We estimate the proportion of participants willing to pay the US price (€30) or €20 for an HIV self-test and analyse their associated factors.
MethodsIn a street-based testing program, 497 participants in a feasibility self-test study answered the question, “What would be the maximum price you would be willing to pay for a similar test to this one so you can use it at your convenience?”
ResultsOnly 17.9% would pay ≥€30, while 40.0%, ≥€20. In the logistic regression, paying more was associated with being tested outside the campuses and having paid or been paid for sex.
ConclusionIn Spain, self-testing would not have an impact unless it became more affordable to potential users.
Estimamos la proporción de participantes dispuestos a pagar por un autotest de VIH su precio en EEUU. (30€), o 20€, y analizamos factores asociados.
MétodosEn un programa de diagnóstico ofertado en la calle, 497participantes de un estudio de factibilidad del auto-test respondieron a la pregunta: ¿Cuál sería el precio máximo que estarías dispuesto a pagar por una prueba como esta para poder realizártela cuando estimaras oportuno?
ResultadosEl 17,9% pagaría ≥30€ y el 40,0% ≥20€. En la regresión logística pagar más estuvo asociado con participar fuera de las universidades y haber pagado o sido pagado por sexo.
ConclusiónEl autotest no tendrá impacto en España si su precio no disminuye a un valor más asequible para los potenciales usuarios.
HIV self-testing could become an alternative and complementary diagnostic strategy capable of filling gaps not covered by existing approaches. It might become an option for those unwilling to attend current services, make more frequent testing easier for people at high risk, facilitate HIV testing to sex partners and be used to detect window period infections with repeated testing in persons with recent potential exposure to HIV.1 The U.S. Food and Drug Administration approved the first self-administered HIV test kit in the U.S. in the fall of 2012.2 The test was released to the market with the current $39.99 retail price (around €30).3 However, despite the possibilities it offers, a cost not affordable to potential users could limit its use. We consequently estimated the proportion of participants in a Spanish HIV self-test feasibility study willing to pay at least the established US price of €30 or a lower price of at least €20 for an HIV self-test, and their correlates.
MethodsBetween October 2009 and February 2010, a self-testing feasibility study was conducted with an HIV rapid test involving 519 Spanish-speaking attendees of a street-based testing program in Spain. The design and procedures of the study have been previously described.4
The participants’ attitude about self-testing, their motivation to use it in the future and their response to the question “What would be the maximum price you would be willing to pay for a similar test to this one so you can use it at your convenience?” were assessed by means of a self-administered questionnaire. Data on sociodemographics, risk behavior and HIV testing history were also collected.
Based on the 497 (95.7%) participants who answered the question on prices, we estimated the proportion willing to pay ≥€30 (the US retail price). Given that the resulting proportion was very low we calculated who would pay lower prices and then chose a second cut point of ≥€20, a price we considered to be more affordable but still subsidizable or attainable in the future as self-test retail price. We also performed a bivariate analysis to explore the association between willingness to pay different prices and demographic and behavioral characteristics, motivation to get tested, and HIV experience. We calculated the odds ratio (OR), its 95% confidence interval (CI) and the statistical significance with the Chi-square and performed logistic regression analysis including those variables with p<0.1. The study protocol was approved by the institutional review board of the Instituto de Salud Carlos III.
