Female, 56 years of age, with a history of smoking 160 packs per year, without prior incidents of interest, was admitted to the emergency room for exhibiting, for various weeks, a fluctuating mass with edema and pain in the left breast. The patient's primary care physician, who had been informed of the same symptoms described, prescribed a treatment of amoxicillin-clavulanate. After 15 days without improvement and with the appearance of fever, the patient decided to be admitted to the hospital. After assessing with the surgery department, purulent material that was obtained from lesion drainage was sent to the Microbiology department for culture. The patient was discharged with antibiotic treatment the same day.
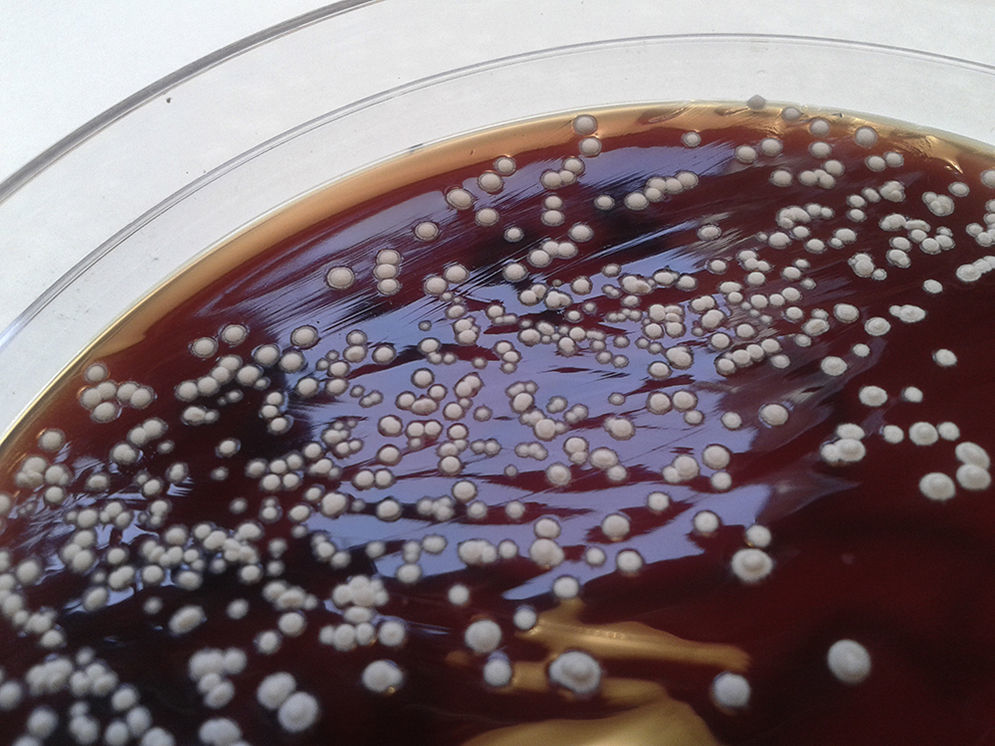
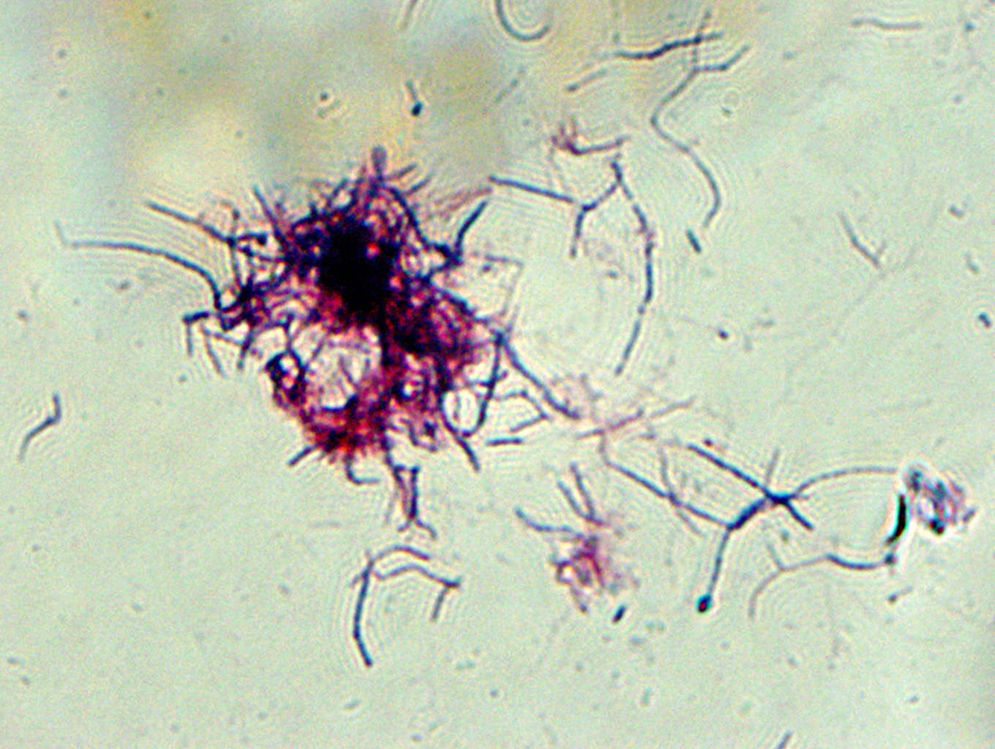
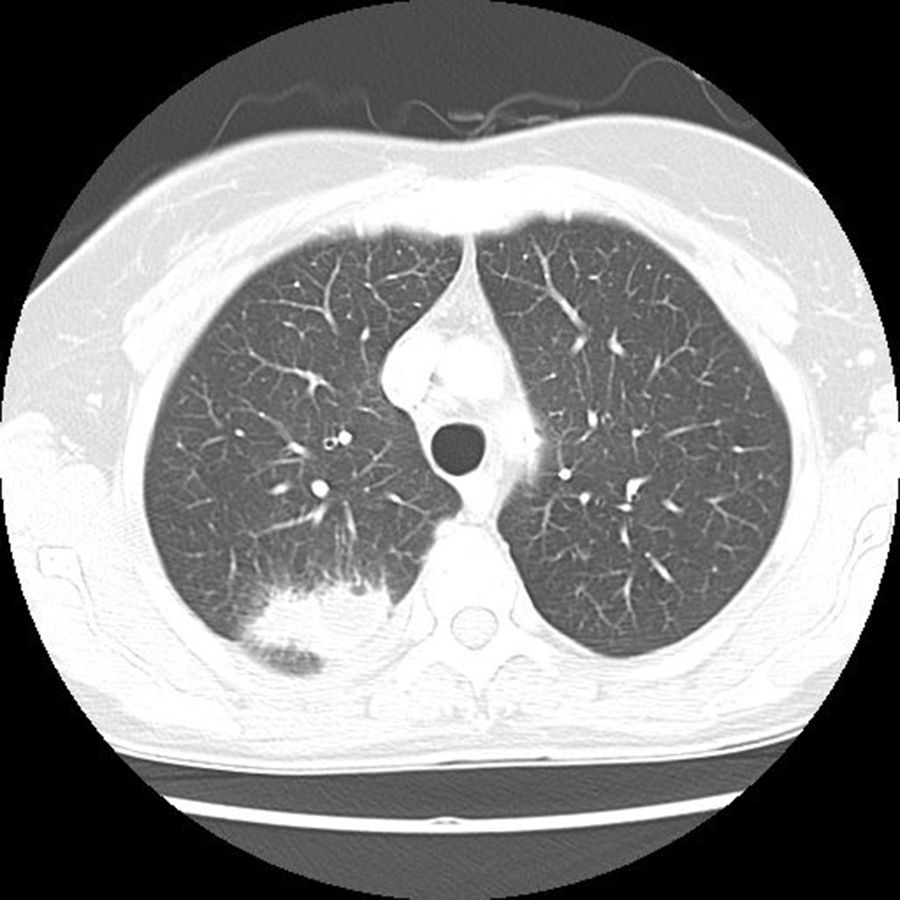
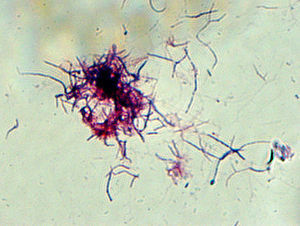
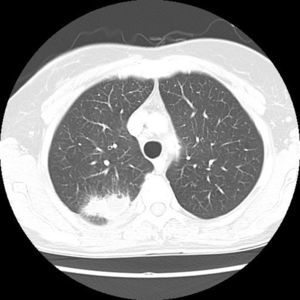
After 48hours, tiny white colonies with cotton-like features were observed in the culture (Fig. 1). Gram staining was performed on the colonies which resulted in a branched Gram-positive bacilli visualization (Fig. 2). With the suspicion of Nocardia spp, the surgery department was advised to forward the patient to the department of infectious diseases. The bacterial strain was sent to the National Microbiology center in Majadahonda for its definitive identification. In addition, in order to conduct further studies, the patient was readmitted to the hospital and given