A limited number of studies have examined infant crying patterns in less affluent societies, but none of them have been longitudinal in nature. The aim of this study was to describe reported infant crying patterns in a cohort of Mexican infants and examine how these are associated with crying-related maternal expectations, general perceptions and help-seeking behavior.
MethodsObservational cohort study, 204 primiparous mothers and their infants, recruited at birth and visited in their homes at nine different time points from 1 to 24 weeks of infant age.
ResultsMothers reported that their infants cried less than infants in other more affluent societies, although not less frequently. A previously reported evening clustering of crying was present, with a subtle 24-h crying peak emerging around 2 to 4 weeks. Having an expectation of an infant who will be difficult to soothe and/or an increased report of crying frequency were associated with perceptions of maternal anguish, which was associated with maternal concern and help-seeking behaviors related to crying.
ConclusionsSimilarities and differences were found in the crying patterns reported by mothers of Mexican infants and others previously studied. Expectations and reports of crying behavior were associated with maternal perceptions, which may have a role in reducing crying-related anguish and demand on health services.
Observed and/or perceived excessive infant crying has important potential consequences to the health and well-being of parents, infants and their interaction, and places a considerable demand on health services available to parents.1
Whereas a number of studies have contributed to better understanding the normal crying patterns of infants and those whose parents seek help for excessive crying, most have focused on higher-income countries.2–9 Only two studies of crying behavior were identified in Latin America, both of which were cross-sectional in nature and did not provide information on more detailed dimensions of crying behavior, like crying frequency, mean crying bout length or changes in crying behavior over the first 6 months of life.10,11 Nonetheless, a clustering of crying in the evening hours, bouts of inconsolable crying (a feature of excessive crying, also commonly referred to as ‘colic’), and a peak in crying behavior within the first 3 months of life have also been identified in the limited number of studies from low- to mid-income countries.10–15
This scarcity of information on crying patterns in less affluent societies is evident and merits further investigation, especially in light of potentially harmful practices such as the use of traditional remedies for crying which increase the risk of gastrointestinal infections. Maternal reports of ‘too much’ infant crying have also been linked in the literature with perceptions of insufficient breast-milk and consequent early introduction of non-breast milk foods and/or discontinuation of breastfeeding.16–19
The objective of the present study was to characterize the reported crying patterns of a cohort of infants from birth to 6 months in Mexico City, Mexico, as well as to examine maternal expectations and perceptions of these patterns and their impact on help-seeking behavior.
2Methods2.1ParticipantsStudy participants included mothers who delivered at Hospital General de Zona 1-A ‘Venados’ in Mexico City, Mexico. The hospital is part of a health and social benefits insurance system established by the government for Mexican formally employed workers and their direct dependents, and its main users are mid-to-low income working-class families. Selection criteria included being first-time mothers of healthy, full-term infants who planned to breastfeed their child and not return to work until the infant was at least 6 months of age. Ethical approval was obtained from The Johns Hopkins University Committee on Human Research and IMSS National Research Commission.
From March 2000 to July 2002, 475 eligible women agreed to participate in the study. Of these, 129 (27.2%) dropped out after recruitment, 142 (29.9%) were visited one or more times but did not complete the study and 204 (43.0%) were visited at all nine time points. The main reasons for this substantial loss-to-follow-up were the burden of an hour-long interview, the high mobility of the population, and other factors related to the size of the urban environment in which the study was conducted. No significant differences were found in the characteristics of study participants and those lost to follow-up, with the exception of a higher proportion of single women in the lost to follow-up group (9.2% vs. 2.9%). Reported crying patterns and maternal perceptions of these patterns generally did not differ between women with complete or incomplete follow-up neither did maternal expectations of crying behavior or attitudes toward crying and feeding measured at the initial home visit.
2.2ProcedureNinety-five percent of participants were recruited within 3 days of their infant's birth (range: 0–9 days), and written consent and expectations of crying behavior were obtained. Women were then interviewed in their homes when their infants were approximately 1, 2, 4, 6, 8, 12, 16, 20, and 24 weeks of age. More than 90% of women were visited within 5 days of their scheduled visit at each time point. Each mother was interviewed by one of six trained Mexican health professionals using the following questionnaires.
2.3Maternal expectationsMothers were asked to estimate how much time (in minutes) their infants would spend crying and fussing when they were newborns, and at 1, 2, and 6 months, including the time of day when they thought it would be greatest. They were also asked about how much they thought their baby would cry in general as compared to other infants, and how easy it would be to soothe their infant when s/he was crying.
