The years of residency are the pillars of the subsequent practice in every medical specialty. The aim of our study is to evaluate the current situation, degree of involvement, main interests, and perceived quality of the training received by Spanish residents of neurology, specifically in the area of headache.
MethodsA self-administered survey was designed by the Headache Study Group of the Spanish Society of Neurology (GECSEN) and was sent via e-mail to all residents who were members of the Society as of May 2015.
ResultsFifty-three residents completed the survey (n=426, 12.4%): 6% were first year residents, 25.5% second year, 23.5% third year, and 45% fourth year residents, all from 13 different Spanish autonomous communities. The areas of greatest interest are, in this order: Vascular neurology, headache, and epilepsy. Of them, 85% believe that the area of headache is undervalued. More than half of residents (52.8%) do not rotate in specific Headache Units and only 35.8% complete their training dominating anaesthetic block and toxin infiltration techniques. Of them, 81.1% believe that research is scarce or absent; 69.8% have never made a poster/presentation, 79.3% have not published and only 15% collaborate on research projects in this area. Lastly, 40% believe that they have not received adequate training.
ConclusionsHeadache is among the areas that interest our residents the most; however, we believe that we must improve their training both at a patient healthcare level and as researchers. Thus, increasing the number of available courses, creating educational web pages, involving residents in research, and making a rotation in a specialised unit mandatory are among the fundamental objectives of the GECSEN.
Los años de residencia son la base fundamental para el ejercicio posterior de cualquier especialidad médica. El objetivo de nuestro estudio es evaluar la situación actual, grado de implicación y calidad percibida en la formación como neurólogos de los residentes, específicamente en el área de cefaleas.
MétodosDesde el Grupo de Estudio de Cefaleas de la Sociedad Española de Neurología (GECSEN) se diseñó una encuesta autoadministrada que fue enviada vía e-mail a todos socios los residentes de Neurología (mayo de 2015).
ResultadosCompletaron la encuesta 53 residentes (53/426: 12,4%; R1: 6%; R2: 25,5%; R3: 23,5% y R4: 45% de 13 comunidades autónomas). Las áreas que más les interesan son por orden: vascular, cefalea y epilepsia. El 85% considera que el área de cefalea está infravalorada. Más de la mitad (52,8%) no rotan en consultas específicas de cefaleas y solo el 35,8% terminan su formación con dominio de la técnica de bloqueos anestésicos e infiltración de toxina. El 81,1% considera que la investigación es escasa o nula. El 69,8% nunca ha realizado un póster/comunicación, el 79,3% no ha publicado y solo un 15% colabora en proyectos de investigación en esta área. El 40% considera que no ha recibido una formación adecuada.
ConclusionesLa cefalea está entre las enfermedades que más interesan a nuestros residentes, sin embargo, consideramos que hay que mejorar su formación tanto en el ámbito asistencial como investigador, así como la visión que tienen de ella. Aumentar los cursos, crear páginas web formativas, involucrarles en investigación y considerar obligatoria la rotación en una unidad especializada son algunos de los objetivos fundamentales que planteamos desde el GECSEN.
Residency is a fundamental step on the path to becoming a neurologist, which is why we must be sure that residents receive the best possible training. However, there has not to date been any specific evaluation of the training provided in the area of headache from the viewpoint of residents. The vertiginous advances seen in the various areas of neurology have brought about a parallel increase in subspecialisation.1 The area of headache is no exception to this trend. This has resulted in a greater challenge for neurologists and an ever-greater need for them to be more specialised and capable of managing patients with more complex diagnoses or who do not respond to conventional treatment. Neurologists must have sufficient training and expertise to indicate and perform the new therapeutic alternatives to traditional oral treatment (anaesthetic blocks, botulinum toxin infiltration, etc.). They must also be able to work directly with colleagues from such other departments as pain units and neurosurgery and psychiatry departments in order to manage headache and frequently associated conditions from a holistic, multidisciplinary approach. Headache is a highly prevalent, incapacitating disease2; the constant publication of new epidemiological, pathophysiological, and therapeutic discoveries makes it a highly fertile area for medical residents. Nonetheless, in such countries as the United States, there is a remarkably low number of headache specialists in comparison to demand. This may be due to the fact that physicians there must undergo one year of training and pass an examination in order to be accredited as headache specialists (19 states have 2 or fewer headache specialists).3 This frequently results in misdiagnosis, as has been shown by the CIEN-mig study in Spain, which found a diagnostic delay of 28.7 months for chronic migraine.4 This is just one example of the need for continued improvement of training in the area of headache, from the very earliest stages.
The official training programme for neurology in Spain (published in the Official State Gazette) establishes the requirement that physicians have the ability to comprehensively assess neurological patients, strengthen their technical skills in the area of neurology, and foster research within each subspecialty.5 However, headache training is currently unavailable in both mandatory and elective rotations in neurology residency programmes, as there is no rotation at specialised headache units or clinics. The programme does, however, specify that residents must have a practical and theoretical understanding of the field at the time they complete their training. In order for residents to be competent in these techniques, they must receive the necessary tools during their training period.6
Therefore, this study aims to assess the appropriateness of the training that residents receive, specifically in the area of headache, as well as the current situation of this training, the level of involvement, and perceived quality.
Material and methodsThe Executive Board of the Spanish Society of Neurology's (SEN) Headache Study Group (GECSEN) designed a self-administered questionnaire, which was sent to all residents belonging to the SEN as of May 2015 through the corporate email of the SEN's scientific division. A follow-up email was sent halfway through the survey period.
