnerable n=375 n (%) | Non-vulnerable n=441 n (%) | p value |
|---|---|---|---|---|
| Sociodemographics | ||||
| Age, me (SD) | 46.2 (21.4) | 46.6 (23.9) | 45.8 (19.0) | <0.001 |
| Gender (female) | 511 (62.6) | 224 (59.7) | 287 (65.0) | 0.11 |
| Marital status | ||||
| Married | 286 (35.0) | 135 (36.0) | 151 (34.2) | 0.3 |
| Single | 211 (25.8) | 99 (26.4) | 112 (25.4) | 0.43 |
| Free union | 165 (20.2) | 74 (19.7) | 91 (20.6) | 0.43 |
| Widowed | 107 (13.1) | 53 (14.1) | 54 (12.2) | 0.27 |
| Separated | 35 (4.2) | 7 (1.8) | 28 (6.3) | 0.002 |
| Divorced | 9 (1.1) | 5 (1.3) | 4 (0.9) | 0.40 |
| Unknown | 3 (0.3) | 2 (0.5) | 1 (0.2) | 0.44 |
| Education | ||||
| Primarya | 333 (40.7) | 139 (37.0) | 194 (43.9) | 0.10 |
| Noneb | 240 (23.9) | 130 (34.6) | 110 (24.9) | 0.01 |
| Secondary | 147 (17.9) | 65 (17.3) | 82 (18.5) | 0.38 |
| Upper secondarya | 54 (6.5) | 21 (5.5) | 33 (7.4) | 0.19 |
| Other/unknown | 17 (2.0) | 10 (2.6) | 7 (1.5) | 0.21 |
| Bachelor's degreea | 14 (1.6) | 5 (1.2) | 9 (1.9) | 0.31 |
| Technical degree | 8 (0.9) | 3 (0.8) | 5 (1.1) | 0.45 |
| Preschool age | 3 (0.3) | 2 (0.5) | 1 (0.2) | 0.44 |
| Patient occupation | ||||
| Homemaker | 380 (46.5) | 169 (45.0) | 211 (47.8) | 0.33 |
| Not working | 134 (16.4) | 75 (20.0) | 59 (13.3) | 0.02 |
| Other unclassified jobsc | 85 (9.7) | 60 (14.9) | 25 (5.6) | <0.001 |
| Farm worker | 68 (8.3) | 26 (6.8) | 42 (9.5) | 0.13 |
| Student | 44 (5.3) | 22 (5.8) | 22 (4.9) | 0.35 |
| Domestic employee | 37 (4.5) | 7 (1.8) | 30 (6.8) | 0,001 |
| Travelling salesman | 36 (4.4) | 9 (2.4) | 27 (6.1) | 0.009 |
| Service employee | 21 (2.5) | 5 (1.3) | 16 (3.6) | 0.03 |
| Bricklayer | 11 (1.3) | 2 (0.5) | 9 (2.0) | 0.05 |
| Religion | ||||
| Catholic | 687 (84.1) | 318 (84.8) | 369 (83.6) | 0.46 |
| Christian | 59 (7.2) | 28 (7.4) | 31 (7.0) | 0.46 |
| Evangelist | 28 (3.4) | 11 (2.9) | 17 (3.8) | 0.30 |
| None | 14 (1.7) | 7 (1.8) | 7 (1.5) | 0.48 |
| Jehovah's Witness | 13 (1.5) | 6 (1.6) | 7 (1.5) | 0.60 |
| Atheist and other | 15 (1.7) | 5 (1.3) | 10 (2.1) | 0.24 |
| State of origin | ||||
| Oaxaca | 204 (25.0) | 87 (23.2) | 117 (26.5) | 0.22 |
| State of Mexico | 124 (15.2) | 63 (16.8) | 61 (13.8) | 0.18 |
| Veracruz | 124 (15.2) | 63 (16.8) | 61 (13.8) | 0.18 |
| Puebla | 98 (12.0) | 43 (11.4) | 55 (12.4) | 0.39 |
| Hidalgo | 86 (10.5) | 39 (10.4) | 47 (10.6) | 0.50 |
| Federal District | 56 (6.8) | 23 (6.1) | 33 (7.4) | 0.28 |
| Guerrero | 44 (5.3) | 19 (5.0) | 25 (5.6) | 0.42 |
| Otherd | 34 (3.7) | 14 (3.5) | 20 (4.3) | 0.35 |
| Chiapas | 21 (2.5) | 12 (3.2) | 9 (2.0) | 0.21 |
| Querétaro | 13 (1.5) | 7 (1.8) | 6 (1.3) | 0.38 |
| Michoacán | 12 (1.4) | 5 (1.3) | 7 (1.5) | 0.50 |
| State of permanent residence | ||||
| State of Mexico | 244 (29.9) | 102 (27.2) | 142 (32.2) | 0.14 |
| Federal District | 239 (29.2) | 105 (28.0) | 134 (30.3) | 0.31 |
| Veracruz | 89 (10.9) | 50 (13.3) | 39 (8.8) | 0.04 |
| Oaxaca | 79 (9.6) | 35 (9.3) | 44 (9.9) | 0.43 |
| Hidalgo | 46 (5.6) | 27 (7.2) | 19 (4.3) | 0.06 |
| Puebla | 41 (5.0) | 20 (5.3) | 21 (4.7) | 0.42 |
| Guerrero | 39 (4.7) | 17 (4.5) | 22 (4.9) | 0.45 |
| Othere | 21 (2.2) | 9 (2.0) | 12 (2.5) | 0.47 |
| Chiapas | 9 (1.1) | 6 (1.6) | 3 (0.6) | 0.18 |
| Michoacán | 9 (1.1) | 4 (1.0) | 5 (1.1) | 0.60 |
| Place of temporary residence | ||||
| No temporary residence | 674 (82.6) | 307 (81.8) | 367 (83.2) | 0.45 |
| Federal District | 66 (8.0) | 33 (8.8) | 33 (7.4) | 0.30 |
| State of Mexico | 53 (6.5) | 23 (6.1) | 30 (6.8) | 0.41 |
| Otherf | 13 (1.3) | 4 (0.8) | 9 (2.2) | 0.21 |
| Unknown | 10 (1.2) | 8 (2.1) | 2 (0.4) | 0.03 |
| Language | ||||
| Náhuatl | 256 (31.3) | 117 (31.2) | 139 (31.5) | 0.50 |
| Otomí or Ñañú | 101 (12.3) | 47 (12.5) | 54 (12.2) | 0.49 |
| Mixtecan languages | 85 (10.4) | 41 (10.9) | 44 (9.9) | 0.38 |
| Mazateco | 79 (9.6) | 34 (9.0) | 45 (10.2) | 0.35 |
| Mazahua | 72 (8.8) | 38 (10.1) | 34 (7.7) | 0.16 |
| Otherg | 65 (7.1) | 31 (5.5) | 34 (7.0) | 0.44 |
| Totonaca | 57 (6.9) | 28 (7.4) | 29 (6.5) | 0.37 |
| Zapotec languages | 37 (4.5) | 15 (4.0) | 22 (4.9) | 0.31 |
| Mixe | 22 (2.7) | 7 (1.8) | 15 (3.4) | 0.13 |
| Zoque | 17 (2.0) | 6 (1.6) | 11 (2.4) | 0.36 |
| Tlapaneco | 16 (1.9) | 5 (1.3) | 11 (2.4) | 0.18 |
| Tzeltal | 9 (1.1) | 6 (1.6) | 3 (0.6) | 0.15 |
Category including craftsman, loader, driver, cook, shoe shiner, established merchant, blacksmith, retired, waiter, worker, baker, plumber, professional, receptionist, tailor, unknown occupation, taco seller, security guard, and professional, which represent less than 1%; also a category called Other in the SES representing 6.7%.