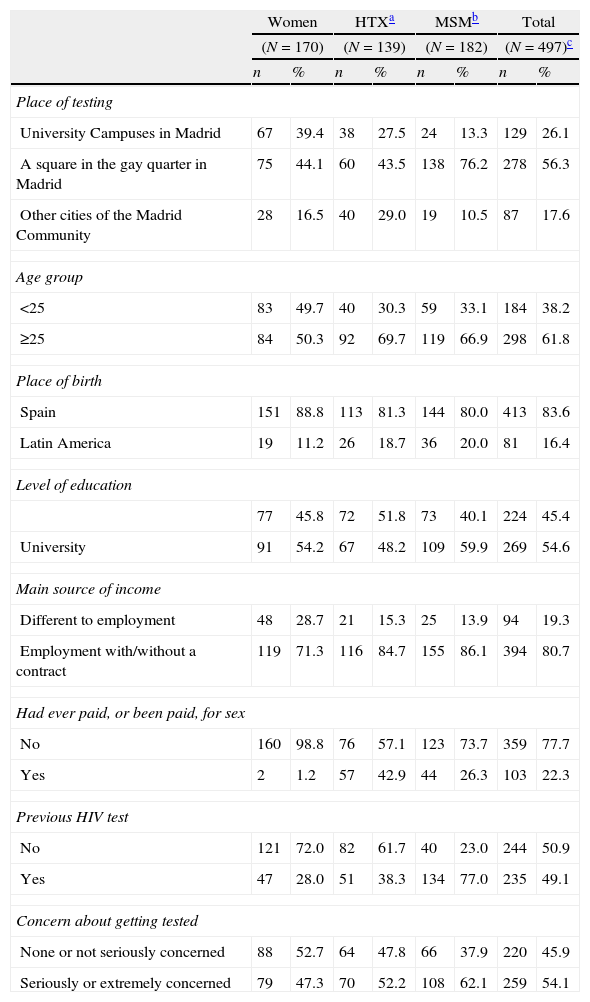
ResultsAbout one-third of the sample were men who had sex with men (MSM), one-third were heterosexual men (HTX) and the last third were women; slightly more than half were enrolled in a square in the Madrid gay quarter; 38.2% were under 25 years of age, 16.4% were Latin Americans, 54.6% had a university degree, 80.7% had an employment as main source of income, 77.7% had never paid or been paid for sex, 49.1% had had a previous HIV test and 54.1% were seriously or extremely concerned about getting the test (Table 1).
Demographic, behavioral characteristics and HIV testing experience of study participants who answered the question on self-test prices by gender/sexual behavior.
| Women | HTXa | MSMb | Total | |||||
| (N=170) | (N=139) | (N=182) | (N=497)c | |||||
| n | % | n | % | n | % | n | % | |
| Place of testing | ||||||||
| University Campuses in Madrid | 67 | 39.4 | 38 | 27.5 | 24 | 13.3 | 129 | 26.1 |
| A square in the gay quarter in Madrid | 75 | 44.1 | 60 | 43.5 | 138 | 76.2 | 278 | 56.3 |
| Other cities of the Madrid Community | 28 | 16.5 | 40 | 29.0 | 19 | 10.5 | 87 | 17.6 |
| Age group | ||||||||
| <25 | 83 | 49.7 | 40 | 30.3 | 59 | 33.1 | 184 | 38.2 |
| ≥25 | 84 | 50.3 | 92 | 69.7 | 119 | 66.9 | 298 | 61.8 |
| Place of birth | ||||||||
| Spain | 151 | 88.8 | 113 | 81.3 | 144 | 80.0 | 413 | 83.6 |
| Latin America | 19 | 11.2 | 26 | 18.7 | 36 | 20.0 | 81 | 16.4 |
| Level of education | ||||||||
| 77 | 45.8 | 72 | 51.8 | 73 | 40.1 | 224 | 45.4 | |
| University | 91 | 54.2 | 67 | 48.2 | 109 | 59.9 | 269 | 54.6 |
| Main source of income | ||||||||
| Different to employment | 48 | 28.7 | 21 | 15.3 | 25 | 13.9 | 94 | 19.3 |
| Employment with/without a contract | 119 | 71.3 | 116 | 84.7 | 155 | 86.1 | 394 | 80.7 |
| Had ever paid, or been paid, for sex | ||||||||
| No | 160 | 98.8 | 76 | 57.1 | 123 | 73.7 | 359 | 77.7 |
| Yes | 2 | 1.2 | 57 | 42.9 | 44 | 26.3 | 103 | 22.3 |
| Previous HIV test | ||||||||
| No | 121 | 72.0 | 82 | 61.7 | 40 | 23.0 | 244 | 50.9 |
| Yes | 47 | 28.0 | 51 | 38.3 | 134 | 77.0 | 235 | 49.1 |
| Concern about getting tested | ||||||||
| None or not seriously concerned | 88 | 52.7 | 64 | 47.8 | 66 | 37.9 | 220 | 45.9 |
| Seriously or extremely concerned | 79 | 47.3 | 70 | 52.2 | 108 | 62.1 | 259 | 54.1 |
% were calculated excluding missings.