Participants remained anonymous at all times.
The survey comprised 15 items: year of residency, autonomous community, area of greatest interest (multiple choice), reason for interest in headache (multiple choice), whether they believed the field of headache to be undervalued, whether their training hospital had a specialised headache clinic, whether their training involved a specific rotation in a headache unit or clinic, their level of interest in research, participation in research projects, poster presentations, oral communications, or publications, their evaluations of the training received, training in procedures (botulinum toxin infiltration, anaesthetic blocks), and areas for improvement.
ResultsThe questionnaire was sent to 426 neurology residents, of whom 285 opened the email and 53 (12.4%) completed the survey. In terms of year of residency, there were 3 respondents (6%) in the first year of residency (R1), 14 (26.4%) in the second year (R2), 12 (22.6%) in the third year (R3), and 24 (45%) in the fourth year (R4).
Survey respondents were from 13 autonomous communities: 5 from Andalusia (9.4%), 4 from Aragon (7.5%), 2 from Asturias (3.8%), 6 from the Canary Islands (11.3%), 4 from Catalonia (7.5%), 3 from Castile-León (5.7%), 2 from Castile-La Mancha (3.8%), 14 from the region of Madrid (26.4%), 6 from the region of Valencia (11.3%), 1 from Galicia (1.9%), 1 from La Rioja (1.9%), 1 from Navarre (1.9%), and 2 from the Basque Country (3.8%); 2 respondents (3.8%) did not answer this question.
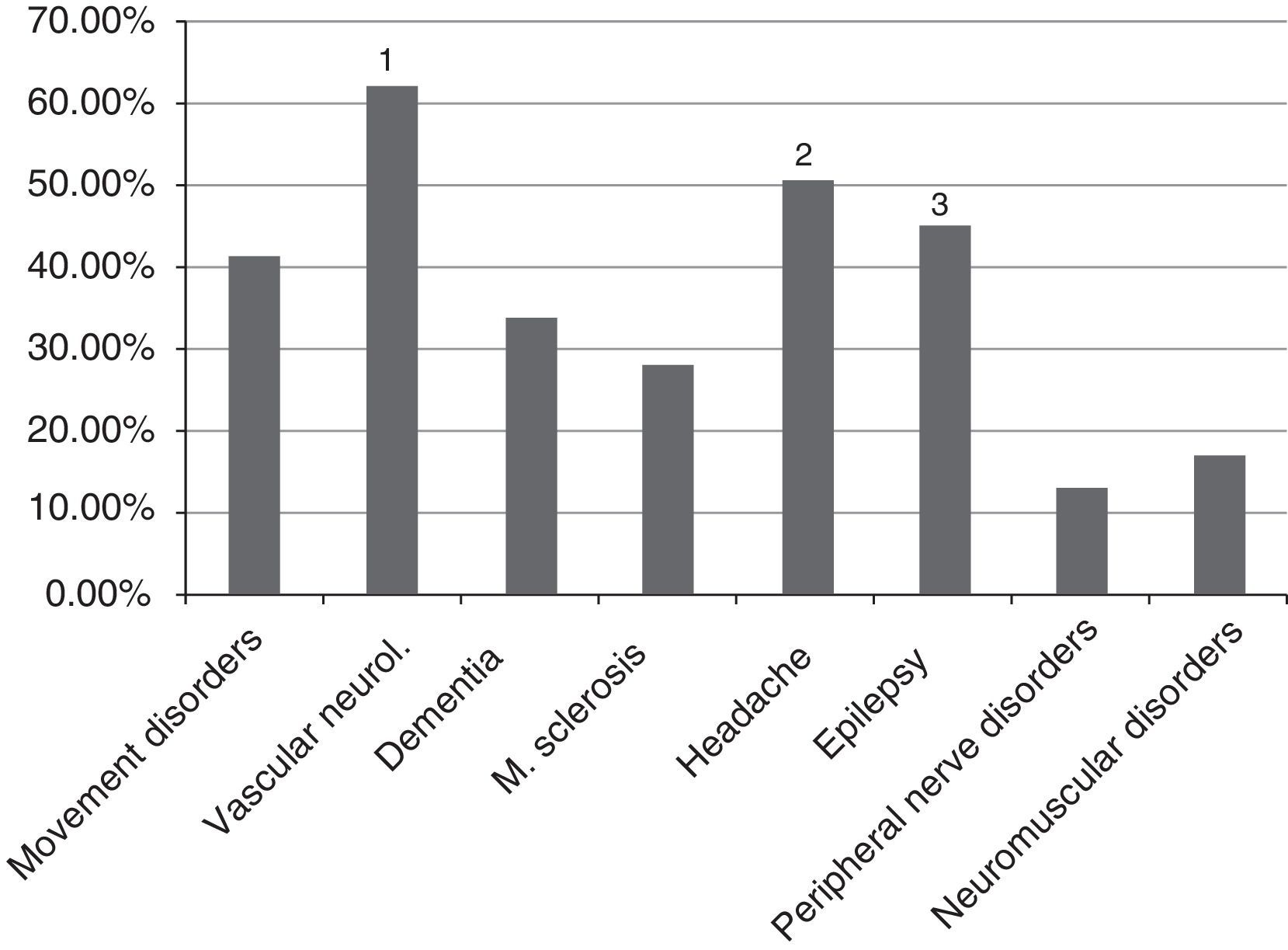
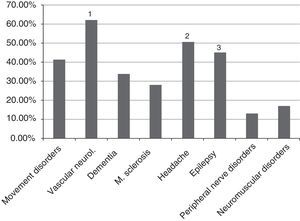
The areas of greatest interest among participants were vascular neurology, headache, and epilepsy, which were chosen by 32 (60.4%), 26 (49%), and 23 residents (43.4%), respectively (Fig. 1). We also analysed the area of greatest interest by residency year. Movement disorders were the most popular area of specialisation in R1; of only 3 residents in the group, 2 (66.7%) chose this subspecialty. In the other 3 years, vascular neurology was the most popular subpecialty, with the second most frequent choice being headache in R4 and epilepsy in R3 and R2, with the same number of votes.