an intravenous antibiotic treatment of cotrimoxazole. A magnetic resonance imaging (MRI) of the brain was performed but no significant findings were obtained. Moreover, a chest X-ray was done in which a suspicious manifestation was visualized in the right superior lobe. The images obtained from the chest CT scan revealed a 2×4.5cm pulmonary mass in the posterior segment of the right superior lobe, with irregularly barbed borders and heterogeneous density, the interior center being less dense (necrosis vs. purulent material), as if a gas bubble was located in the superior portion. The lesion made contact with and swelled the adjacent pleura (Fig. 3). The radiology report suggested the possibility of neoplasia due to the smoking history of the patient, however it was unable to rule out infectious/inflammatory disease.
The patient never mentioned having any respiratory symptoms.
During the bronchoscopy, the permeable lobes were observed but no significant pathological findings were seen. The samples obtained were sent to the Microbiology department but had no significant growth in their cultures. In addition, Nocardia spp was not isolated in the sputum samples that were sent. The respiratory samples that were sent to the pathological anatomy department found no evidence for malignant cells.
Serological testing for HIV, HBV, HCV, Mycoplasma pneumoniae, Chlamydophila pneumoniae, Coxiella burnetti, and Rickettsia conorii all resulted negative.
EvolutionPending the PET scan, the patient was discharged due to the good evolution, and the absence of contrasting clinical data, with cotrimoxazol oral treatment.
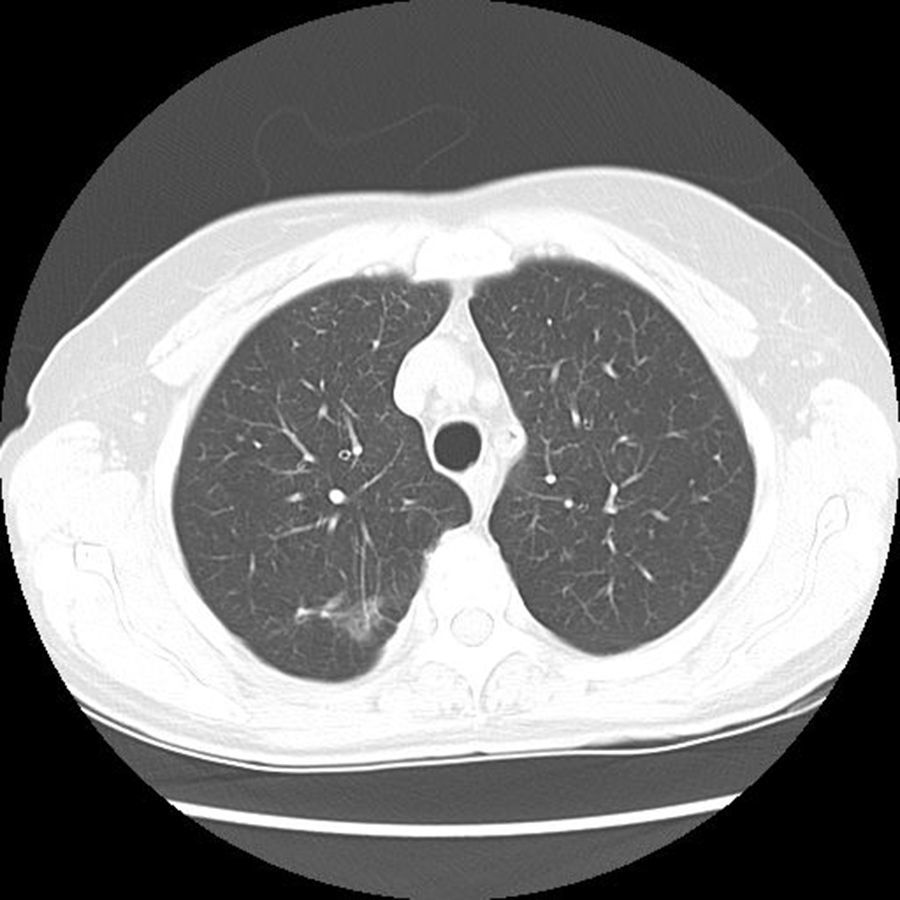
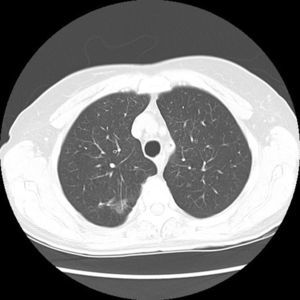
In the PET scan, a hypemetabolic pulmonary mass in the right superior lobe was detected with the suspicion of malignancy, unable to rule out inflammation or infectious pathology, suggesting histological affiliation to the lesion. In the CT control scan, the pulmonary lesion had evidently improved (Fig. 4) which stopped the study by thoracic surgery, suggesting the infectious etiology as the most probable cause given by the results of the imaging tests and the absence of symptoms. After nine months, the cotrimoxazol antibiotic treatment had been suspended, following the disappearance of the patient's symptoms.
The definitive identification of the microorganism that the strain corresponded to was determined to be Nocardia abscessus.
CommentsThe genus Nocardia consists of aerobic, branched, Gram-positive, bacilli. More than 80 species have been identified, of them 33 capable of infecting humans and causing disease.1N. cyriacigeorgica, N. farcinica, N. nova, N. abscessus, and N. carnea are frequently seen in the clinical setting. The bacteria is generally acquired via inhalation, cutaneous contact or ingestion. Bacterial infection is typically seen in immunosuppressed patients, however it is estimated that one third of infections with Nocardia spp. have been reported in