Torpid evolution of diabetic foot ulcers (DFU) is a complex problem of health of patients and causes an increase in costs for the health system. Negative pressure therapy (NPT) is a treatment that accelerates healing by a negative pressure flow applied to the wound to stimulate a series of physiological processes in chronic wounds.
Patients and methodsWe performed a retrospective case series study that evaluated the complications associated to NPT in the treatment of DFU in patients from the Diabetic Foot Unit of the Universidad Complutense de Madrid from 2011 to 2015.
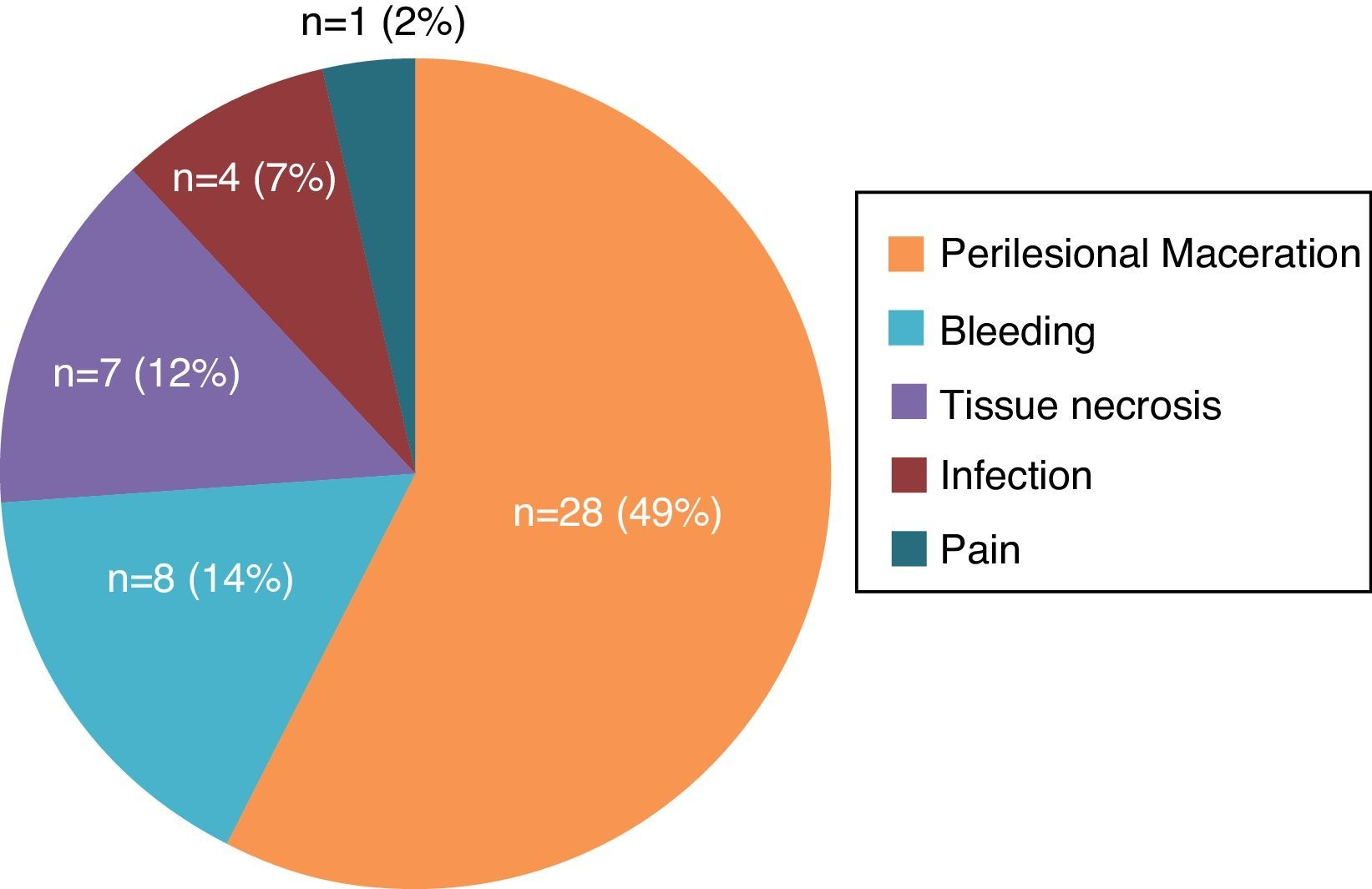
ResultsFifty-seven (83.8%) patients who underwent NPT were analyzed and complications during the time that NPT was maintained were collected. Skin maceration of wound borders was found in 49% of the patients, bleeding (14%), necrosis (12%), local infection (7%) and local pain (2%).