The main reasons for interest in headache were: prevalence (58.5%), diagnosis (41.5%), treatment (41.5%), research (15%), and other reasons (9.43%). Forty-five residents (85%) believed that the field of headache was undervalued.
According to fundamental area (care, training, and research into headache), the results are as follows:
- -
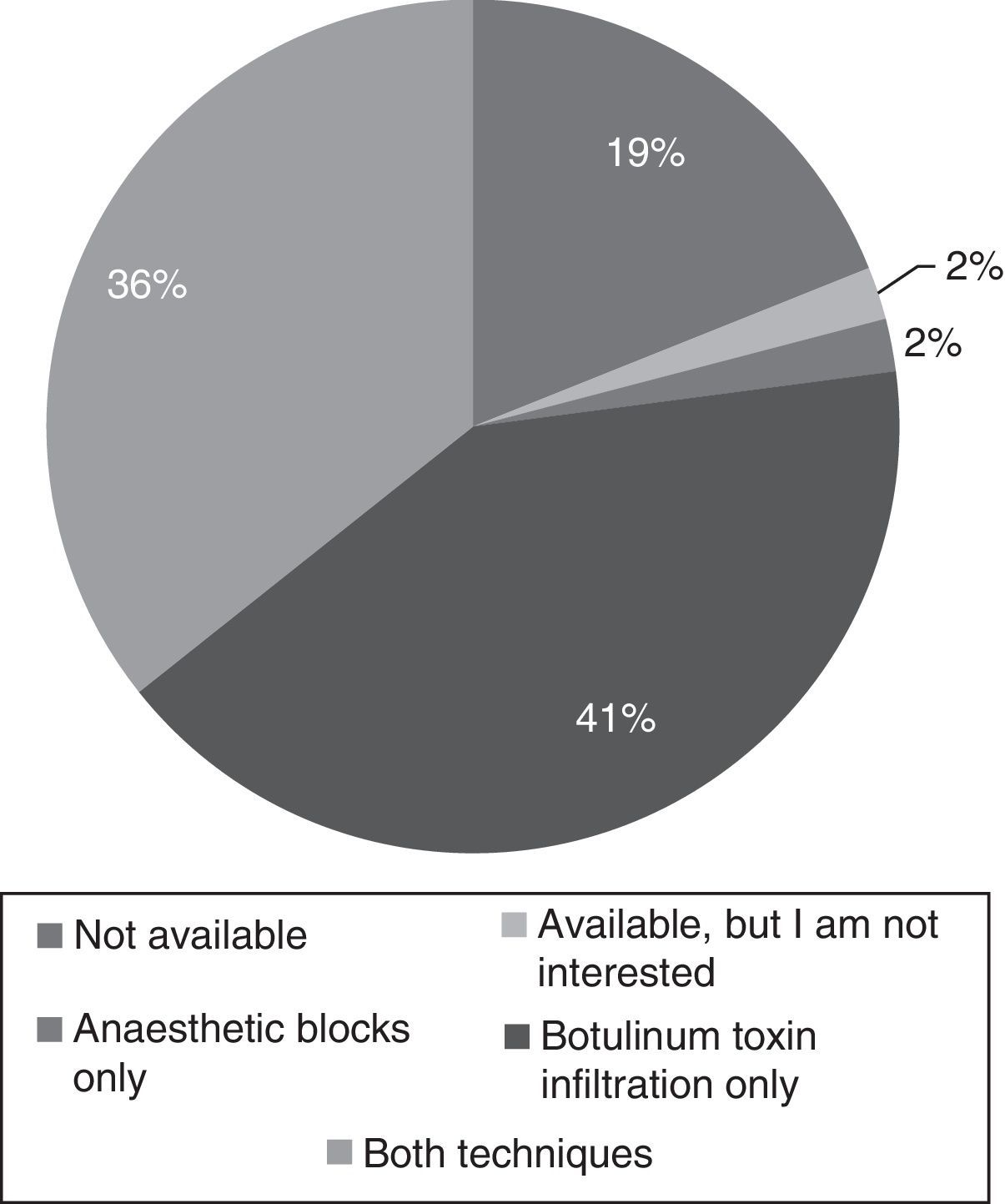
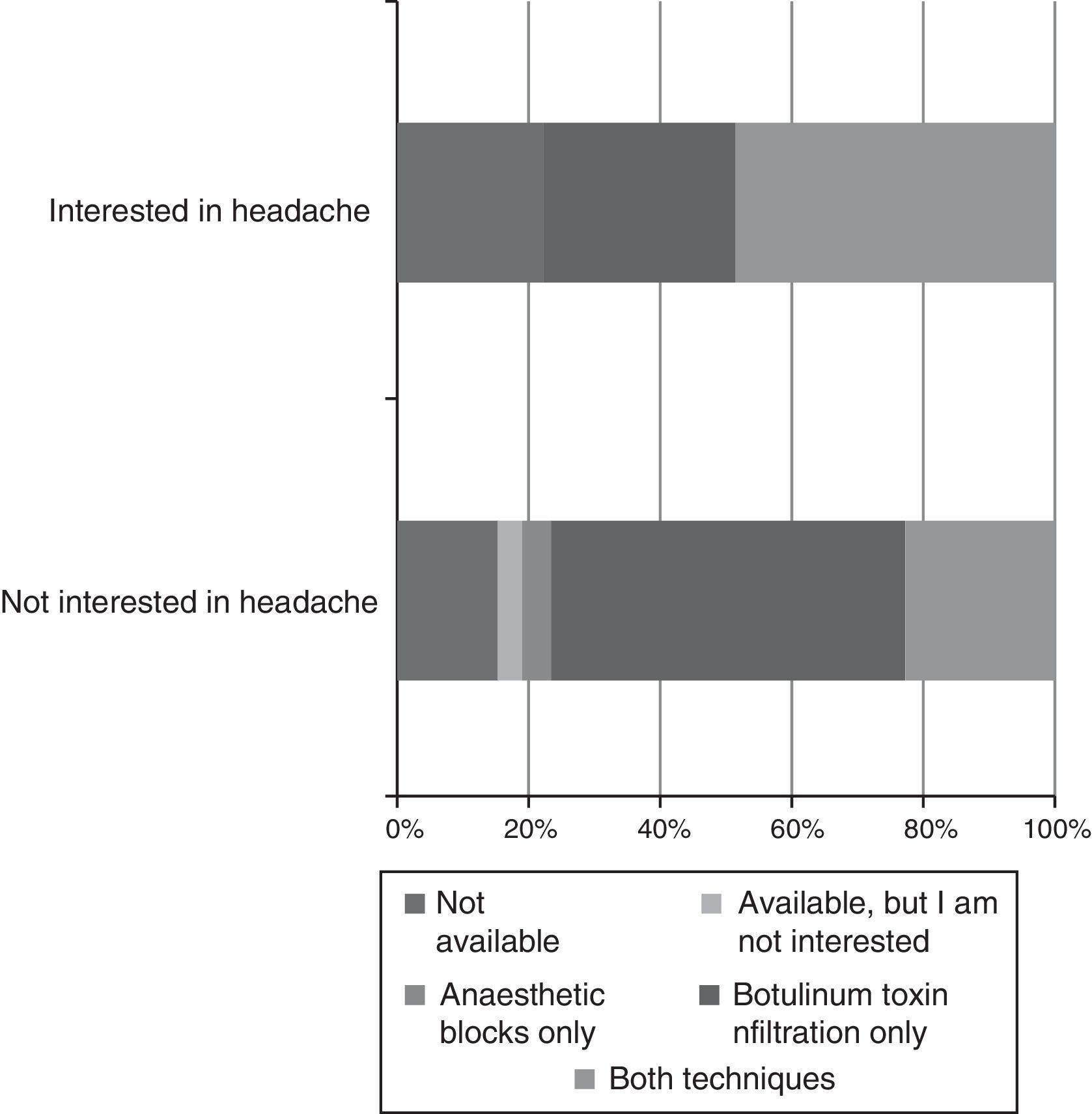
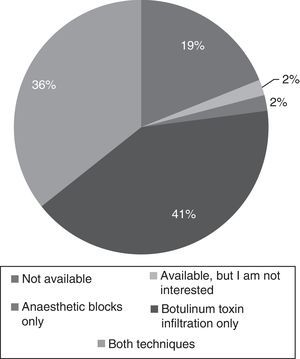
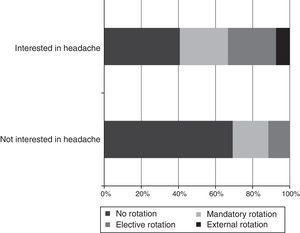
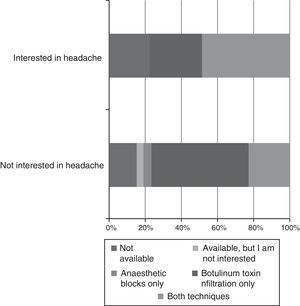
Care: 59% of residents were training at hospitals which had specialised headache units or clinics. However, 53% of respondents did not have specific rotations in these units and clinics. Rotations were elective in 21% of cases, and mandatory in 22%; a headache unit/clinic was chosen as an external rotation by only 4% of residents. Regarding the training in administering infiltrations, 10 residents (19%) had no training, one resident (1.9%) was not interested, one resident (1.9%) had been trained only in performing anaesthetic blocks, 22 (41.5%) had been trained only in the protocol for botulinum toxin infiltration, and only 19 (35.8%) were fully competent in both techniques at the end of the training period (Fig. 2).