2.4Attitudes toward cryingAttitudes toward crying were measured at the first week visit using an instrument developed through formative qualitative research in the same study population.20 It contained three sections to assess three underlying constructs identified by means of factor analysis, two of which are relevant here: (1) the “Crying as an Infant Signal” section (Babies Cry) with 10 statements, such as: “If the baby doesn’t cry, the mother will not know when the infant needs something”; (2) the “Crying Response and Spoiling the Baby” section (Response to Crying) with 15 statements, such as: “One must let the baby cry out every once in awhile so that s/he will be independent”. Each mother was asked to what extent she agreed with each statement on a scale from 1 to 6 (completely disagree to completely agree). Higher scores indicated a stronger maternal belief that: (1) babies need to cry to make their needs known (Babies Cry) or (2) it is beneficial to promptly respond to infant crying (Response to Crying). Alpha coefficients in this sample of women were 0.74 for the Babies Cry section and 0.77 for the Response to Crying section.
2.5Adapted Crying Patterns Questionnaire (CPQ)Reported crying patterns were assessed at each of the nine visits. The CPQ assesses crying and fussing duration jointly during four defined 6-h periods over a typical day of the past week.21 Time-of-day periods were adapted from previous studies to accommodate linguistic and cultural characteristics of the study population. The periods used were madrugada (night – midnight to 6a.m.), mañana (morning – 6a.m. to noon), medio-día (midday – noon to 4p.m. – the midday meal is typically from 2 to 4p.m.), media tarde (mid-afternoon – 4p.m. to 8p.m.) and noche (evening – 8p.m. to midnight). In the analyses, the media-tarde period was equitably split between the medio-día and noche periods to create an afternoon (noon to 6p.m.) and evening (6p.m. to midnight) period. The times of day used in the analyses were thus equally spaced and comparable to the original CPQ. The original CPQ also included four questions regarding general maternal perception of infant crying behavior (general amount of crying, difficulty of soothing, bother to other household members, and maternal anguish related to crying) as well as a question on how often the mother let her infant self-soothe when crying, which was also used in our study. These were rated by the mothers on a scale from 1 to 6 (low to high).
Data collected in this questionnaire provided the three reported crying pattern variables: crying frequency (number of crying bouts per day), mean crying bout length (average number of minutes per crying bout at each visit) and 24-h crying time (in minutes per day). Due to the skewed nature of the distribution of the crying variables, median and interquartile ranges are reported and nonparametric tests were used to evaluate changes.
2.6Maternal help-seekingAt each of the nine visits, mothers were asked whether any help was sought regarding their infant's crying from family members/friends or other health professionals, and what advice was given. Because the advice often included the recommendation of giving water, tea or formula, actual maternal use of these at 1, 4 and 8 weeks was extracted from feeding questionnaires.
2.7Data analysisGraphical analysis of the data using variograms22 indicated that the closer the spacing of the visits (e.g., 2 and 4 weeks), the more similar the crying reported for a specific infant at these time points, with correlations decreasing as the time between the visits increased (e.g., 2 and 16 weeks). This suggested the data followed a first-order autoregressive correlation structure.22 Therefore, random effects generalized models with an autoregressive disturbance of the first order22 were used to evaluate associations between maternal and infant characteristics and reported patterns and general perceptions of crying behavior, as well as the odds of seeking help or worrying about ‘colic’ or crying behavior. All analyses were performed using Stata version 11.2.23
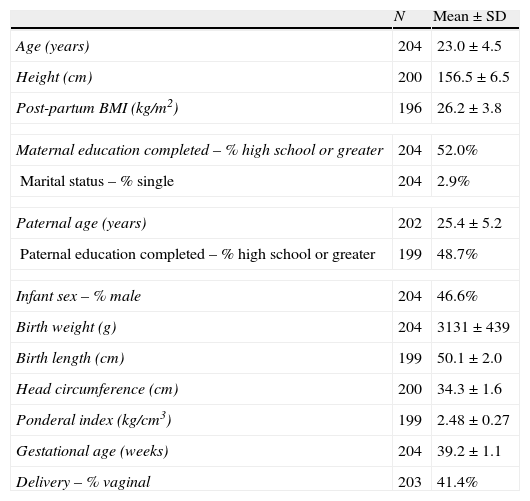
3ResultsMaternal and infant characteristics of our sample population are shown in Table 1. The average age of participating mothers was 23 years (standard deviation ±4.5), with an average height of 156cm (±6.5) and postpartum BMI of 26.2kg/m2 (±3.8). Fifty-two percent (n=106) completed 12 or more years of formal education and only six (2.9%) were single mothers. Our selection criteria included only mothers delivering full-term, singleton infants, resulting in a sample average gestational age of 39.2 weeks (±1.1) and average infant birth weight of 3131g (±439). Forty-seven percent of infants were male (n=95) and less than half were delivered vaginally (41.4%, n=84). This very high rate of caesarean delivery has been previously reported in the literature and is regarded as largely unnecessary and not due to complications during pregnancy or birth.24,25
Maternal and infant characteristics of the final study cohort.
