Parathyroid cysts were first described in 1880 by Sandström, but the first surgical resection was not performed until 1905 by Goris. These cysts can be classified as functioning, which occur with primary hyperparathyroidism, or non-functioning. The latter are the most frequent, representing 80%–90% of all parathyroid cysts.1,2 In addition, cystic parathyroid lesions account for 0.075% of cervical ultrasounds.3
Functional parathyroid cysts are managed like primary hyperparathyroidism, whose treatment of choice is surgery. Thus, functioning parathyroid cysts account for 3% of parathyroidectomies performed by primary hyperparathyroidism.4
In contrast, the management of non-functioning cysts is conservative, with drainage by needle aspiration being the treatment of choice. Regarding the etiopathogenesis of these non-functioning cysts, there are 2 theories: the first is that they originate in the embryonic period from the 3rd and 4th pharyngeal arches; the second indicates that they originate by fusion of parathyroid microcysts caused by degeneration of the gland or retention of secretions that form microcysts.1
The objective of this case report is to analyze the management of non-functioning parathyroid cysts refractory to drainage with needle aspiration.
Patients with parathyroid cysts that met the following criteria are included in this report: (a) ultrasound or computed tomography (CT) diagnosis of parathyroid cysts; (b) fluid obtained by needle aspiration, with limited cellularity and a concentration of parathyroid hormone (PTH) greater than in plasma (>9–65pg/ml); (c) no hyperparathyroidism (normal plasma PTH and calcium levels); (d) previous treatment with percutaneous drainage; and (e) recurrence of the cyst, with a size greater than 3cm in diameter.
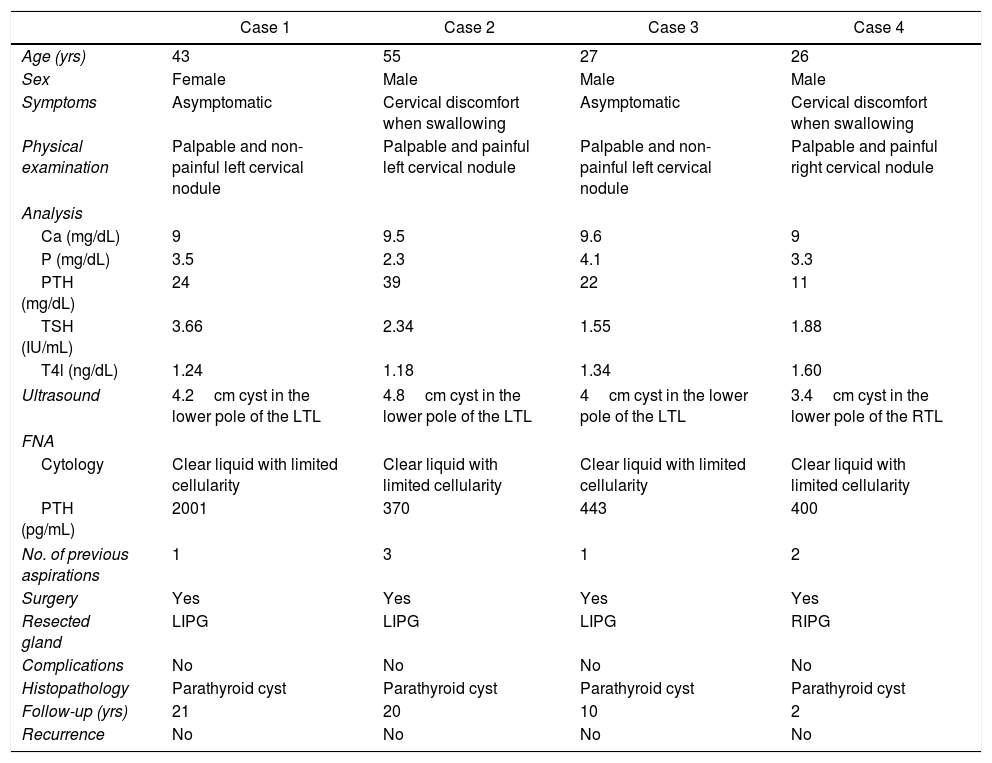
Four patients met the inclusion criteria (Table 1), which represents 0.43% of all parathyroid disease treated surgically at our hospital in the same period of time. Excluded from the series were 3 treated parathyroid cysts as they were functioning and treated as primary hyperparathyroidism. 75% (n=3) of patients were male and mean age was 37.7±13.8 years. 75% (n=3) of the non-functioning cysts were located in the left lower parathyroid gland. In the 4 cases (100%), surgery was indicated, entailing parathyroidectomy of the affected gland. Being non-functioning cysts, they did not require intraoperative monitoring of PTH. There were no complications in the postoperative period. After a mean follow-up of 13.2±8.9 years, the patients have not presented recurrence of the disease.