The proportion of participants who would purchase the test if the price was ≥€30 was 17.9% (CI 14.4–21.4) while the proportion willing to pay €20 or more rose to more than double (40.0%; CI 36.6–44.4). Those who would pay €0 represented 5.2%, while the proportion willing to pay less than €10 (including those reluctant to pay) was 25.8%. The proportion of participants willing to pay €10 or more was 74.2% (CI 70.3–78.2), willing to pay €15 or more was 49.5% (CI 45.0–54.0), and willing to pay €25 or more was 20.3% (CI 16.7–24.0). Participants tended to choose round numbers and the most frequent values were €10 (21.6%), €20 (18.5%) and €5 (12.1%).
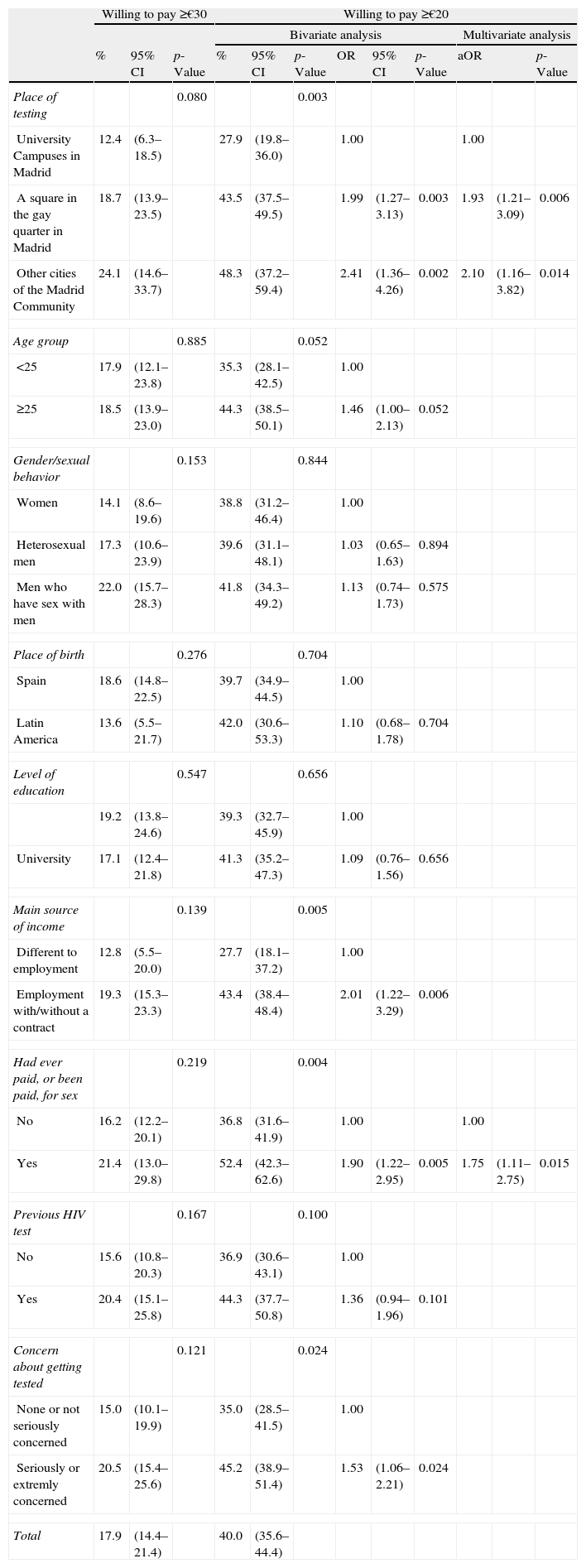
There were no significant sociodemographic, behavioral or HIV-testing variables related with the willingness to pay ≥€30 (Table 2). However, four variables were found to be significantly related with willing to pay €20 or more: place of testing, main source of income, having ever paid and/or been paid for sex and concern about getting tested (as appraised from the answer to the question “before coming to this service, had you been thinking for some time that you should take the test?”). The age group variable was also close to being significantly related with willingness to pay €20 or more. Those who got tested outside university campuses, or who had an employment as principal source of income, or had ever paid or been paid for sex, expressed around 15% points more willingness to pay ≥€20. Multivariate analysis revealed two independent variables: place of testing and having paid or been paid for sex.