| N | Mean±SD | |
| Age (years) | 204 | 23.0±4.5 |
| Height (cm) | 200 | 156.5±6.5 |
| Post-partum BMI (kg/m2) | 196 | 26.2±3.8 |
| Maternal education completed – % high school or greater | 204 | 52.0% |
| Marital status – % single | 204 | 2.9% |
| Paternal age (years) | 202 | 25.4±5.2 |
| Paternal education completed – % high school or greater | 199 | 48.7% |
| Infant sex – % male | 204 | 46.6% |
| Birth weight (g) | 204 | 3131±439 |
| Birth length (cm) | 199 | 50.1±2.0 |
| Head circumference (cm) | 200 | 34.3±1.6 |
| Ponderal index (kg/cm3) | 199 | 2.48±0.27 |
| Gestational age (weeks) | 204 | 39.2±1.1 |
| Delivery – % vaginal | 203 | 41.4% |
Women in this sample only somewhat agreed that babies need to cry to make their needs known (Babies Cry median score: 64.6%, IQR: 49.0–77.1). There was more agreement that it is beneficial to promptly respond to infant crying (Response to Crying median score: 72.6%, IQR: 65.5, 82.7).
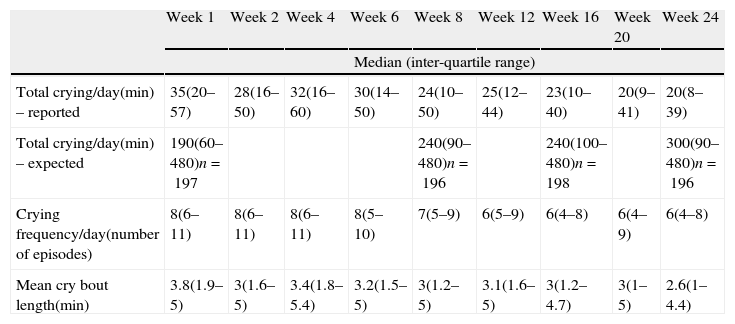
3.2How much infants cry: reported crying patternsTime spent crying over a 24-h period showed a decreasing trend across visits (Table 2). Although maternal expectations were that 144 of 194 (74%) infants would cry over 3h at 1, 8, 16 or 24 weeks, actually only 26 (13%) of the 204 infants were ever reported as having cried over 3h at any visit (also referred to as “persistent” criers). Sixty-six (129/194) percent of mothers expected their infant would cry more than what they actually reported them as crying at the 1- and 16-week visit, while there were significant correlations between expected and reported 24-h crying duration