Adenosine deaminase (ADA) is an enzyme which catalyzes the deamination of adenosine during the formation of inosine and, as such, plays an important role in the proliferation, maturation and differentiation of T-lymphocytes.1 Levels of ADA in cerebrospinal fluid (CSF) greater than 9–10IU/l are associated with a tuberculous aetiology.1–4 However, these levels have also been observed in other aetiologies, especially infectious meningitis, such as Listeria,5Brucella,3Cryptococcus, Toxoplasma, herpes simplex virus (HSV),6Plasmodium and in some non-infectious diseases, such as lymphomatous meningitis. The objective of this study was to investigate the characteristics of CSF, including ADA levels, in patients with meningitis caused by HSV, varicella zoster virus (VZV) and Listeria, which, in some cases, may be indistinguishable from tuberculosis.
We retrospectively reviewed all patients diagnosed with meningitis or encephalitis caused by HSV (type-1 and 2), VZV and Listeria between January 2005 and June 2010, where ADA in CSF had been determined. The microbiological diagnosis of HSV and VZV between January 2005 and February 2008 was obtained by demonstrating the viral cytopatic effect (Light Diagnostics™ HSV-1/2 Typing DFA Kit; Light Diagnostics™ VZV Antibody FITC Reagent. Chemicon, Millipore) in a human lung fibroblast monolayer (MRC-5) cell culture, and from February 2008 by amplification of viral DNA in the CSF by PCR (LightCycler®-VZV Qual Kit y LightCycler®-HSV-1/2 Qual Kit, Roche). We collected the epidemiological characteristics, clinical data, laboratory tests and microbiological studies of all the included patients. Quantitative variables were expressed as mean±standard deviation (SD) and qualitative variables as absolute value and percentage. We studied the correlation between quantitative variables using the Spearman or Pearson correlation coefficients, as appropriate. The comparison of qualitative variables was done by chi-squared test. Statistical significance was established at P<0.05. The study protocol was approved by the Ethics Committee of the A Coruña University Hospital Complex.
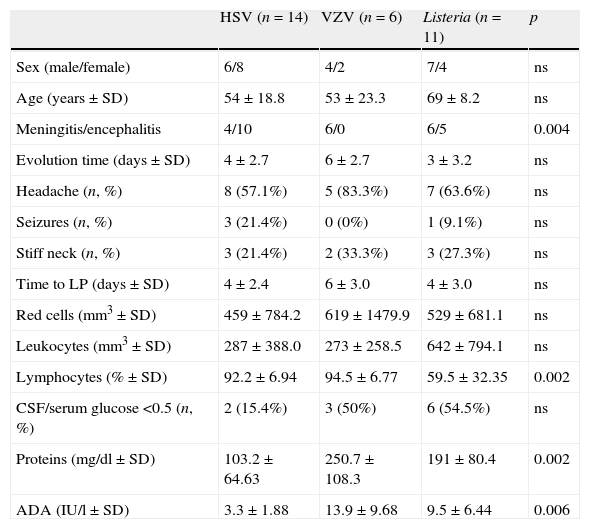
We included 31 patients with meningitis or encephalitis: 14 HSV, 6 VZV and 11 Listeria. The clinical and epidemiological characteristics of the patients and test results of the CSF are shown in the Table 1. Of the 6 patients with meningitis caused by VZV, 3 had cutaneous zoster lesions. The ADA value was correlated with the protein value (r=0.001). Among VZV meningitis, 50% of the patients had an ADA≥9UI/l, and 83% ADA≥8IU/I, while only 36.4% of the Listeria meningitis had an ADA≥9IU/l. Initially, no patient with meningitis–encephalitis caused by HSV had raised ADA levels, although in the second lumbar puncture, performed in 7 of these patients, ADA level was 11±3.80IU/l, however significant differences were not observed in the protein value between the first and second lumbar punctures (103.2±64.64 vs. 95.9±31.65mg/dl, P=0.75).