Percentage of participants and factors associated with willing to pay ≥€30 or ≥€20 for an HIV self-test, according to their demographic, behavioral characteristics and HIV testing experience.
| Willing to pay ≥€30 | Willing to pay ≥€20 | |||||||||||
| Bivariate analysis | Multivariate analysis | |||||||||||
| % | 95% CI | p-Value | % | 95% CI | p-Value | OR | 95% CI | p-Value | aOR | p-Value | ||
| Place of testing | 0.080 | 0.003 | ||||||||||
| University Campuses in Madrid | 12.4 | (6.3–18.5) | 27.9 | (19.8–36.0) | 1.00 | 1.00 | ||||||
| A square in the gay quarter in Madrid | 18.7 | (13.9–23.5) | 43.5 | (37.5–49.5) | 1.99 | (1.27–3.13) | 0.003 | 1.93 | (1.21–3.09) | 0.006 | ||
| Other cities of the Madrid Community | 24.1 | (14.6–33.7) | 48.3 | (37.2–59.4) | 2.41 | (1.36–4.26) | 0.002 | 2.10 | (1.16–3.82) | 0.014 | ||
| Age group | 0.885 | 0.052 | ||||||||||
| <25 | 17.9 | (12.1–23.8) | 35.3 | (28.1–42.5) | 1.00 | |||||||
| ≥25 | 18.5 | (13.9–23.0) | 44.3 | (38.5–50.1) | 1.46 | (1.00–2.13) | 0.052 | |||||
| Gender/sexual behavior | 0.153 | 0.844 | ||||||||||
| Women | 14.1 | (8.6–19.6) | 38.8 | (31.2–46.4) | 1.00 | |||||||
| Heterosexual men | 17.3 | (10.6–23.9) | 39.6 | (31.1–48.1) | 1.03 | (0.65–1.63) | 0.894 | |||||
| Men who have sex with men | 22.0 | (15.7–28.3) | 41.8 | (34.3–49.2) | 1.13 | (0.74–1.73) | 0.575 | |||||
| Place of birth | 0.276 | 0.704 | ||||||||||
| Spain | 18.6 | (14.8–22.5) | 39.7 | (34.9–44.5) | 1.00 | |||||||
| Latin America | 13.6 | (5.5–21.7) | 42.0 | (30.6–53.3) | 1.10 | (0.68–1.78) | 0.704 | |||||
| Level of education | 0.547 | 0.656 | ||||||||||
| 19.2 | (13.8–24.6) | 39.3 | (32.7–45.9) | 1.00 | ||||||||
| University | 17.1 | (12.4–21.8) | 41.3 | (35.2–47.3) | 1.09 | (0.76–1.56) | 0.656 | |||||
| Main source of income | 0.139 | 0.005 | ||||||||||
| Different to employment | 12.8 | (5.5–20.0) | 27.7 | (18.1–37.2) | 1.00 | |||||||
| Employment with/without a contract | 19.3 | (15.3–23.3) | 43.4 | (38.4–48.4) | 2.01 | (1.22–3.29) | 0.006 | |||||
| Had ever paid, or been paid, for sex | 0.219 | 0.004 | ||||||||||
| No | 16.2 | (12.2–20.1) | 36.8 | (31.6–41.9) | 1.00 | 1.00 | ||||||
| Yes | 21.4 | (13.0–29.8) | 52.4 | (42.3–62.6) | 1.90 | (1.22–2.95) | 0.005 | 1.75 | (1.11–2.75) | 0.015 | ||
| Previous HIV test | 0.167 | 0.100 | ||||||||||
| No | 15.6 | (10.8–20.3) | 36.9 | (30.6–43.1) | 1.00 | |||||||
| Yes | 20.4 | (15.1–25.8) | 44.3 | (37.7–50.8) | 1.36 | (0.94–1.96) | 0.101 | |||||
| Concern about getting tested | 0.121 | 0.024 | ||||||||||
| None or not seriously concerned | 15.0 | (10.1–19.9) | 35.0 | (28.5–41.5) | 1.00 | |||||||
| Seriously or extremly concerned | 20.5 | (15.4–25.6) | 45.2 | (38.9–51.4) | 1.53 | (1.06–2.21) | 0.024 | |||||
| Total | 17.9 | (14.4–21.4) | 40.0 | (35.6–44.4) | ||||||||
CI, confidence interval; aOR, adjusted odd ratio.