at 8 and 24 weeks. Overall, infants’ crying patterns differed more across visits than across infants, with intraclass correlations (95% confidence intervals) of 0.37 [0.32–0.43] for crying frequency; 0.36 [0.31–0.42] for mean bout length, and 0.27 [0.22–0.33] for 24-h crying.
Median and inter-quartile ranges of crying variables across visits (N=204).
| Week 1 | Week 2 | Week 4 | Week 6 | Week 8 | Week 12 | Week 16 | Week 20 | Week 24 | |
| Median (inter-quartile range) | |||||||||
| Total crying/day(min) – reported | 35(20–57) | 28(16–50) | 32(16–60) | 30(14–50) | 24(10–50) | 25(12–44) | 23(10–40) | 20(9–41) | 20(8–39) |
| Total crying/day(min) – expected | 190(60–480)n=197 | 240(90–480)n=196 | 240(100–480)n=198 | 300(90–480)n=196 | |||||
| Crying frequency/day(number of episodes) | 8(6–11) | 8(6–11) | 8(6–11) | 8(5–10) | 7(5–9) | 6(5–9) | 6(4–8) | 6(4–9) | 6(4–8) |
| Mean cry bout length(min) | 3.8(1.9–5) | 3(1.6–5) | 3.4(1.8–5.4) | 3.2(1.5–5) | 3(1.2–5) | 3.1(1.6–5) | 3(1.2–4.7) | 3(1–5) | 2.6(1–4.4) |
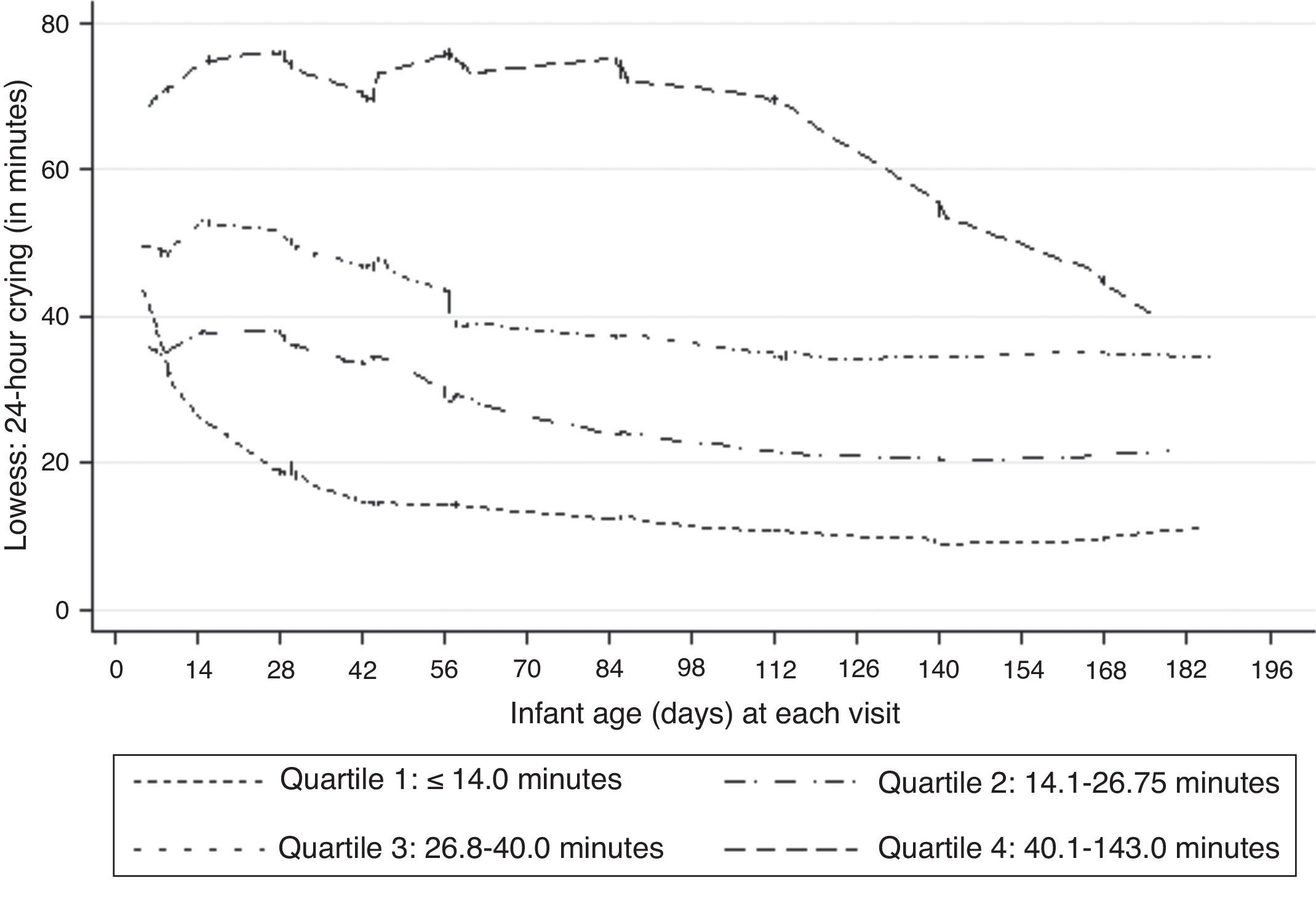
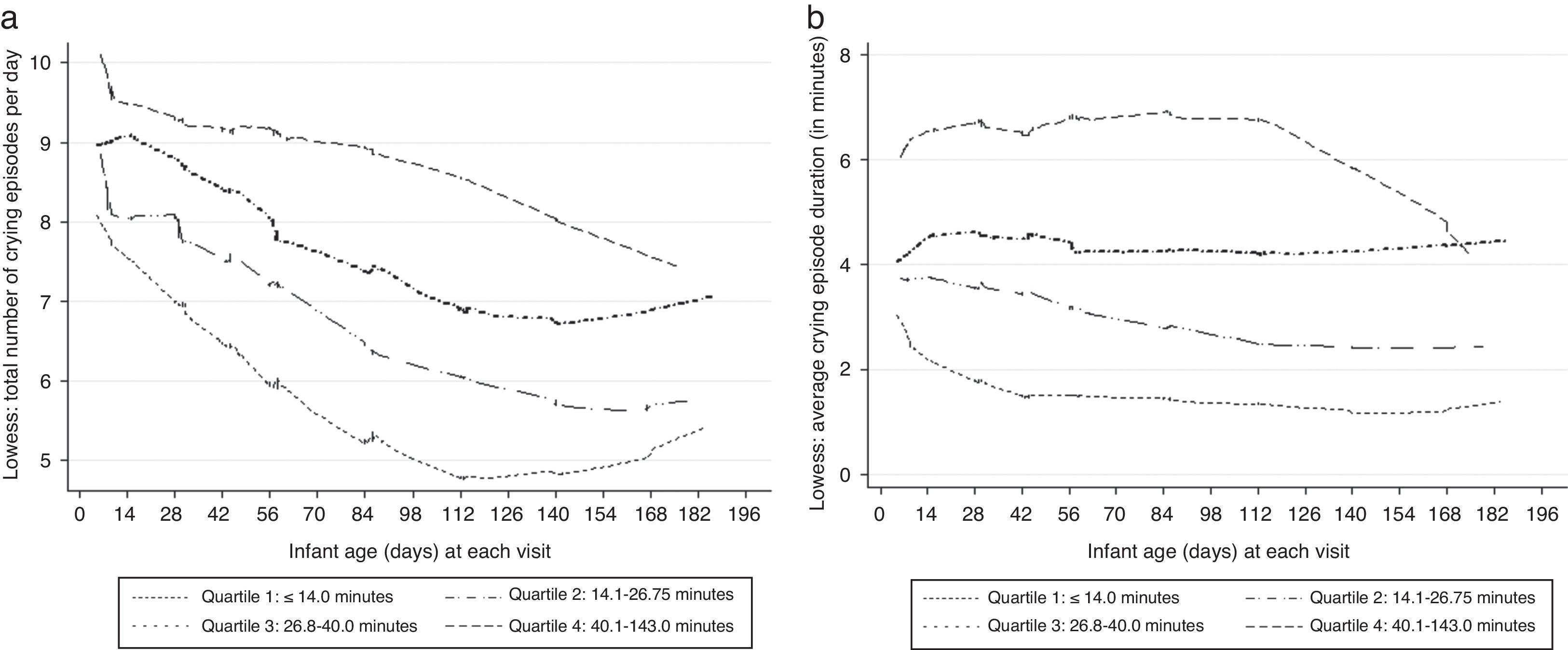
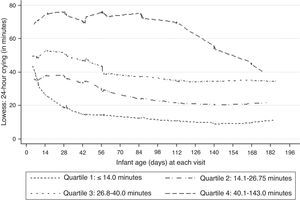
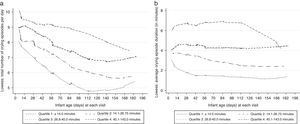
Lowess-smoothed curves were fitted by quartiles of median 24-h crying across the nine visits in Fig. 1 as intermittent lines. Although there was no clear evidence of a peak in the entire sample or in the lowest crying quartile, a subtle peak was evident in the 2- to 4-week period among the remaining quartiles. Lowess-smoothed curves of reported Crying frequency and Mean crying bout length were examined in a similar manner (Fig. 2). A visual examination of the graphs suggested a general decrease in Crying frequency, whereas subtle peaks were also evident in Mean crying bout lengths. According to total crying times predicted by mothers at 1, 8, 16 and 24 weeks, most mothers expected infant crying to peak at 24 weeks (69/194 women or 36%), although 25% of women also expected a peak at week 1 (50/194 or 28%). Interestingly though, a crying peak was actually reported for only 14/50 women who expected it during the first week.
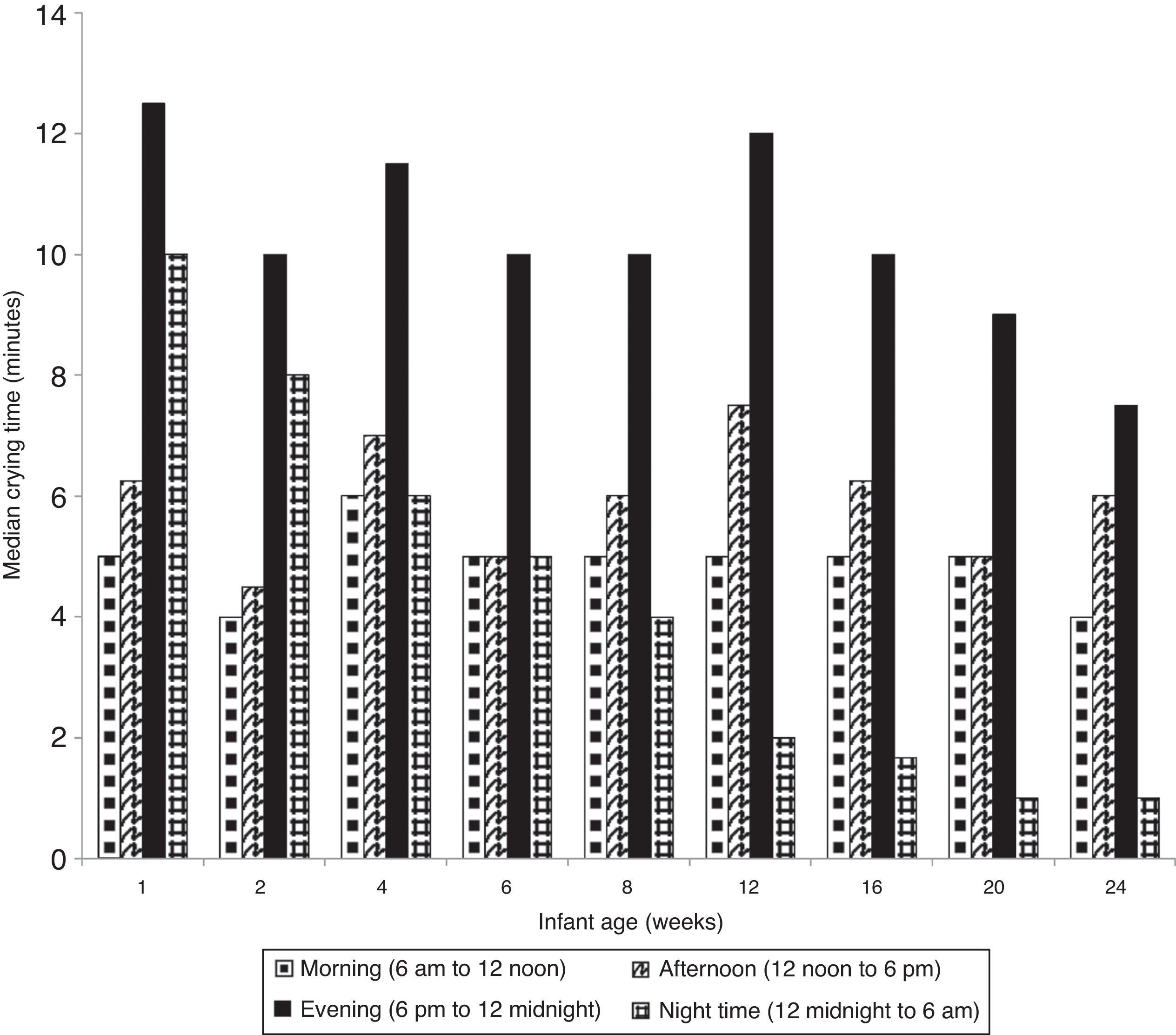
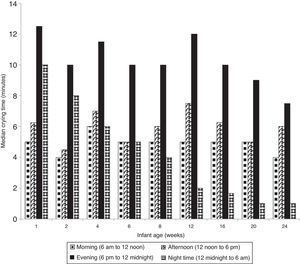
The time of day when median time of infant crying was highest throughout the study period was in the evening (i.e., 6p.m. to midnight) (Fig. 3). Median nighttime (midnight to 6a.m.) crying levels were high during the first 2 weeks of life and decreased over time. A majority of women expected their infant to both fuss (66%) and cry (72%) most in the evening and nighttime periods (6p.m. to 6a.m.).
3.3Maternal expectations of crying patternsIn contrast to the decline in reported crying time, mothers expected infants to cry more as they got older. Sixty-six percent (129/194) of mothers expected their infant would cry more than what they actually reported them as crying at the 1-, 8-, 16- or 24-week visit.
3.4Maternal perceptions of reported crying patternsThe vast majority of mothers did not perceive their infant's reported crying negatively across visits. Only 7–11% of mothers reported that the baby cried “a lot” or “too much” and between 4 and 13% of mothers perceived it to be difficult to soothe their