Nayarit, Morelos, Yucatán, Tlaxcala, unknown, San Luis Potosí, Jalisco, Guanajuato, United States, Campeche, which represent less than 1.0% in total.
Tabasco, Quintana Roo, Nayarit, Morelos, Tlaxcala, San Luis Potosí, Querétaro, United States, Campeche, which represent less than 1% of the total results.
Hidalgo, Veracruz, Tlaxcala, Puebla, Oaxaca, Guerrero, Chiapas, which represent less than 1% of the total results.
Tzotzil, Tzetzal, Tojolabal, Popoluca, Pima, Ixcateco, Huichol, Tarahumara or Raramuri, Purepecha or Tarasco, Paipai, Matlalzinca, Guarijio, Cuicateco, Chontal De Oaxaca, Amuzgo, Aguacateco, Triqui, Tepehua, Huasteco or Teenek, Chol, Ocuilteco, Chinantecan languages, Maya, Yaqui, which represent less than 1%.
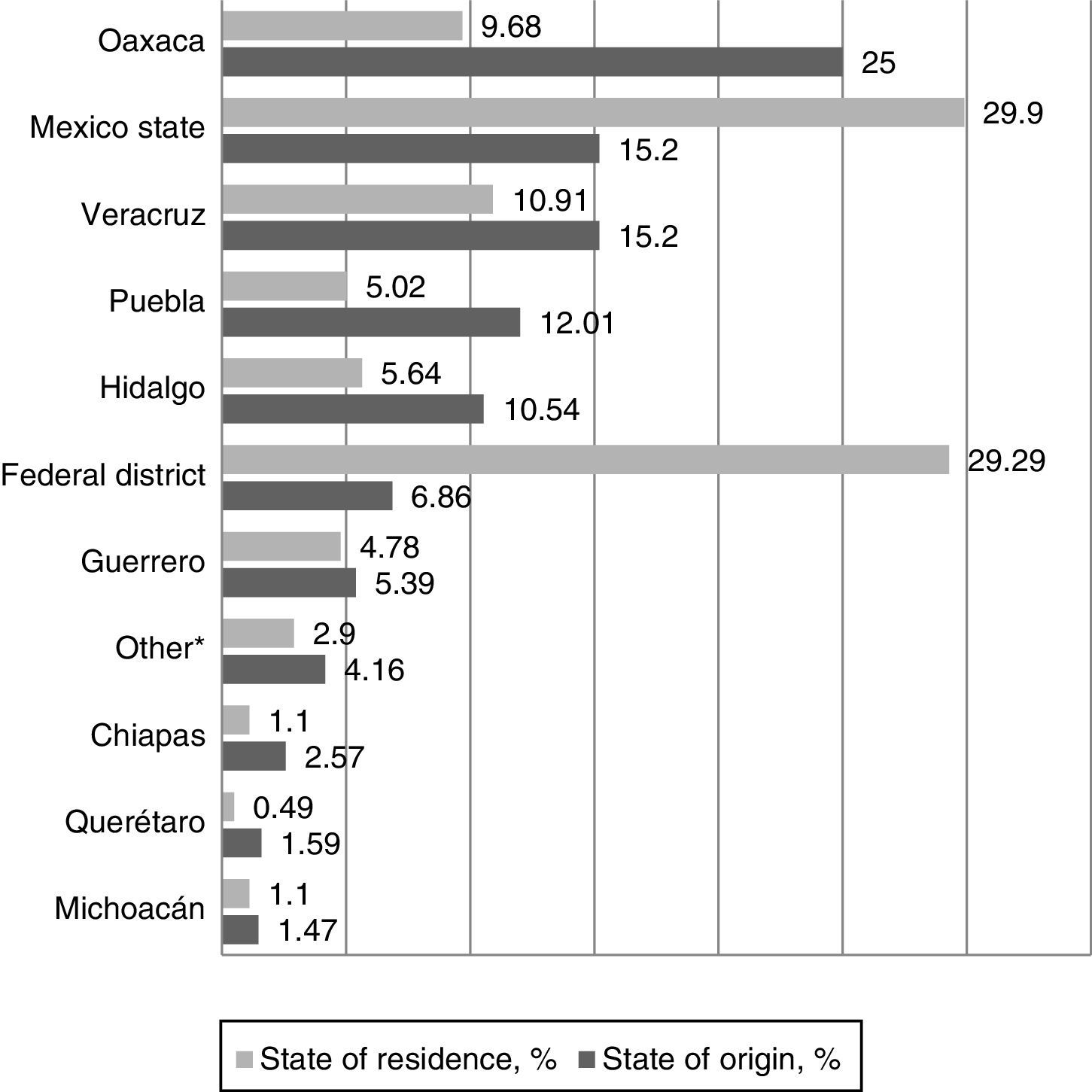
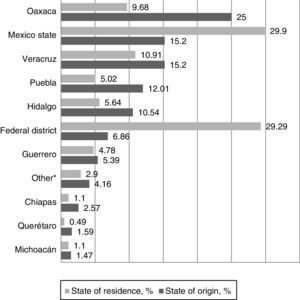
As far as religion is concerned, 687 (84.1%) said they were Catholic, 59 (7.2%) Christian and 28 (3.4%) Evangelist; 17 (2.0%) people said they were not affiliated with any religion or were atheist, 13 (1.5%) people were Jehovah's Witnesses and 12 (1.4%) belonged to other beliefs not specified in the SES. The most common sate of origin was Oaxaca and the state of permanent residence was the State of Mexico; Graph I shows the comparison between these two variables. With regard to residence, 142 (17%) people lived at a temporary residence.
Relationship between state of origin – state of permanent residence of indigenous patients hospitalised in HGM between January 2014 and January 2015. *It refers to the states of Quintana Roo, Tabasco, Campeche, Guanajuato, Jalisco, Nayarit, Morelos, Yucatán, Tlaxcala, San Luis Potosí, United States and the category “unknown”, which represent less than 1% of the population admitted to the hospital.