immunocompetent patients. Factors associated with bacterial infection are, but not limited to, diabetes, alcoholism, COPD, anti-TNF treatments, IDU patients, and tuberculosis.2 Systematic infection is more frequent in immunosuppressed patients but cases have been reported where brain abscess and pulmonary infection were presented in immunocompetent patients.3
N. abscessus, previously named Nocardia asteroides type 1, was characterized in the year 2000 by polyphasic taxonomy analysis of four isolated clinical patients.4 Bacterial infections of this species have been linked to brain abscess, pericarditis, skin and soft tissues infections and pulmonary infections.5
The preferred treatment for Nocardia is cotrimoxazol alone or associated with dapsone, amikacin, or third generation cephalosporins. In cases where cotrimoxazol causes an allergic reaction, it is recommended to desensitize patient. Alternative treatments include amikacin, imipenem, meropenem, third generation cephalosporins, and linezolid.6
In our case, the isolation of Nocardia in the breast abscess was not accompanied with growth in the samples from the tracheobronchial tree, although the good evolution of the pulmonary lesion with the specific treatment for the microorganism, coupled with the chronological finding of the abscess, suggested that the pulmonary lesion may have been caused by the same etiology. Following protocols for extracerebral nocardiosis patients,7 cerebral MRI scans were taken, but no lesions were found.