Epidemiologic, clinical and CSF characteristics of patients with meningitis or encephalitis caused by HSV, VZV and Listeria.
| HSV (n=14) | VZV (n=6) | Listeria (n=11) | p | |
| Sex (male/female) | 6/8 | 4/2 | 7/4 | ns |
| Age (years±SD) | 54±18.8 | 53±23.3 | 69±8.2 | ns |
| Meningitis/encephalitis | 4/10 | 6/0 | 6/5 | 0.004 |
| Evolution time (days±SD) | 4±2.7 | 6±2.7 | 3±3.2 | ns |
| Headache (n, %) | 8 (57.1%) | 5 (83.3%) | 7 (63.6%) | ns |
| Seizures (n, %) | 3 (21.4%) | 0 (0%) | 1 (9.1%) | ns |
| Stiff neck (n, %) | 3 (21.4%) | 2 (33.3%) | 3 (27.3%) | ns |
| Time to LP (days±SD) | 4±2.4 | 6±3.0 | 4±3.0 | ns |
| Red cells (mm3±SD) | 459±784.2 | 619±1479.9 | 529±681.1 | ns |
| Leukocytes (mm3±SD) | 287±388.0 | 273±258.5 | 642±794.1 | ns |
| Lymphocytes (%±SD) | 92.2±6.94 | 94.5±6.77 | 59.5±32.35 | 0.002 |
| CSF/serum glucose <0.5 (n, %) | 2 (15.4%) | 3 (50%) | 6 (54.5%) | ns |
| Proteins (mg/dl±SD) | 103.2±64.63 | 250.7±108.3 | 191±80.4 | 0.002 |
| ADA (IU/l±SD) | 3.3±1.88 | 13.9±9.68 | 9.5±6.44 | 0.006 |
Note: LP lumbar puncture, CSF cerebrospinal fluid.
Encephalitis diagnosis was established when abnormalities in brain function were observed (altered mental status, motor or sensory deficits, altered behaviour and personality changes, and speech or movement disorders).
In countries in which tuberculosis is endemic, determination of ADA in CSF is usually performed as an initial screening of tuberculous meningitis, however the low sensitivity of this test means that the usefulness of ADA in CSF still remains controversial. A recent meta-analysis7 did not find a valid cut-off value for the correct discrimination between tuberculous and pyogenic meningitis. Nonetheless, several studies have shown the usefulness of ADA for differentiating between tuberculous meningitis and aseptic or viral meningitis, in which the ADA levels are usually low (2.58–7.39IU/l).1–4,8 In our study we found that patients with meningitis caused by VZV had much higher ADA levels than expected for viral meningitis (13.9±9. 68IU/l). We believe that this finding could be related to the degree of meningeal inflammation and to the level of proteins, since patients with meningitis caused by VZV had the highest protein levels in CSF, and because increased protein diffusion through the vascular walls has been associated with an increase in ADA levels.9 Nonetheless, multiple factors must have an influence on the relationship between ADA and proteins in CSF. Thus, in our series, it was seen that, for the evolution of meningitis–encephalitis caused by HSV, the ADA level rises even though the protein value does not.
In some of the patients the raised levels of ADA lead to a first suspected diagnosis of tuberculous meningitis, until VZV-DNA was detected in the CSF. This is because both pathologies can have similar CSF characteristics, such as lymphocytic predominance, raised ADA and glucose consumption,10 and, moreover, zoster skin lesions can be absent in up to half of the patients with VZV meningitis, as was observed in our study.
The usefulness of the ADA levels in CSF samples continues to be controversial, since several cases of meningitis with increased ADA are constantly being published, to which we may now add VVZ meningitis. However, we believe that the determination of ADA levels in CSF is still useful for, in the appropriate clinical context, not delaying the onset of anti-tuberculous treatment. The quick detection of viral DNA by PCR is highly useful for the diagnosis of aseptic meningitis.