Only one out of six participants was willing to pay the 30€ current cost for the over-the-counter self-test licensed in USA, but this proportion would double if the price dropped to €20. It should be noted that all the participants were potential users who had just experienced self-testing and that the study included not only men who have sex with men, but also heterosexual men and women, Spanish and Latin American immigrants.
Although several published studies cover the subject of willingness to pay,5–9 it would be difficult to compare those results with ours for several reasons: different price cut points,6–9 participation of HIV positive subjects who are not potential self-test users6,7,9 and old publication dates.8,9 Katz et al. found very similar results in the US: 17% of participants enrolled in a trial to evaluate the impact of access to home self-testing would pay ≥$40,5 although all were men who have sex with men. So the results in Spain are not surprising, taking into account that free access to HIV tests and health care are considered an intrinsic part of the welfare state.
The fact that those who had paid or had been paid for sex showed greater willingness to pay more, could indicate knowledge of engaging in a high risk behavior subject to social disapproval, which could incite them to get tested confidentially. Also, the percentage of people with employment as main source of income willing to pay, is significantly higher than the percentage of those with other main sources of income, perhaps indicating a better or at least more stable income and spending capacity. Yet this variable was not significant in the multivariated analysis. At the same time, the percentage of those willing to pay ≥€20 who attended the program in university campuses in Madrid is significantly lower than those who participated in Madrid City and other cities of the Madrid Community. We know that the campus sample population is younger, with a much greater proportion of women and Spaniards, fewer people whose main source of income is employment, with less precedent of having paid or been paid for sex and of previous HIV testing.
The study was performed before self-testing was released in the U.S. market and news about it were published in the Spanish press.10,11 Results might have been different if a reference price had been specified to the participants, or if the test was already available in Spain. Another factor to consider is the lack of statistical power to detect some differences due to the number of participants. Furthermore, study subjects were the beneficiaries of a free rapid test program. Nevertheless, it seems that home self-testing would not have the expected impact unless it became more affordable to potential users, although additional studies must be conducted in different populations if we are to get a more realistic view of the extent to which certain prices would not be affordable for certain populations.
FundingThis study was funded by Ministry of Health, Social Services and Equality (Ministerio Sanidad – EC11-279) and the Fondo de Investigación Sanitaria (FIS:PI09/90748).
Conflict of interestsThe authors declare no conflict of interest.