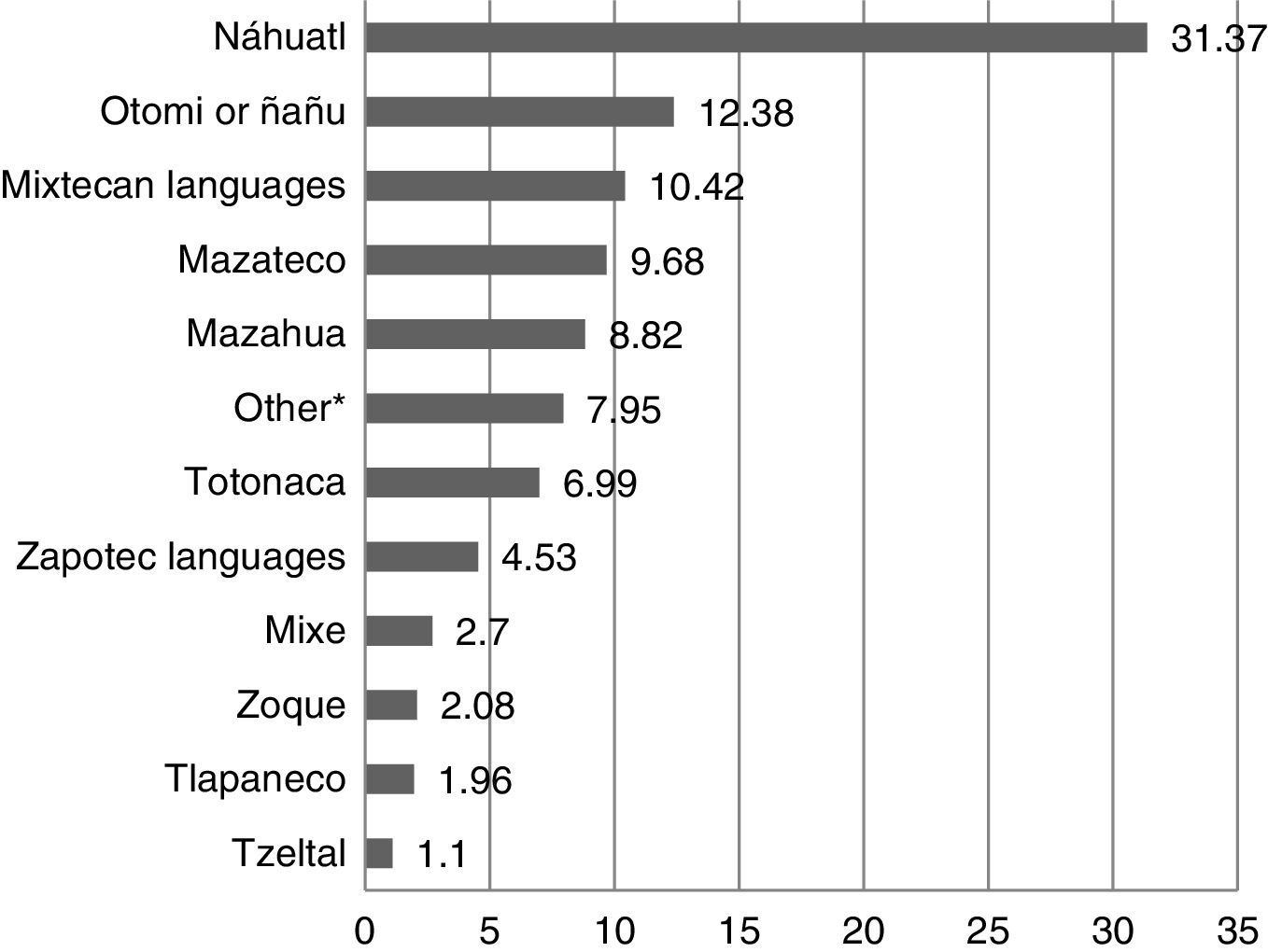
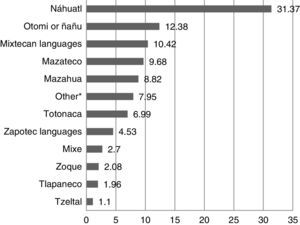
As for the indigenous language, 256 (31.3%) people spoke Náhuatl, 101 (12.3%) Otomi and 85 (10.4%) Mixtec languages; the representation of other indigenous languages of the country can be seen in Graph II.
Percentage of people hospitalised in HGM between January 2014 and January 2015 by the reported indigenous language. *For indigenous languages which represent less than 1% of the total: Aguacateco, Amuzgo, Cuicateco, Guarijio, Huichol, Ixcateco, Matlalzinca, Paipai, Pima, Popoluca, Purepecha or Tarasco, Tarahumara or Raramuri, Tzetzal, Chontal, Tojolabal, Chol, Ocuilteco, Tepehua, Tzotzil, Yaqui, Triqui, Maya, Huasteco and Chinantecan languages.
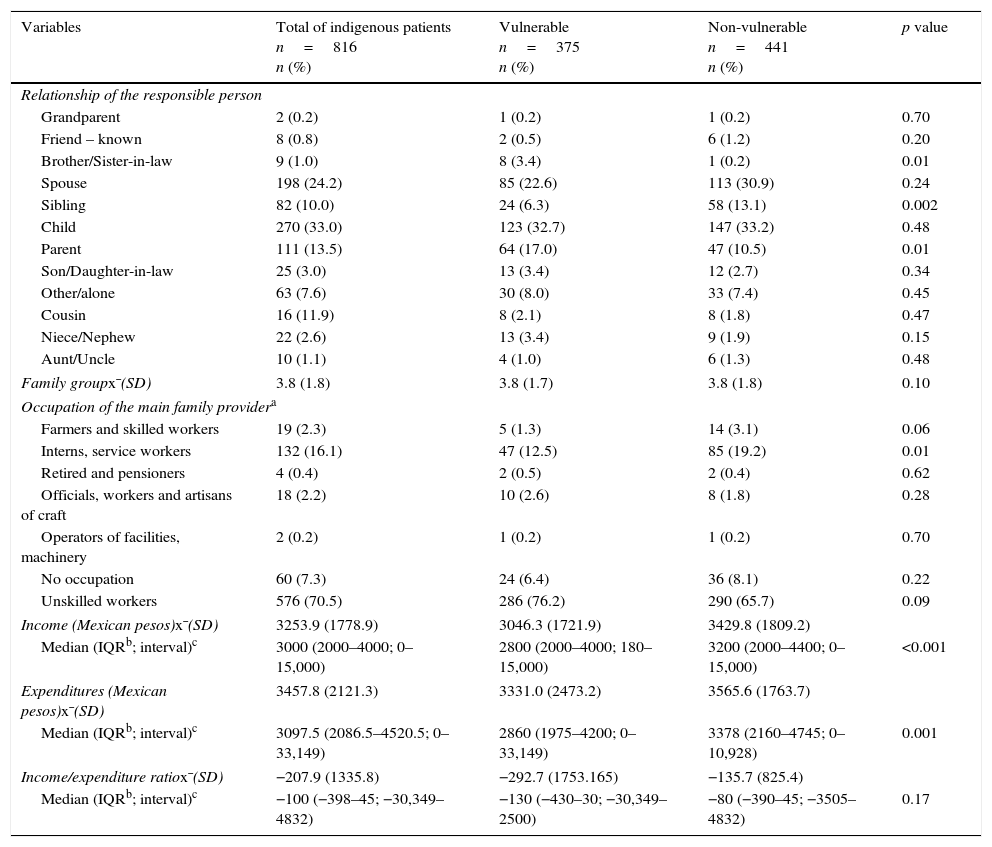
Regarding the family-related variables, 270 (33%) of patients were accompanied by their son or daughter; 198 (4.2%) by their husband or wife; 111 (13.5%) by their mother or father. The family group was made up on average x¯ (SD) of 3.8 (1.8) individuals. From the total, 576 (70.5%) were unskilled workers. The average income x¯ (SD) was 3253.9 (1778.9) Mexican pesos, average expenditure was 3457.8 (2121.3) and the income/expenditure ratio is -207.9 (1335.8).