DiscussionThe periwound maceration was the most frequent complication and the most easily resolved. After resolution of the complications, 80% of the patients obtained a favorable result with the therapy, so it can be concluded that NPT is an effective and safe therapy for the treatment of DFU.
El retraso en la cicatrización de las úlceras de pie diabético supone un problema complejo en la salud de los pacientes y provoca un aumento de costes para el sistema sanitario. La terapia de presión negativa (TPN) es un procedimiento terapéutico que acelera la cicatrización, empleando un flujo de presión negativa para estimular una serie de procesos fisiológicos en las heridas crónicas.
Pacientes y métodosSe realizó un estudio observacional retrospectivo en el que se evaluaron las complicaciones asociadas a la TPN en el tratamiento de las úlceras de pie diabético, con pacientes de la Unidad de Pie Diabético de la Universidad Complutense de Madrid, entre los años 2011 y 2015.
ResultadosMediante la revisión de historias clínicas se obtuvo una muestra de 68 pacientes que fueron sometidos a esta terapia, de los cuales 57 (83,8%) presentaron alguna complicación durante el tiempo que mantuvieron la TPN. En el 49%de los pacientes se encontró maceración perilesional, seguida de sangrado (14%), necrosis (12%), infección local (7%) y dolor local (2%).
DiscusiónLa maceración perilesional fue la complicación más frecuente, pero también la que más fácilmente se solventó, mediante la aplicación de apósitos barrera y otras terapias que favorecen el control del exudado de la herida. Tras la resolución de las complicaciones, en el 80% de los pacientes se obtuvo un resultado favorable con la terapia, por lo que se puede concluir que la TPN se considera una terapia efectiva y segura en el tratamiento de las úlceras de pie diabético.
The most common etiologies for DFU are diabetic neuropathy and peripheral arterial disease. Strict ischemic foot is only about 10% of all DFU, being neuropathy involved in 90% of cases. However, in the last years the incidence of neuroischemic ulcers has increased, being actually the most common ulcer types in the diabetic foot.1 The delay of healing of DFU is a complex health problem that affects diabetic patients, increases the costs of health systems and decreases quality of life of patients with DFU.2,3 One of the most evidence based therapies to fasten wound closure is negative pressure therapy (NPT).4–7 It is a noninvasive therapy based on the application of a pressure over the base of the wound with the idea to accelerate healing of wounds of different etiology.2,3,8
NPT consists in the application of sub atmospheric pressure, with a 50–175mm Hg pressure range, in a continuous or intermittent fashion and with or without the instillation of a drug over the complex wound.9,10 NPT improves wound conditions and creates a good environment for healing activating the mechanisms of normal healing: granulation tissue proliferation, increased local hyperemia, reduction of edema, bacterial load and exudate, control of metaloprotease levels, and healing of wound in a wet environment.2,3,8,9
Main indications for this therapy are: chronic wounds, acute and traumatic wounds, dehiscence, flaps and grafts.2,3,9,10 Contraindications are: soft tissue infections, osteomyelitis, necrotic tissue, malignancy and non-explored fistula.9–11
Although in the scientific literature there are several studies about the effectiveness of NPT12, very few of them explain the complications associated with this therapy that are mainly derived from its use in non indicated cases. Commonly described adverse effects are usually minor and include pain during dressing changes, tissue necrosis, perilesional tissue erosion and periwound maceration.13–15 Major adverse effects can also occur such us allergic reactions, infection, sepsis or osteomyelitis that require immediate discontinuation of the therapy.16–18
The objective of the present study is to describe the most common complications observed with the application of NPT in patients with DFU.