infant when they were crying. Mothers also did not perceive that the crying was a great bother to the family as it was reported from <1 to 3% across visits. In sharp contrast, at 1 week 27% of mothers reported feeling anguish related to their baby crying. There was a pattern of decline with 23–27% of mothers reporting anguish during weeks 1–4 and reports declining from 16% to 10% thereafter.
3.5Maternal help-seekingAlthough 44 to 66% of the women occasionally let their infants self-soothe, very few women reported doing so more often than not, ranging from two to five women in the first 8 weeks (1–2%) and six to 11 women (3–5%) from 12 to 24 weeks.
During the course of the nine visits in the study, the vast majority (89%, 182/204) of women reported seeking help related to their infant's crying behavior, mostly from both family/friends and professionals (48%) as well as family/friends only (37%). Ninety-nine women also provided information on the advice given to them at 1 week, stating crying was mostly attributed to hunger (30%), colic (24%) or normal behavior (18%). At 4 (n=103) and 8 weeks (n=98) the suggestions of colic (34% and 26%, respectively) surpassed those of hunger (17% and 9%) and normal behavior (17% and 12%). Thirty-four women mentioned they received the recommendation to give their infant herbal tea at 1, 4 or 8 weeks, of whom 25 (74%) carried through with the recommendation. All ten women (100%) who were advised by family, friends or health professionals to give their infant formula reported doing so, as did 3/5 women (60%) who were advised to give their infant water.