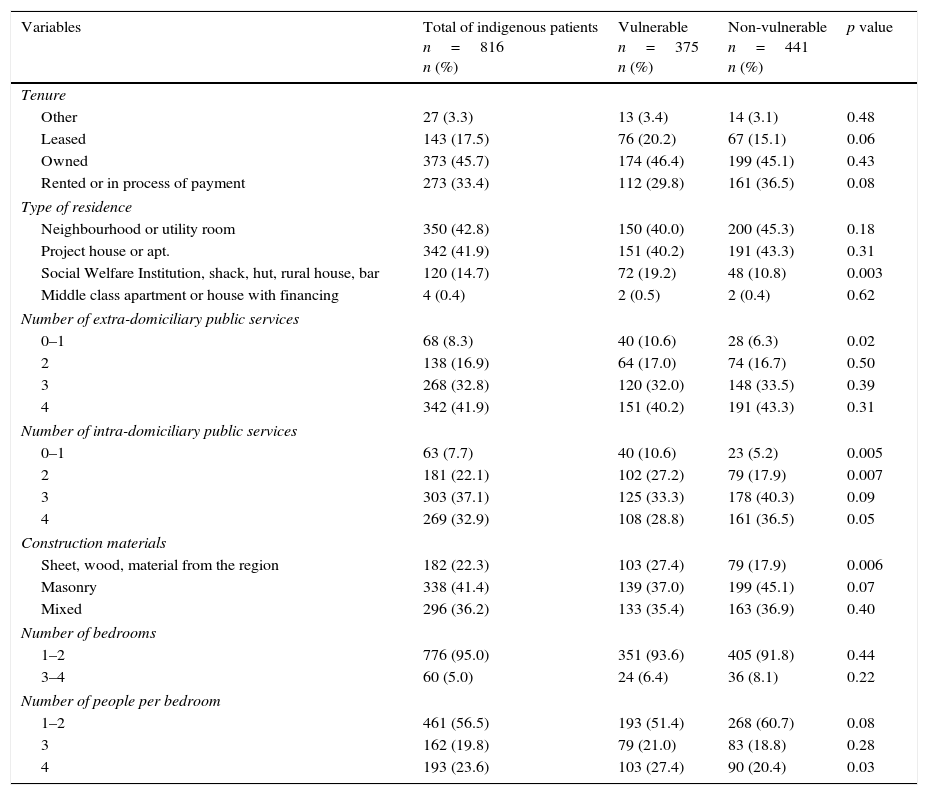
Regarding the housing characteristics, 373 (45.7%) people owned their own home; other forms of tenure and construction conditions are described in Table III.
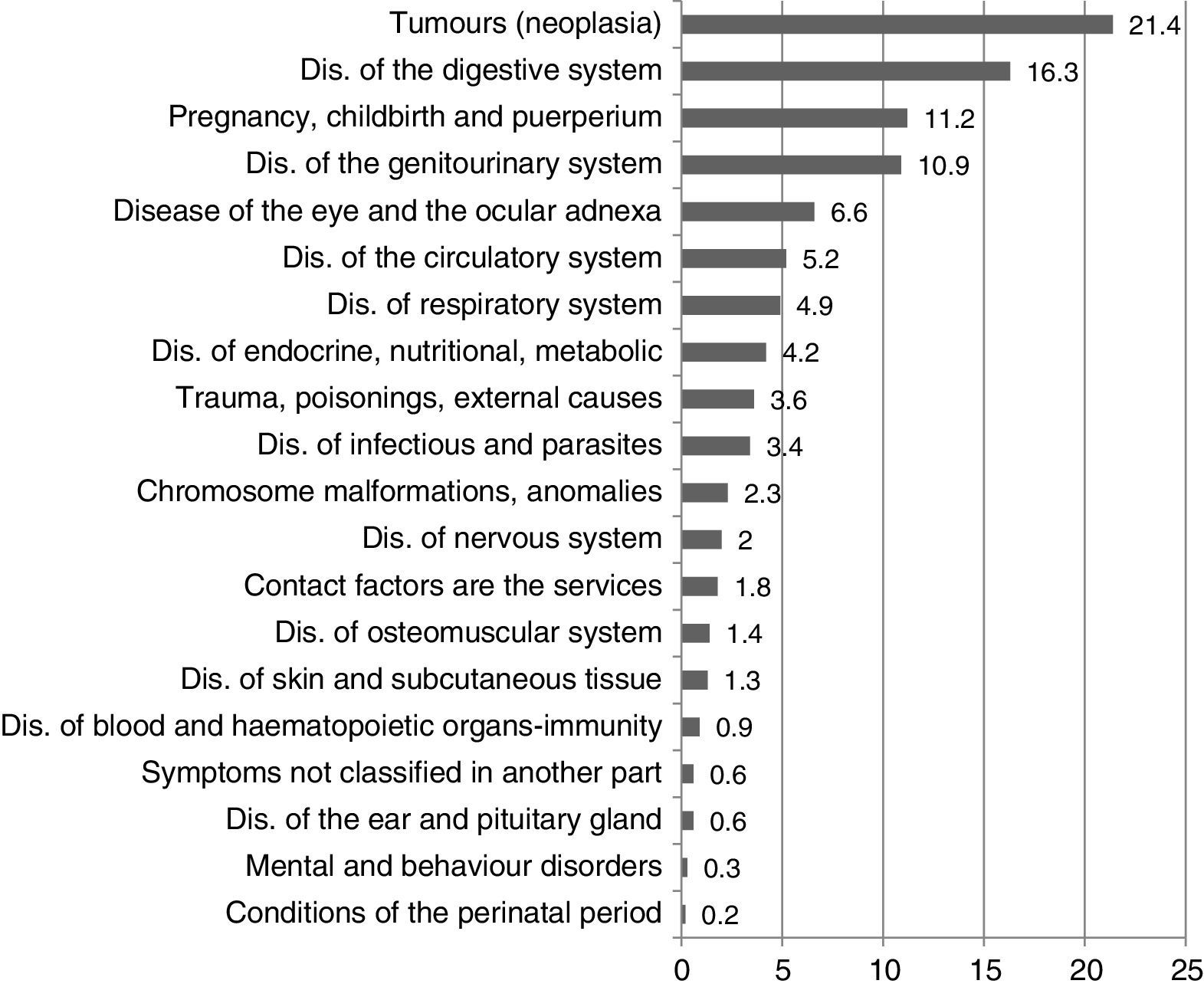
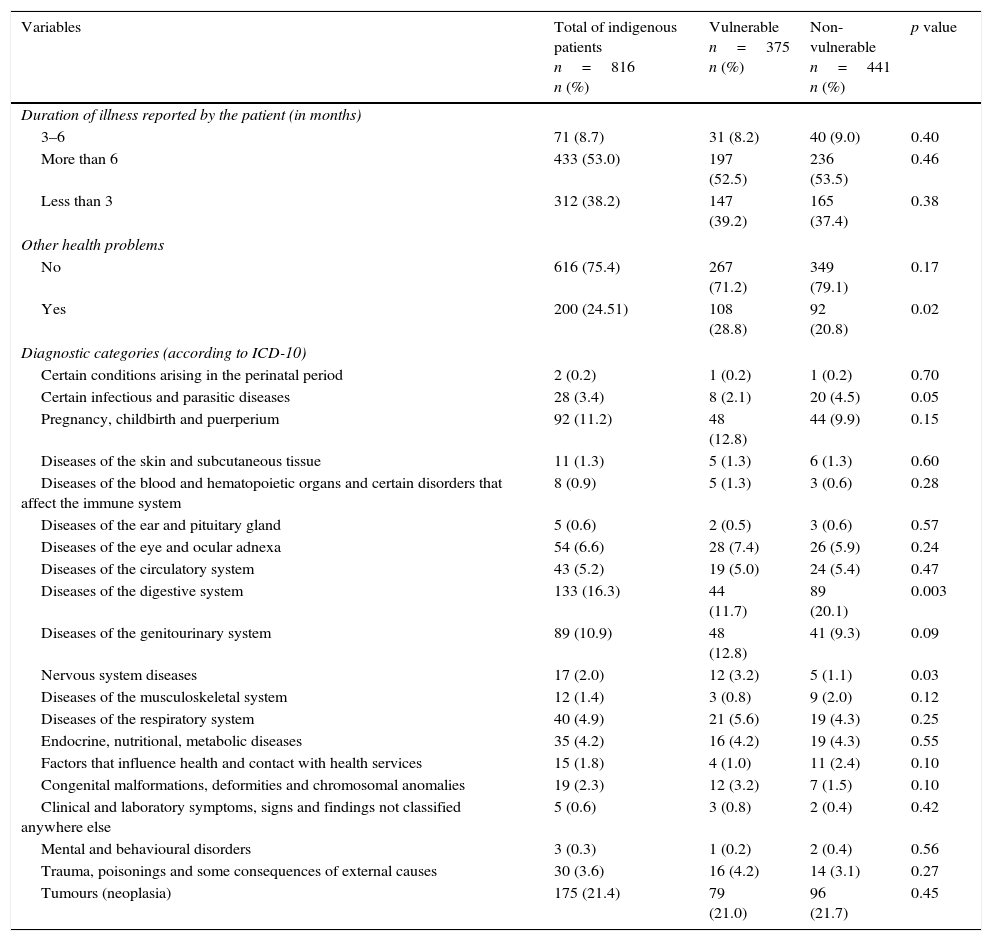
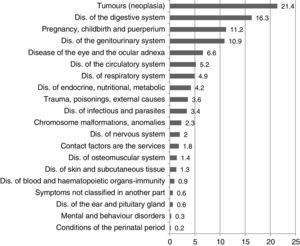
With regard to health-related variables, 312 (38.2%) people reported having the disease concerned for less than 3 months; 71 (8.7%) between 3 and 6 months, and 433 (53.0%) reported suffering from said disease for more than 6 months; 200 (24.5%) subjects reported health issues other than the reason for consultation. The most common diagnostic categories were neoplasms (175 [21.4%]) and digestive system diseases (133 [16.3%]). Other categories are referenced in Graph III.
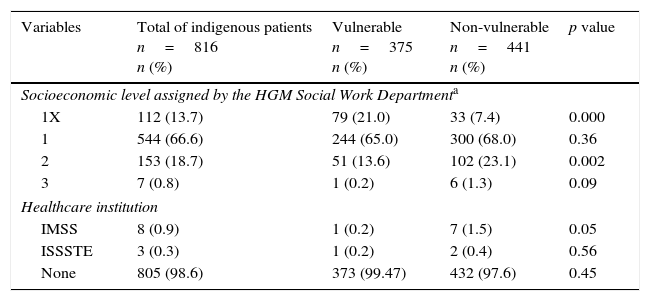
Regarding access to healthcare, 805 (98.6%) people said they were not a member of any healthcare institution; 544 (66.6%) people were classified at socioeconomic level 1; 153 (18.7%) at level 2; 112 (13.7%) were exempt; and 7 (0.8%) were classified at level 3; no person classified as levels 4, 5 or 6. The patients were recognised as vulnerable in 375 (45.9%) of the total.
In the bivariate analysis some significant differences were found between the group classified as vulnerable and those classified as non-vulnerable: in terms of individual variables there were significant differences in the average age (46.6 SD 23.9 vs. 45.8 SD 19; p<0.001), where older indigenous people are classified as vulnerable; furthermore, those who had no education (34.6% vs. 24.9%; p=0.01), did not have a job (20% vs. 13.3%; p=0.02), work in unskilled positions (14.9% vs. 5.6%; p<0.001), those who said they had a permanent residence in Veracruz (13.3% vs. 8.8%; p=0.04) or the place of temporary residence is not known (2.1% vs. 0.4% p=0.03) (Table I).
Regarding the family variables, significant differences were seen when the patient's companion was the brother/sister-in-law (3.4% vs. 0.2%; p=0.01), mother or father (17.0% vs. 10.5%; p=0.01) and those who had lower incomes ($2800 vs. $3200; p< 0.001) were classified as vulnerable (Table II).
Comparison between vulnerable and non-vulnerable indigenous patients hospitalised in HGM between January 2014 and January 2015, taking into account family variables.