Characteristics of Patients With Recurrent Non-Functioning Parathyroid Cysts.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age (yrs) | 43 | 55 | 27 | 26 |
| Sex | Female | Male | Male | Male |
| Symptoms | Asymptomatic | Cervical discomfort when swallowing | Asymptomatic | Cervical discomfort when swallowing |
| Physical examination | Palpable and non-painful left cervical nodule | Palpable and painful left cervical nodule | Palpable and non-painful left cervical nodule | Palpable and painful right cervical nodule |
| Analysis | ||||
| Ca (mg/dL) | 9 | 9.5 | 9.6 | 9 |
| P (mg/dL) | 3.5 | 2.3 | 4.1 | 3.3 |
| PTH (mg/dL) | 24 | 39 | 22 | 11 |
| TSH (IU/mL) | 3.66 | 2.34 | 1.55 | 1.88 |
| T4l (ng/dL) | 1.24 | 1.18 | 1.34 | 1.60 |
| Ultrasound | 4.2cm cyst in the lower pole of the LTL | 4.8cm cyst in the lower pole of the LTL | 4cm cyst in the lower pole of the LTL | 3.4cm cyst in the lower pole of the RTL |
| FNA | ||||
| Cytology | Clear liquid with limited cellularity | Clear liquid with limited cellularity | Clear liquid with limited cellularity | Clear liquid with limited cellularity |
| PTH (pg/mL) | 2001 | 370 | 443 | 400 |
| No. of previous aspirations | 1 | 3 | 1 | 2 |
| Surgery | Yes | Yes | Yes | Yes |
| Resected gland | LIPG | LIPG | LIPG | RIPG |
| Complications | No | No | No | No |
| Histopathology | Parathyroid cyst | Parathyroid cyst | Parathyroid cyst | Parathyroid cyst |
| Follow-up (yrs) | 21 | 20 | 10 | 2 |
| Recurrence | No | No | No | No |
RIPG: right inferior parathyroid gland; LIPG: left inferior parathyroid gland; RTL: right thyroid lobe; LTL: left thyroid lobe; FNA: fine-needle aspiration.
Non-functioning parathyroid cysts are usually asymptomatic,2,5 except those that reach a size greater than 3cm, which tend to cause symptoms due to the compression of neighboring structures.1,2 The initial treatment is percutaneous drainage, which is ambulatory and can resolve the condition in up to 50% of cases, or at least maintain it at a size that does not produce compressive symptoms.6
In cases of cyst recurrence after aspiration with an acquired size greater than 3cm, a more definitive treatment is recommended. Some authors propose further needle-aspirations, but in most cases there are new cyst recurrences.7,8 The most effective treatment is surgery, as it achieves definitive resolution of the cyst. Classically the main reason against surgery was the associated morbidity. Today, however, in experienced endocrine surgery units, this surgery is performed with practically no morbidity,9,10 as observed in our series. Remember that, as it is neither tumor tissue nor functioning, the risk of parathyromatosis in case of rupture of the cyst is virtually non-existent.
In recent years, other non-surgical therapeutic alternatives have been developed and promoted. For instance, radiofrequency has been gaining indications in benign disease, both thyroid and parathyroid, with promising results. However, the experience to recommend its use in parathyroid disease is minimal, especially in cystic lesions where the results are worse than in solid lesions. Sclerosis with tetracycline or ethanol7,11 has been recommended by some authors, and has even been recommended as a second therapeutic step after the failure of percutaneous drainage by needle aspiration. However, parathyroid cysts >3cm, because of their size, are usually close to the recurrent nerve, which is frequently injured. Therefore, our group does not recommend this technique. In any case, we should keep in mind that, given the lack of experience in this disease, recommendations cannot be restrictive.
In conclusion, for the treatment of non-functioning parathyroid cysts refractory to percutaneous needle-aspiration drainage, surgery is a safe and effective therapeutic option in endocrine surgery units.
Please cite this article as: Ruiz J, Ríos A, Rodríguez JM, Parrilla P. Quistes no funcionantes de paratiroides refractarios al tratamiento conservador. Cir Esp. 2018;96:52–54.