Patients and methodsA retrospective case series study was performed in patients with DFU treated with NPT in the Diabetic Foot Unit of Universidad Complutense de Madrid, between January 2011 and November 2015.
Inclusion criteria included patients, independently of their gender, older than 18 years with a DFU that after surgical debridement required treatment with NPT. Patients with some contraindications for the application of NPT previously reported were excluded. In accordance with Spanish law of patients security and data protection all information was securely and anonymously treated.
All patients underwent surgical debridement of their FDU, removing nonviable devitalized tissue and afterward NPT was applied with a polyurethane sponge in the ulcer with a pressure of 125mm Hg and a mean time of 7–10 days.2,3,8 The device employed was VivanoTec®, with a Vivano®Med portray (Hartmman, Germany). Employed devices for the therapy did not include an instillation drug or antiseptic drugs in the wound base. All patients were instructed to maintain absolute rest, to do not change the dressing of the device and to put in contact with the center in case of any problem.
Ulcers were classified by its etiology into neuropathic, ischemic or neuroischemic based on the clinical exploration of the patients. A neuropathic ulcer was considered when the patient showed decreased sensitivity thresholds, tested with Semmes–Wenstein 5.07–10g monofilament and Horwell biotensiometry.19 Alteration of superficial sensitivity was considered when the patient did not detect 4 or more points in the monofilament examination of the plantar foot and alteration of vibratory sensitivity was considered when patient was unable to detect vibration under a 25mV threshold with the biotensiometry. Ischemic ulcer was considered when the patient showed signs of peripheral arterial disease such us absence of tibialis posterior of tibialis anterior pulse, ankle-brachial index (ABI) less than 0.9 and toe pressure less than 55mm Hg with an ABI of less than 0.7.20
Registration of the following complications were noted: periwound maceration which basically consisted of softening and decomposition of periwound tissues,8 pain referred by the patient during dressing changes, bleeding that produced obstruction of therapy avoiding negative pressure,11 tissue necrosis seen as necrosis as a consequence of the NPT11 and infection, when 2 or more signs of local infection or systemic signs defined by the Infectious Diseases Society of America (IDSA) was present.12
Complications were classified as minor (easy resolution) and major (therapy discontinuation). Periwound maceration, bleeding and pain with dressing changes were considered minor complications. Major complications were considered when discontinuation of the therapy and a new treatment had to be started because of that complication, basically tissue necrosis and infection.
Therapy was considered successful when the main objective of NPT application was achieved. The main objective was bone tissue coverage with granulation tissue even when full epitelization was not achieved and other local therapies needed to be established.
Statistical analysis was performed with SPSS program for Windows, 21.0 version (SPSS, Inc. Chicago, IL). Qualitative variables were presented as frequencies and percentages and quantitative variables as mean and standard deviation. Chi squared test was performed for qualitative variables of ulcer type and complication of therapy. For calculation strength of association between the variables an Odds Ratio was calculated, considering the 0.05 value as the limit for null hypothesis rejection.
ResultsA total of 57 patients were finally selected, of whom 48 showed some kind of complication during the application of the NPT. Mean age of patients was 59.86±12.95 years. Gender was 80.70% men and 19.30% women. Seven cases (12.28%) had type I diabetes mellitus and 50 cases (87.72%) had type II, with a mean time of 15.79±12 years of evolution of the disease. Neuropathic ulcers were present in 21 cases (36.8%), 3 cases (5.3%) had ischemic ulcers and 33 cases (57.9%) had neuroischemic ulcers.