| Variables | Total of indigenous patients n=816 n (%) | Vulnerable n=375 n (%) | Non-vulnerable n=441 n (%) | p value |
|---|---|---|---|---|
| Relationship of the responsible person | ||||
| Grandparent | 2 (0.2) | 1 (0.2) | 1 (0.2) | 0.70 |
| Friend – known | 8 (0.8) | 2 (0.5) | 6 (1.2) | 0.20 |
| Brother/Sister-in-law | 9 (1.0) | 8 (3.4) | 1 (0.2) | 0.01 |
| Spouse | 198 (24.2) | 85 (22.6) | 113 (30.9) | 0.24 |
| Sibling | 82 (10.0) | 24 (6.3) | 58 (13.1) | 0.002 |
| Child | 270 (33.0) | 123 (32.7) | 147 (33.2) | 0.48 |
| Parent | 111 (13.5) | 64 (17.0) | 47 (10.5) | 0.01 |
| Son/Daughter-in-law | 25 (3.0) | 13 (3.4) | 12 (2.7) | 0.34 |
| Other/alone | 63 (7.6) | 30 (8.0) | 33 (7.4) | 0.45 |
| Cousin | 16 (11.9) | 8 (2.1) | 8 (1.8) | 0.47 |
| Niece/Nephew | 22 (2.6) | 13 (3.4) | 9 (1.9) | 0.15 |
| Aunt/Uncle | 10 (1.1) | 4 (1.0) | 6 (1.3) | 0.48 |
| Family groupx¯(SD) | 3.8 (1.8) | 3.8 (1.7) | 3.8 (1.8) | 0.10 |
| Occupation of the main family providera | ||||
| Farmers and skilled workers | 19 (2.3) | 5 (1.3) | 14 (3.1) | 0.06 |
| Interns, service workers | 132 (16.1) | 47 (12.5) | 85 (19.2) | 0.01 |
| Retired and pensioners | 4 (0.4) | 2 (0.5) | 2 (0.4) | 0.62 |
| Officials, workers and artisans of craft | 18 (2.2) | 10 (2.6) | 8 (1.8) | 0.28 |
| Operators of facilities, machinery | 2 (0.2) | 1 (0.2) | 1 (0.2) | 0.70 |
| No occupation | 60 (7.3) | 24 (6.4) | 36 (8.1) | 0.22 |
| Unskilled workers | 576 (70.5) | 286 (76.2) | 290 (65.7) | 0.09 |
| Income (Mexican pesos)x¯(SD) | 3253.9 (1778.9) | 3046.3 (1721.9) | 3429.8 (1809.2) | |
| Median (IQRb; interval)c | 3000 (2000–4000; 0–15,000) | 2800 (2000–4000; 180–15,000) | 3200 (2000–4400; 0–15,000) | <0.001 |
| Expenditures (Mexican pesos)x¯(SD) | 3457.8 (2121.3) | 3331.0 (2473.2) | 3565.6 (1763.7) | |
| Median (IQRb; interval)c | 3097.5 (2086.5–4520.5; 0–33,149) | 2860 (1975–4200; 0–33,149) | 3378 (2160–4745; 0–10,928) | 0.001 |
| Income/expenditure ratiox¯(SD) | −207.9 (1335.8) | −292.7 (1753.165) | −135.7 (825.4) | |
| Median (IQRb; interval)c | −100 (−398–45; −30,349–4832) | −130 (−430–30; −30,349–2500) | −80 (−390–45; −3505–4832) | 0.17 |
Within the housing-related variables, significant differences were observed in those classified as vulnerable compared to those classified as non-vulnerable when: participants said that they lived in a “Social Welfare Institution, rural house, shack, hut or cave” (19.2% vs. 10.8%; p=0.003); the amount of extra-domiciliary public services was between 0–1 (10.6% vs. 6.3%; p=0.02); the reported construction material was “sheet, wood or material from the region” (27.4% vs. 17.9%; p=0.006); or when the number of people per bedroom was 4 (27.4% vs. 20.4% p=0.03) (Table III).
Comparison between vulnerable and non-vulnerable indigenous patients hospitalised in HGM between January 2014 and January 2015, taking into account residential and public service variables.
| Variables | Total of indigenous patients n=816 n (%) | Vulnerable n=375 n (%) | Non-vulnerable n=441 n (%) | p value |
|---|---|---|---|---|
| Tenure | ||||
| Other | 27 (3.3) | 13 (3.4) | 14 (3.1) | 0.48 |
| Leased | 143 (17.5) | 76 (20.2) | 67 (15.1) | 0.06 |
| Owned | 373 (45.7) | 174 (46.4) | 199 (45.1) | 0.43 |
| Rented or in process of payment | 273 (33.4) | 112 (29.8) | 161 (36.5) | 0.08 |
| Type of residence | ||||
| Neighbourhood or utility room | 350 (42.8) | 150 (40.0) | 200 (45.3) | 0.18 |
| Project house or apt. | 342 (41.9) | 151 (40.2) | 191 (43.3) | 0.31 |
| Social Welfare Institution, shack, hut, rural house, bar | 120 (14.7) | 72 (19.2) | 48 (10.8) | 0.003 |
| Middle class apartment or house with financing | 4 (0.4) | 2 (0.5) | 2 (0.4) | 0.62 |
| Number of extra-domiciliary public services | ||||
| 0–1 | 68 (8.3) | 40 (10.6) | 28 (6.3) | 0.02 |
| 2 | 138 (16.9) | 64 (17.0) | 74 (16.7) | 0.50 |
| 3 | 268 (32.8) | 120 (32.0) | 148 (33.5) | 0.39 |
| 4 | 342 (41.9) | 151 (40.2) | 191 (43.3) | 0.31 |
| Number of intra-domiciliary public services | ||||
| 0–1 | 63 (7.7) | 40 (10.6) | 23 (5.2) | 0.005 |
| 2 | 181 (22.1) | 102 (27.2) | 79 (17.9) | 0.007 |
| 3 | 303 (37.1) | 125 (33.3) | 178 (40.3) | 0.09 |
| 4 | 269 (32.9) | 108 (28.8) | 161 (36.5) | 0.05 |
| Construction materials | ||||
| Sheet, wood, material from the region | 182 (22.3) | 103 (27.4) | 79 (17.9) | 0.006 |
| Masonry | 338 (41.4) | 139 (37.0) | 199 (45.1) | 0.07 |
| Mixed | 296 (36.2) | 133 (35.4) | 163 (36.9) | 0.40 |
| Number of bedrooms | ||||
| 1–2 | 776 (95.0) | 351 (93.6) | 405 (91.8) | 0.44 |
| 3–4 | 60 (5.0) | 24 (6.4) | 36 (8.1) | 0.22 |
| Number of people per bedroom | ||||
| 1–2 | 461 (56.5) | 193 (51.4) | 268 (60.7) | 0.08 |
| 3 | 162 (19.8) | 79 (21.0) | 83 (18.8) | 0.28 |
| 4 | 193 (23.6) | 103 (27.4) | 90 (20.4) | 0.03 |
Regarding health-related variables, significant differences were seen in relation to vulnerability when the patient said they had other health problems (28.8% vs. 20.8%; p=0.02), and had a diagnosis within the category of nervous system diseases (3.2% vs. 1.1%; p=0.03) (Table IV).