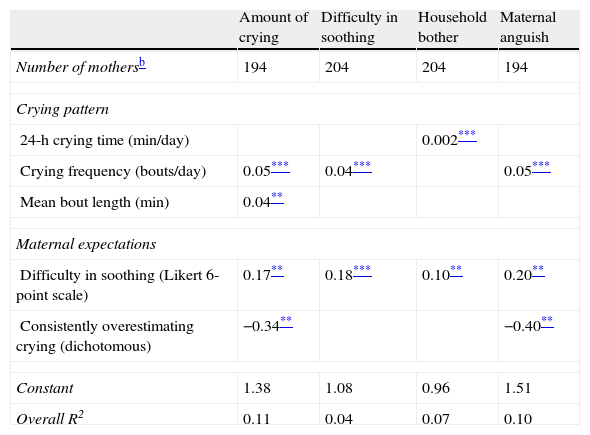
3.6Associations among the variablesMaternal expectations of crying behavior were found to be significantly associated with her perceptions of infant crying behavior. Mothers who expected their infants to be more difficult to soothe at recruitment reported their infants as crying more in general, being more difficult to soothe, being of greater bother to other household members and being more anguished by their infant's crying at all visits. In addition, mothers who reported their infants as crying less than they had expected (at baseline) were less anguished by their infant's crying behavior across all visits. Specific aspects of reported crying patterns (24-h total, crying frequency or mean bout length) were associated with the maternally-reported general perceptions of crying behavior. Although statistically significant, effect sizes were quite small as was the proportion of the variance explained by the models which were fit (Table 3).
Random effects generalized linear models with AR1 disturbance of determinants of general maternal perceptions of crying.a
| Amount of crying | Difficulty in soothing | Household bother | Maternal anguish | |
| Number of mothersb | 194 | 204 | 204 | 194 |
| Crying pattern | ||||
| 24-h crying time (min/day) | 0.002*** | |||
| Crying frequency (bouts/day) | 0.05*** | 0.04*** | 0.05*** | |
| Mean bout length (min) | 0.04** | |||
| Maternal expectations | ||||
| Difficulty in soothing (Likert 6-point scale) | 0.17** | 0.18*** | 0.10** | 0.20** |
| Consistently overestimating crying (dichotomous) | −0.34** | −0.40** | ||
| Constant | 1.38 | 1.08 | 0.96 | 1.51 |
| Overall R2 | 0.11 | 0.04 | 0.07 | 0.10 |
AR1 disturbance: structure in which correlations between a measurement repeated at each visit decreases as the time lag between visits increases. Outcomes are listed in columns. The unit for outcomes is the level of each of the perceptions on 6-point Likert scale ranging from 1 (positive perception response, such as “cries almost not at all”) to 6 (negative perception response, such as “cries too much”). The coefficients represent the effects of the explanatory variables on a particular mother's perceptions of her infant's crying behavior (e.g., the perception of how much anguish a mother reports in relation to her infant's crying with random effect Ui=0 increases in 0.05 points – on a Likert scale from 1 to 6 – for each additional occasion her baby cries holding maternal expectations of difficulty in soothing and maternal expectations of how much her infant will cry constant).
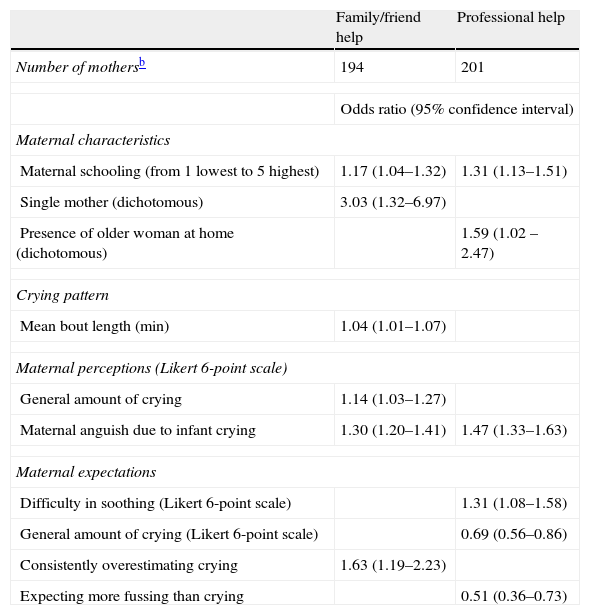
The odds of seeking family/friend or professional help were greater in this sample among women with higher levels of education and among those who reported greater anguish associated with their infant's crying. Other factors were also found to be associated with maternal help-seeking behavior (Table 4).