- -
Training: 40% of respondents believed that their training in the field of headache was not adequate. The remaining residents believed that their training had mainly consisted in courses (5 residents, 9.4%), self-teaching (12, 22.6%), and training received at the hospital (15, 28.3%). In terms of improving the training provided, 25 residents (47.2%) suggested rotations in headache units or clinics being made mandatory; 37 (69.8%) suggested residents should attend more training courses; 29 (59.7%) suggested updating and improving the study group's webpage; and 24 (45.3%) suggested promoting research.
- -
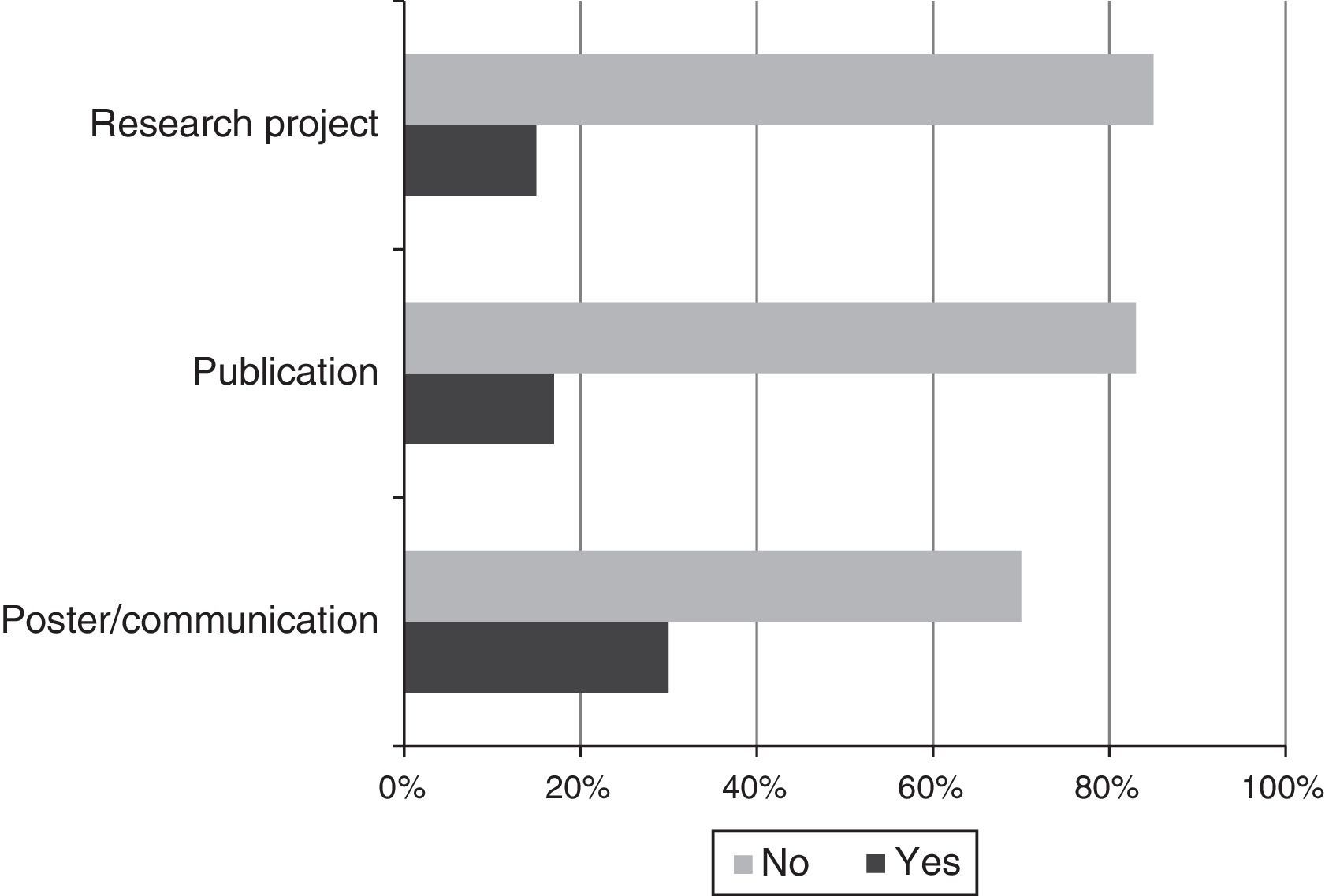
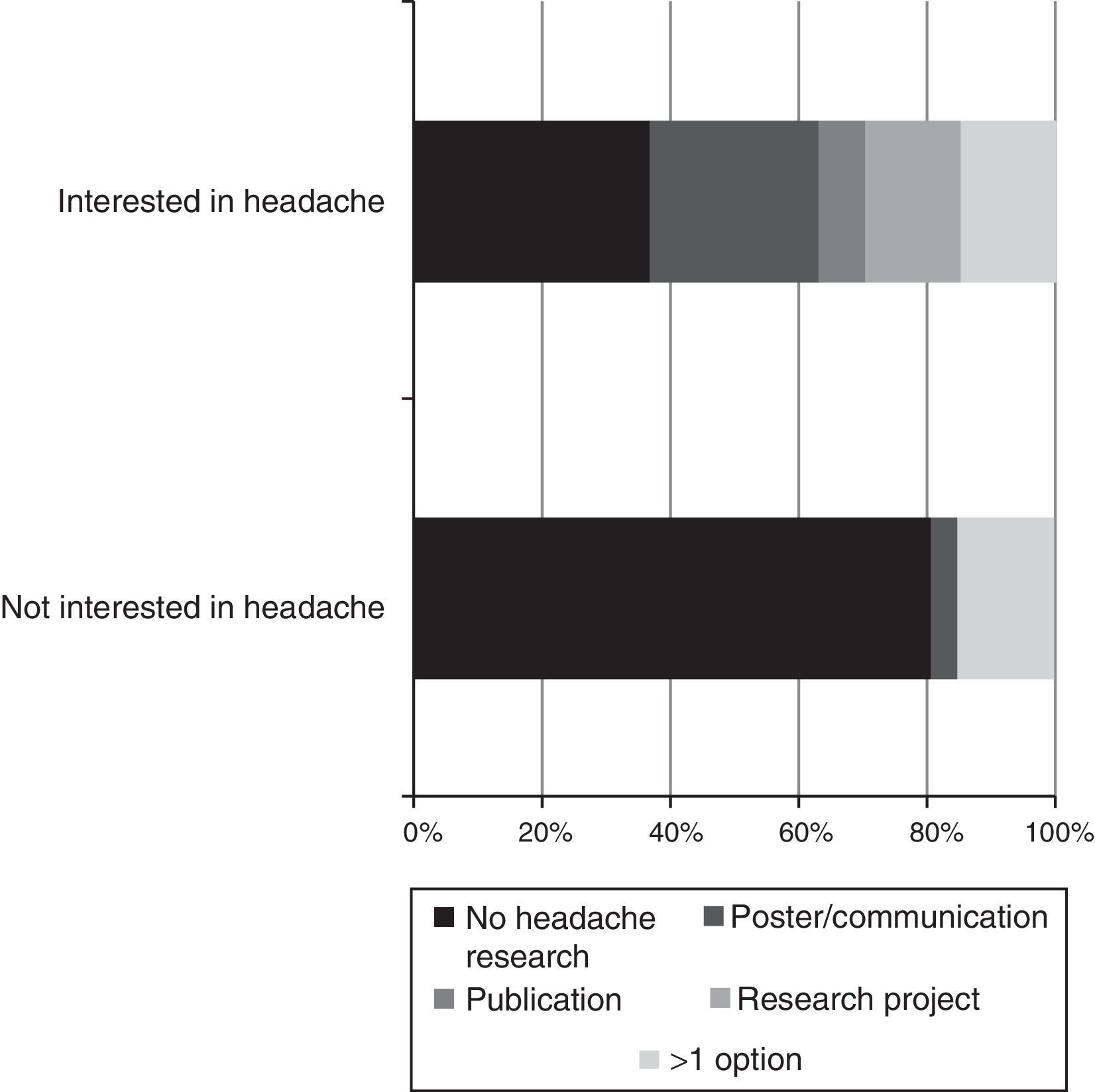
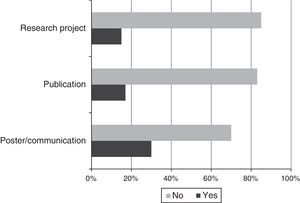
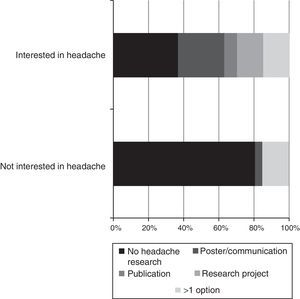
Research: 34% of residents believed that no research was performed, 47% believed scarce research was performed, and 19% believed a significant amount of research was performed. In terms of interest, 13% had no interest in headache research, 39% had some interest, and 48% were very interested. In terms of their involvement in research, 37 residents (69.8%) had never presented a poster or delivered a communication on headache, 44 (83%) had made no publications, and only 8 respondents (15%) were involved in a research project in the field (Fig. 3).
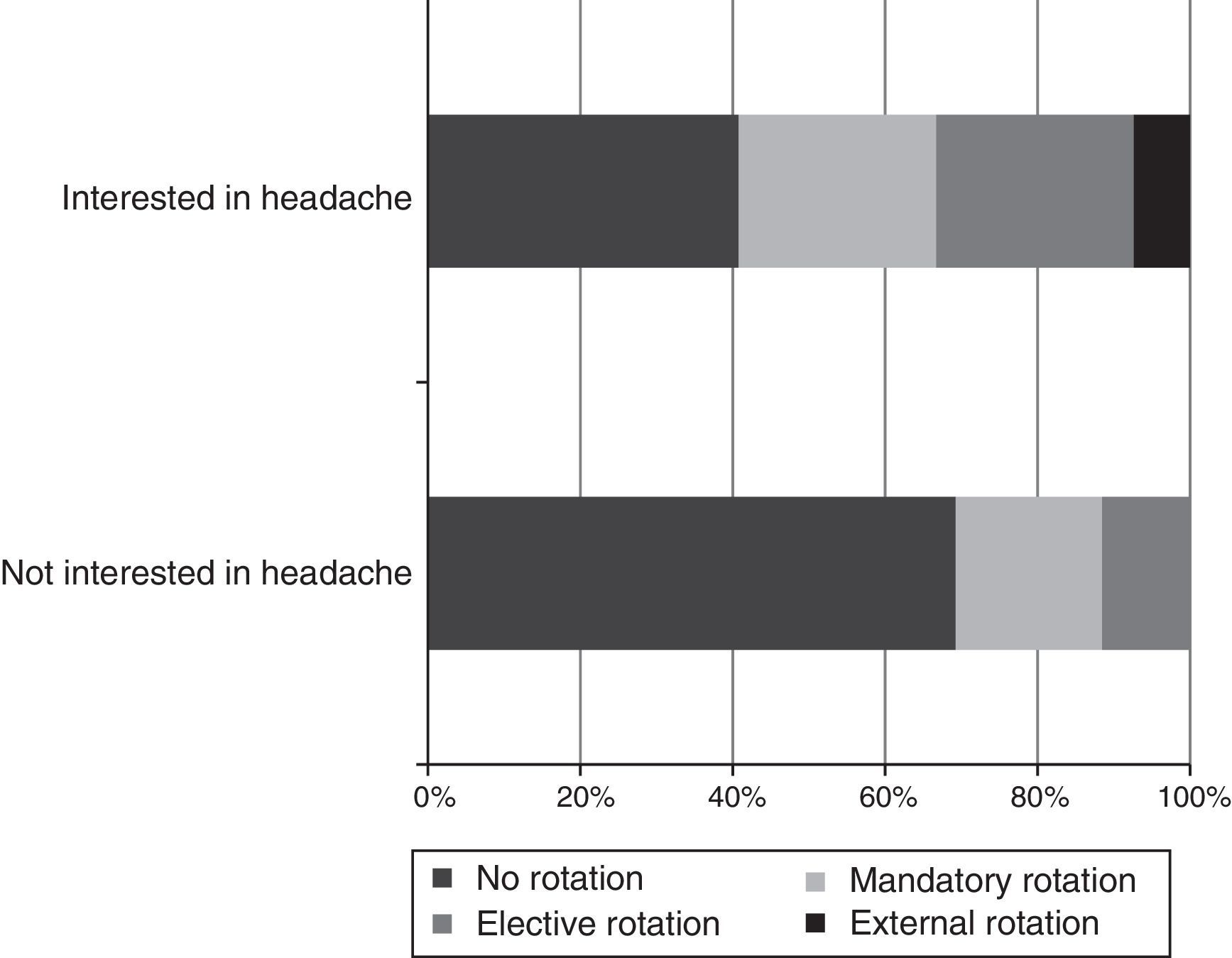
Subgroup analysis shows that headache rotations (Fig. 4) and receiving training in specific techniques (Fig. 5) result in residents having a greater interest in this field. Likewise, residents who were not involved in headache research showed considerably less interest in the disease (Fig. 6).