Comparison between vulnerable and non-vulnerable indigenous patients hospitalised in HGM between January 2014 and January 2015, taking into account health-related variables.
| Variables | Total of indigenous patients n=816 n (%) | Vulnerable n=375 n (%) | Non-vulnerable n=441 n (%) | p value |
|---|---|---|---|---|
| Duration of illness reported by the patient (in months) | ||||
| 3–6 | 71 (8.7) | 31 (8.2) | 40 (9.0) | 0.40 |
| More than 6 | 433 (53.0) | 197 (52.5) | 236 (53.5) | 0.46 |
| Less than 3 | 312 (38.2) | 147 (39.2) | 165 (37.4) | 0.38 |
| Other health problems | ||||
| No | 616 (75.4) | 267 (71.2) | 349 (79.1) | 0.17 |
| Yes | 200 (24.51) | 108 (28.8) | 92 (20.8) | 0.02 |
| Diagnostic categories (according to ICD-10) | ||||
| Certain conditions arising in the perinatal period | 2 (0.2) | 1 (0.2) | 1 (0.2) | 0.70 |
| Certain infectious and parasitic diseases | 28 (3.4) | 8 (2.1) | 20 (4.5) | 0.05 |
| Pregnancy, childbirth and puerperium | 92 (11.2) | 48 (12.8) | 44 (9.9) | 0.15 |
| Diseases of the skin and subcutaneous tissue | 11 (1.3) | 5 (1.3) | 6 (1.3) | 0.60 |
| Diseases of the blood and hematopoietic organs and certain disorders that affect the immune system | 8 (0.9) | 5 (1.3) | 3 (0.6) | 0.28 |
| Diseases of the ear and pituitary gland | 5 (0.6) | 2 (0.5) | 3 (0.6) | 0.57 |
| Diseases of the eye and ocular adnexa | 54 (6.6) | 28 (7.4) | 26 (5.9) | 0.24 |
| Diseases of the circulatory system | 43 (5.2) | 19 (5.0) | 24 (5.4) | 0.47 |
| Diseases of the digestive system | 133 (16.3) | 44 (11.7) | 89 (20.1) | 0.003 |
| Diseases of the genitourinary system | 89 (10.9) | 48 (12.8) | 41 (9.3) | 0.09 |
| Nervous system diseases | 17 (2.0) | 12 (3.2) | 5 (1.1) | 0.03 |
| Diseases of the musculoskeletal system | 12 (1.4) | 3 (0.8) | 9 (2.0) | 0.12 |
| Diseases of the respiratory system | 40 (4.9) | 21 (5.6) | 19 (4.3) | 0.25 |
| Endocrine, nutritional, metabolic diseases | 35 (4.2) | 16 (4.2) | 19 (4.3) | 0.55 |
| Factors that influence health and contact with health services | 15 (1.8) | 4 (1.0) | 11 (2.4) | 0.10 |
| Congenital malformations, deformities and chromosomal anomalies | 19 (2.3) | 12 (3.2) | 7 (1.5) | 0.10 |
| Clinical and laboratory symptoms, signs and findings not classified anywhere else | 5 (0.6) | 3 (0.8) | 2 (0.4) | 0.42 |
| Mental and behavioural disorders | 3 (0.3) | 1 (0.2) | 2 (0.4) | 0.56 |
| Trauma, poisonings and some consequences of external causes | 30 (3.6) | 16 (4.2) | 14 (3.1) | 0.27 |
| Tumours (neoplasia) | 175 (21.4) | 79 (21.0) | 96 (21.7) | 0.45 |
Within the hospital care variables, those who were in the socioeconomic exempt level (1X) are more vulnerable (21.0% vs. 7.4% p=0.000) (Table V).
Comparison between vulnerable and non-vulnerable indigenous patients hospitalised in HGM between January 2014 and January 2015, taking into account variables related to the hospital care.
| Variables | Total of indigenous patients n=816 n (%) | Vulnerable n=375 n (%) | Non-vulnerable n=441 n (%) | p value |
|---|---|---|---|---|
| Socioeconomic level assigned by the HGM Social Work Departmenta | ||||
| 1X | 112 (13.7) | 79 (21.0) | 33 (7.4) | 0.000 |
| 1 | 544 (66.6) | 244 (65.0) | 300 (68.0) | 0.36 |
| 2 | 153 (18.7) | 51 (13.6) | 102 (23.1) | 0.002 |
| 3 | 7 (0.8) | 1 (0.2) | 6 (1.3) | 0.09 |
| Healthcare institution | ||||
| IMSS | 8 (0.9) | 1 (0.2) | 7 (1.5) | 0.05 |
| ISSSTE | 3 (0.3) | 1 (0.2) | 2 (0.4) | 0.56 |
| None | 805 (98.6) | 373 (99.47) | 432 (97.6) | 0.45 |
IMSS, Mexican Social Security System; ISSSTE, The Institute of Security and Social Services of State Workers.
This study involves the indigenous population who were admitted to HGM, identified by determining whether or not they speak an indigenous language; the SES did not include the question “Do you speak an indigenous language? If so, which?”, having requested its use for the purposes of this investigation; the SES does not include any further questions about the cultural affiliation of the population. While the percentage of this population is low compared to the total population of hospitalised individuals, it is important to know that this population, recognised as vulnerable from a regulatory perspective,18 do attend HGM.
Most of the indigenous people hospitalised are women. Of the total, 62% (homemakers and unemployed) do not receive income, which could suggest that they experience economic difficulties when it comes to dealing with disease, thus making them more vulnerable.
Most people (77.9%) stated that they were from Oaxaca, the State of Mexico, Veracruz, Puebla and Hidalgo; however, 59.1% were permanent residents in the Federal District and the State of Mexico, which demonstrates the internal immigration of indigenous people in the country; this situation of being both indigenous and migrant26 means high levels of marginalisation and poverty in these communities, which corresponds with the trend of migration in Latin America where 49% of indigenous people now live in urban areas.1 In the group studied the specific reasons for moving to places other than their place of birth are not known.
Seventeen percentage stated living at a temporary residence, apparently to solve their health problem. Information on the migration of the indigenous Mexican population for healthcare reasons is not known, which itself is an issue that requires more attention: first, to know the relationship between the local health system, the population and diseases; and secondly, the social consequences of such migration as people move away, even temporarily, from their context to face a city that does not offer support to indigenous migrants, which could increase their vulnerability and promote rootlessness when eventually this relocation is final.
The main languages identified were Náhuatl and Otomí, which are the same as in the colonial age, showing historic persistence.27
As for the families of these patients, they mainly consisted of 2–4 members; just over 50% of companions were the closest relatives (sons, daughters, husbands and wives). The livelihood of these families came from unskilled jobs, and on average the income for an entire family was very low, maintaining a deficit due to the fact that their expenditure exceeds their income. It may be assumed that the dynamics and roles of the family nucleus will be affected by the onset of the illness of one of the family members, since the mobilisation of not only the patient, but also their companions, costs, causing already low income levels to decrease as it is used to support these members.
Most subjects came to the institution with chronic conditions, especially oncological and digestive diseases, which would indicate disease processes not treated at the primary care level due to the fact that health centres are closed, medicines and supplies are in short supply, they take too long to be treated, and they are far away or there are no resources to care for them.28 Some studies show that the demand for care from this population is linked to infectious diseases29,30; more epidemiological studies with different identification criteria are required in order to compare data in different contexts.