Mean application time of NPT was 10.42±4.78 days. Observed complications were the following (Fig. 1): perilesional wound maceration in 28 patients (49%), bleeding in 8 patients (14%), pain with dressing change in 1 patient (2%), tissue necrosis in 7 patients (12%) and local infection of the ulcer in 4 patients (7%). Periwound maceration, bleeding and pain were considered minor complications (65%) and tissue necrosis and infection were considered major complications (19%). Of the 48 patients that suffer complications, tissue necrosis, pain and local infection were a cause of treatment cessation before scheduled time, comprising 11 patients (21%). The 37 cases with minor complications were easily resolved without the need to stop the treatment.
Of the 57 patients studied, only 9 (16%) of them did not developed any complication. Most common complication was periwound maceration that was present in almost half of cases. In most cases, it was not find association (p>0.05) between any of the complications observed and the etiology of the ulcers. However, it was observed an association between the presence of ischemic ulcers and the development of pain during its application (p<0.05; OR 0.94 (IC 0.88–1)).
Effectiveness of the therapy was achieved in 86% of patients (n=49). In 8 patients (14%) the therapy was not successful. In three of them 3 (21%) patients suffered minor complications and 5 (62%) had major complications. Association was also found between minor complication and success of NPT (p<0.01; OR 0.53(IC 0.9–0.3)).
DiscussionIn the present study, the most common complication was periwound maceration (49%), being at the same time a minor complication easy to resolve. Jiménez et al.18 observed in their study with 87 patients, that the most common complication was also perilesional wound dehiscence, followed by erosion of perilesional tissue and pain with dressing changes. Also, Mouës et al.17 found that periwound maceration was the most common minor complication with tissue erosion. Indeed, a recent study found that the presence of periwound maceration in 6 of the 53 cases studied (11.32%), pointing its easy resolution with the use of barriers dressings.21
It is also our opinion that the cause of this complication is not derived from the therapy itself, but from the occlusive film that is applied over the wound or the sponge introduced inside the ulcer the oversize the borders of the wound or it does not absorb all the exudate from the wound. To avoid this complication, we have found that it is necessary to use an adequate device to offload the DFU together with barrier dressings to limit the damage of the skin borders of the wound.
Presence of pain was a very uncommon complication and it was associated it ischemic type etiology of the ulcer. It can be considered that the negative pressure made with the therapy and the suction effect of the exudate can provoke pain in sensitivity normal patients. In these patients it would be interesting to drop the pressure of mm of Hg at which therapy is applied or perhaps to make the therapy in an intermittent way. Vuerstaek et al. and McCallon et al.15,16 found pain during dressing change as one of the most common complications and Jiménez et al.18 indicates the same finding recommending the use of analgesics and instillation of local anesthetics in the wound to avoid this complication.
In general terms, NPT was successful in 45 patients (9 of them without complications and 36 of them with minor complications easily resolved). Of all cases, 79% of them achieved tissue granulation tissue and exudate control even with the presence of minor complications. Several studies in the literature consider NPT as an effective and safe treatment for the treatment of DFU4,5,13 reducing healing times compared to conventional treatments. Mechanisms of action of NPT favors a good environment for ulcer healing reducing the edema, controlling the exudate and stimulating the angiogenesis and the formation of granulation tissue.
Complications or major adverse effects associated with NPT are mainly produced in cases in which indications were not right. It is necessary to know perfectly contraindications of this treatment described in the literature10,14 and carefully evaluate if the etiology of the ulcer would benefit from this therapy. At the same time, minor complications can be viewed as subtlest adverse effects with easy resolution.
In conclusion, NPT is an effective and safe therapy with optimal results for the management of DFU. NPT seems to be beneficial for the management of DFU with different etiologies and with a high percentage of success and minor complications easily resolved. The most common complication associated with NPT was periwound maceration and most of the adverse effects were minor and could be easily resolved and they do not interfere with the evolution of the ulcers if they are well managed.
We thank Clínica Universitaria de Podología of UCM for its collaboration in this study and Raúl Molines Barroso for his help in the statistical analysis of data.