Taking into account the high level of subspecialisation in neurology, together with the need for a solid grounding in general neurology and related areas of medicine,1 the limited time for training, and the new core curriculum, modifying residency rotations to ensure that residents receive the best possible training is a constantly growing challenge. GECSEN believes that, in any case, upon completion of their training, neurology residents should be fully capable of managing patients with headache, performing the appropriate differential diagnosis, indicating the proper treatment, and performing the basic procedures of headache treatment. We believe that, with headache currently being the most frequent complaint among patients visiting neurology consultations, these abilities are the minimum that can be expected of neurologists.
Residents should follow comparable training programmes; it is also essential to follow criteria for teaching accreditation.7 It should be guaranteed that neurologists will learn similar skills regardless of where they are trained. As our results show, the availability of training in the different procedures mentioned varies greatly between centres. The root of this may be at a higher level: each training centre should push to have at least one staff neurologist specialising in headache. This leads us to suggest that the importance of training and practical experience in the field of headache is still not fully recognised in many Spanish training centres. This survey, which included residents from practically every region of Spain, is intended to give an overview of the current situation.
Although this is the first time headache training has been analysed in Spain, a number of studies, particularly in the United States, have addressed the issue from various perspectives. Finkel's research team8,9 has published several articles on the subject. The team's first study analysed 55 surveys from 46 institutions, and notes the limited training on headache given both to students (average one hour preclinical training and 2hours training at medical school) and residents (3hours). The second study surveyed centres with specific training programmes for residents; the questionnaire was sent to 133 centres, of which 95 (71.4%) responded. Ninety-two percent of centres had lectures for residents (number and duration of lectures are not specified); only 57% of residents could choose headache as an elective rotation (a somewhat higher proportion than that found in our results: 47%). There was a headache specialist at 76% of centres, with 57% having a specific headache unit (a similar proportion to that found in this study: 59%).
Another paper, highly related to our study, surveyed 93 neurologists from the New Investigators and Trainees Section of the American Headache Society, with 52.7% responding (a similar number of responses to our study); almost all respondents were young attending neurologists, fellows, or residents.10 Fewer than half (45.3%) had a rotation at a specialised headache centre during their residency; this figure is even lower than the one found in our results (47%). Another noteworthy detail of the American study is that only 2% of residents pursued headache fellowships. In early 2014, there were no fellows in this field in 32 states (63%), meaning that the country has a clear shortage of specialists to meet demand from patients with headache.