The population studied did not have access to healthcare due to the unskilled work they reported; this would explain the fact that they were seeking treatment at HGM. On the other hand, most (86.2%) were not exempt from payment in the hospital; out-of-pocket spending is unknown, which could be important when the income is very low as it can lead to falling below the poverty line and becoming impoverished due to illness. It is unknown how many of those studied use Seguro Popular (public health insurance), though it is known that this covers 77.9% of the indigenous population of the country,17 having a heterogeneous protective effect on the family economy with few advantages for the poorest subjects or those from rural areas31; it also does not cover all diseases or all costs; all of which would lead us to assume that this population have difficulties in affording healthcare.
The comparative analysis of independent variables (individual, family, housing and public services, health and hospital care) showed some relationship with the vulnerability classification, which we will discuss below.
Older indigenous people, who do not work or have an unskilled job were most likely to be classified as vulnerable. This can potentially be explained by the precarious living conditions in which this subgroup of elderly indigenous people live; this has been described in the literature as a way of life in undignified conditions, which are categorised by poverty, loneliness, disease and marginalisation.32
The lower education and income variables are inter-related within the vulnerable population; this could be interpreted as the fact that their literacy levels compromise their ability to deal with hospital situations. In Latin America it is recognised that illiteracy and dropout rates among indigenous and rural women is higher, affecting their chances of finding a job, and so they are more vulnerable.1 In other words, the level of education influences not only the skills required in the health context but also in the economic possibilities to address problems such as disease, especially among women; although no differences were observed in women for the classification of vulnerability; we believe that there is a co-variable effect that does not allow to establish these differences.
More indigenous people were classified as not vulnerable when they are separated, employed in domestic service, are travelling salesmen and service employees. On the contrary, they are more vulnerable when they reported having permanent residence in Veracruz or their temporary place of residence is not known, although these characteristics were not the most frequent. To analyse these differences, subsequent specific studies are needed.
It is noteworthy that no statistically significant differences were found in terms of religion, state of origin or indigenous language reported, probably due to classification bias.
When the patient's companion was their brother/sister-in-law, mother or father, they were classified as vulnerable and if they were accompanied by their sister or brother they were classified as non-vulnerable; this may be related to the operation of the observed support network with the variable of temporary or permanent residence in the city and is an interesting subject for further analysis.
It is evident that living in a “public institution, rural house, shack, hut or cave”, having fewer than two intra-domiciliary services, if the construction material of the residence is precarious and if there is overcrowding; there are elements that predominate in the classification criteria of social workers to consider a vulnerable person; however, there are a number of people who have these conditions and are not classified as vulnerable; which shows a classification problem.
The complexity of the indigenous situation deserves a deeper analytical approach; for example, in the case of housing, it should be considered that while settling in urban areas can provide better conditions as regards dwelling construction and access to public services, in relation to their rural counterparts, the lag in other issues such as employment, low income or social exclusion and discrimination they may face,1 keeps them in a more vulnerable state compared to non-indigenous people. It may also be the case that the low income of those who move to cities does not allow access to housing with all the infrastructure, keeping them in marginalised area without services and even promoting living on the street.33 Patients classified by the SES as exempt from payment are also categorised as vulnerable, unlike those who obtained payment level 2, who were classified as non-vulnerable, showing that income and payment capacity inside the hospital are related to the variable analysed.
When the patient stated that they had other health problems, they were classified as with vulnerability, which is consistent with higher comorbidity plus an effect on the patients’ daily and financial life.
Suffering from a nervous system disease was associated with vulnerability, unlike having a digestive system disease which was not linked to vulnerability; this is a problem for classification prior to medical examination, since the medical diagnosis is issued after the SES and therefore it cannot be considered a criterion for the vulnerability classification.
When this work was performed some issues related to the study and care of this population in the hospital setting came to light:
- -
The identification of indigenous population in health institutions: The debate on the identification is ongoing and includes the discussion of the definition of indigenous from government, non-governmental and academic institutions, as well as the use of language or self-recognition as variables in identifying them.3,10–12 For the case of HGM, the use of language is the first approach to identification; it does not recognise those who, without speaking it, to self-identify as indigenous, which would be an under-registration. Self-identification is a recognised element in Mexican society from the Constitution until its materialisation in the Census of 2000. If in addition to the language, self-identification is included in local statistics, registration would be optimised and this would allow for differentiating the most disadvantaged segment of the population, which is useful information for the development of social programs12 and making comparative social, clinical or basic analyses, as well as statistical.
- -
Care for indigenous people as a vulnerable population: National and international standards recommend that healthcare policies be drafted that are consistent with local needs and take into account vulnerable groups such as indigenous people.22,29,24,34–36 This study shows that more than half of the indigenous population are not recognised as vulnerable, which would mean that the concepts of indigenous and vulnerability are unclear and/or are not standardised for this hospital setting; it is advisable to comply with this regulation and to take action to protect their rights while they are in the institution.
- -
Utility of the registry of specific information on this population in hospitals: In Mexico, the official information on indigenous health comes mainly from the National Health Survey (ENSANUT),2 last conducted in 2012, which includes the morbidity report made by the same population and that, combined with the sociodemographic information, provides an overview from the point of view of the population. Using hospital sources would complement said reports to go into further detail on the subject; however, it should be remembered that the first step in making records is identification. Currently there are no more basic data to support scientifically-based and culturally appropriate policies.13,37
The indigenous people who come to the city to live or to seek medical care are temporarily or permanently incorporated into a social dynamic that, from various perspectives, is unique and complex. The World Bank (2015)1 emphasises that on the protection of indigenous rights and the development of programs, the authorities turn their attention mainly to traditional rural areas, so little has been done to address indigenous people in cities, making them invisible, preventing culturally sensitive public services from being provided. In the case of the health system in Mexico City and specifically HGM, where they are identified for the first time and there are still no standardised criteria to recognise their social vulnerability and act accordingly, it is necessary to implement actions in favour of this population group, increasing their visibility and mitigating the social gap within the institution.
The descriptive information referenced here shows the unfavourable conditions of the indigenous population who, regardless of their origin or language, have few economic and social resources to withstand a disease. HGM seems to be one of the key institutions for this population, so it is necessary to implement a social program with healthcare equality; and in parallel, it is necessary to train professionals in cultural competence. One proposal could be to meet the “Guidelines to include the identification of indigenous peoples and Afro-descendants in the records of health, of the CEPAL”13 which, with local adaptations, is used for the creation of programs intended for this population.
This report calls for the institutional and academic community to initiate research in medical anthropology and for the recording and analysis of sociodemographic and health information, disaggregated into population groups, and to provide data from the institutions that is reliable and comparable so that this may be used as a strong argument for the implementation of local actions.
Limitations of the studyThe number of indigenous subjects considered in this study are those who were hospitalised at HGM during the one-year period stated. Therefore, it does not represent all patients seen in a year as it excluded those who attended external consultations, since not all those who visit this department are assessed by the Social Work Department.
As this is an observational, cross-sectional and retrospective study, the information is descriptive and specifically reflects the situation of this group of patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo funding was received for this study.
Conflict of interestThe authors declare that they have no conflicts of interest for this study.
Thanks to Dr Rubén Burgos for reviewing the draft report, and to the Systems Department of Hospital General de México “Dr. Eduardo Liceaga” for preparing the databases used in this analysis.