Although a somewhat higher proportion of the residents surveyed in our study were trained to perform botulinum toxin infiltration, very few were trained in anaesthetic blocks, with only one third of residents being competent in both techniques upon completion of their residency. In comparison, a survey of training programme directors in the USA (n=55; higher response rate among centres offering headache fellowships) found that a considerably higher number offered the opportunity to perform techniques under supervision: 65.5% for botulinum toxin infiltration and 60% for anaesthetic blocks.11 This training more often took place at ordinary clinics than in emergency departments or inpatient wards. However, formal accreditation was also infrequent (around 17%), and was mainly possible through the performance of a series of procedures under supervision (25%). Although very few residents had to wait to receive this accreditation before being permitted to perform these infiltrations (in only 7.3% of programmes), the procedures could not be performed independently in the majority of centres (only 27% permitted this). The majority of survey respondents (85%) believed that residents had sufficient procedural exposure; slightly over half (53%) believed that residents had gained sufficient competence upon completion of their training. Spanish legislation does not currently provide for specific training in headache as a subspecialty; however, the GECSEN does run an annual training course for residents. This includes both theoretical and practical content, is highly valued, and has high attendance. Attaining formal recognition within Spain's new legal framework12 would enable improvements to be made in the safety and effectiveness of these techniques.
The possibility of carrying out a rotation in a specialised clinic has a series of advantages, in the opinion of these authors; above all, a mentor specialising in headache is likely to transmit their knowledge and their passion for these patients. Differential diagnosis of headache can be a very complex process, as can selecting and administering an appropriate treatment option. Theoretical learning based on reading from the scientific literature is not a simple process; the best way of sharing experience is in everyday clinical practice. Tabby et al.13 describe how the most desirable ways of resolving problems with residents are increased supervision and assignation of a tutor/mentor; this is also reflected in papers by Johnson et al.14 and Minen et al.10; the latter reports that the main reasons for choosing to specialise in headache were having a mentor in the field, liking the patient population, and working in a headache unit (according to 64.7%, 52.9%, and 41.2% of participants, respectively). One highly interesting paper15 describes the reasons for which neurology residents choose to pursue subspecialty training: rather than demographic or educational factors, residents’ participation in research in the field and the teaching they received were decisive factors. This is clearly reflected in the present study, in which residents listing headache as one of their areas of interest were those who had participated in research, had worked in a specialised headache clinic, and who had been taught to perform both anaesthetic blocks and botulinum toxin infiltrations.
Regarding teaching, 40% of our respondents considered that they had not received adequate training. While this should indeed be a concern, other authors have described higher figures; in one study, while all survey respondents believed headache an essential area of study, only 25% considered their training to be adequate, with 80% believing efforts should be made to improve it.9 In another study, a survey sent to practising neurologists and tutors found that only 30% felt that they were capable of diagnosing pain disorders, with an even lower number (20%) feeling properly trained to treat them; 90% of respondents felt that they had received insufficient education in this field.16 Gallagher et al.17 evaluate the headache training both of neurologists and of primary care physicians; of the latter group, only one third had received more than 5 hours’ teaching on headache; only 41% saw more than 5 case presentations. This percentage was higher in neurology residents, without being an overwhelming majority (64% received over 5 hours’ teaching on headache); it is striking, however, that 80% had no plans to further build upon this experience.
The most frequent way that residents in our study expanded their knowledge was through providing care in hospitals; however, Johnson et al.14 report that as many as 71% considered that self-teaching was of greater assistance.
From a research perspective, it has been demonstrated that the studies residents publish constitute a basis for their future research.18 We believe, therefore, that promoting these research efforts during the neurology residency, always with the proper guidance and supervision, will strengthen this crucial area of residents’ professional development. Nonetheless, fewer than one in 3 residents in our sample had presented a poster or communication on headache; only 17% had published any written research or actively contributed to a research project. Particularly noteworthy was the fact that 81% of residents surveyed believed that little or even no research is being performed in the field of headache. There are several possible explanations for this: not reading neurology journals regularly, a lack of training sessions on headache at their hospitals; it may even be related to the sense that the subspecialty is undervalued.
The 3 most chosen subspecialties (except among R1 residents, whose data cannot be evaluated as only 3 completed the questionnaire) were vascular neurology, headache, and epilepsy, in that order. We are pleased that residents enjoy headache as a subspecialty, despite the aforementioned sense that it is undervalued. This is the case not only in Spain, but also in other countries such as the United States, where residents share this perception; many consider headache to be a psychogenic disease, that the subspecialty is not as “hard core” as other areas of neurology, and that the residency was more inpatient-focused.10
We should reiterate that our survey had a fairly low response rate, which would constitute a limitation of the study; however, the final number of respondents is similar to that of similar publications. One implication of this may be that the evaluations of respondents were biased by their greater interest in headache; the true situation may therefore be worse than our results suggest.
In conclusion, a significant barrier to improving patient care in the field of headache is a shortage of specialists, limited training, and a negative perception of the field. The Executive Board of GECSEN believes that efforts should be made for improvement on several key points. Firstly, a rotation in specific headache clinics should be a part of every neurology resident's training; as well as improving their ability to diagnose and treat these patients, residents would also become skilled in basic technical procedures. Efforts should also be made to promote training courses, to make the GECSEN's webpage more dynamic, and to involve residents in research projects. Everything that is done to expand their knowledge in this period will leave a mark on their future careers.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank all the residents who participated in the study, the SEN's scientific division (Mercè Casellas), and Dr José Vivancos Mora for his invaluable help in reviewing the paper.
Please cite this article as: Gago-Veiga AB, Santos-Lasaosa S, Romero JV, Pozo-Rosich P. ¿Se interesan los residentes de Neurología en la cefalea? Neurología. 2018;33:1–7.
This study was presented as an oral communication at the 67th Annual Meeting of the Spanish Society of Neurology, Valencia, 2015. Part of the study was presented as a poster at the Annual Meeting of the Madrid Association of Neurology, Madrid, 2015.