Population-averaged logistic models with AR1 disturbance of determinants of help-seeking behavior.a
| Family/friend help | Professional help | |
| Number of mothersb | 194 | 201 |
| Odds ratio (95% confidence interval) | ||
| Maternal characteristics | ||
| Maternal schooling (from 1 lowest to 5 highest) | 1.17 (1.04–1.32) | 1.31 (1.13–1.51) |
| Single mother (dichotomous) | 3.03 (1.32–6.97) | |
| Presence of older woman at home (dichotomous) | 1.59 (1.02 –2.47) | |
| Crying pattern | ||
| Mean bout length (min) | 1.04 (1.01–1.07) | |
| Maternal perceptions (Likert 6-point scale) | ||
| General amount of crying | 1.14 (1.03–1.27) | |
| Maternal anguish due to infant crying | 1.30 (1.20–1.41) | 1.47 (1.33–1.63) |
| Maternal expectations | ||
| Difficulty in soothing (Likert 6-point scale) | 1.31 (1.08–1.58) | |
| General amount of crying (Likert 6-point scale) | 0.69 (0.56–0.86) | |
| Consistently overestimating crying | 1.63 (1.19–2.23) | |
| Expecting more fussing than crying | 0.51 (0.36–0.73) | |
Outcomes are listed in columns. Odds ratios are presented, for example the odds of an average mother who is single in this population seeking help related to their infants crying from a friend/family member as compared to an average mother who is not single in this population (OR: 3.03), holding maternal schooling, mean crying bout length, and relevant maternal perceptions and maternal expectations constant.
This study provides a longitudinal picture of maternally reported crying patterns in the first 24 weeks of life in Mexico, the first in a setting other than a high-income country. Among the salient findings of this study are the associations between maternal expectations of crying behavior in relation to later reports, perceptions and behaviors including the elevated levels of crying-related anguish and consequent advice-seeking, despite general perceptions of lower-than-average crying behavior.
These infants were reported as crying less than those in higher-income countries.4–7,9,21,26-28 In comparison with the cross-sectional data available from other mid- to low-income countries,10,12,14,15 reported crying levels were somewhere in the middle. Although crying frequency tends to be similar across settings, shorter crying bouts have been reported and observed in settings where an “infant-demand” approach to caregiving is adopted (i.e., infants are carried for longer periods of time by their mothers, infant cries are responded to promptly, and infants are frequently breastfed), such as in many low- to mid-income countries9,10,12,14 or among select groups of parents in higher-income countries.8 The care-giving practices reported by the urban Mexican women in this sample tended to be less in line with the “infant-demand” approach, with greater similarities to the “scheduled” approach (less physical contact, letting the baby cry out, earlier abandonment of breastfeeding) adopted by most women in high-income settings, probably as a result of a busy, urban lifestyle characteristic of Mexico City. Full breastfeeding rates (i.e., no bottle feeding) among Mexican women at 2, 6 and 12 weeks (78, 67 and 47%) were very similar to those reported in London (73, 57 and 45%) as were the percentages of women reporting letting their baby cry out at these ages (49, 56 and 59% of Mexican mothers vs. 38, 57 and 58% of London mothers).12 It must be noted that whereas the majority of Mexican mothers did report occasionally allowing their baby to cry out, 37–54% reported it seldom occurred. Nonetheless, reported crying frequencies in this Mexican sample were also similar to those from other studies, whereas reported mean crying bout length was lower.4,29 Although it is possible that the choice of method (i.e., our use of the adapted CPQ rather than crying diaries) may have also affected the numbers obtained, the same results were evident when considering only CPQ-based studies in high-income countries.9,12
A number of previously published studies have shown a crying peak at ∼ 6 weeks of infant age.2,7,8,12 Others have found a progressive decline in overall crying from birth.4,6,7,30,31 Our sample tended to follow the progressive decline pattern in crying with age, consistent with the commonly observed clustering of crying behavior within the first 3 months of life31 and the evening clustering of crying,4,6–8 underscoring similarities in reported crying patterns across different settings. Thus, although it may be expected that different forms of care may be associated with different levels of overall crying, objective assessments of crying measures from different cultures also suggest a degree of similarity, highlighting the effect of cultural views on differing reports and perceptions.
Mothers in our study who expected their infants to cry a lot and were pleasantly surprised when it was not so bad reported significantly lower levels of maternal anguish. However, those who expected it to be more difficult to soothe their infants reported significantly higher levels of maternal anguish, even if their infants were not as difficult to soothe as they had expected. Increased anguish was also associated with significantly greater odds of seeking help for their infants’ crying behavior. This suggests that providing new mothers with reassurance and a wider array of coping strategies to soothe their infants, especially among those who expect this will be challenging for them, has the potential of translating into less burden on health services available to parents and more rewarding interactions for mothers and infants alike.
Anguish was also found to be most closely associated with crying frequency as opposed to other dimensions of crying (total time or bout length). Other studies in Mexico have found that women interpret increased crying frequency as hunger, leading to perceptions of insufficient milk.16–18,32,33 Indeed, in our formative research we found that infant crying was associated with the perception of insufficient breast-milk and the early abandonment of breastfeeding.34
Nearly all women in this sample reported seeking help related to their infant's crying during the 6-month follow-up. Although some were reassured this was normal behavior, the greatest proportion of these were told it was due to hunger or colic in the first 8 weeks of life, both of which are very valid reasons for crying, among many others. However, the main advice given was to provide the infant with herbal tea, formula or water, and this was adopted by women more often than not.
Several limitations are worth noting. First, we relied on maternal reports of infant crying behavior rather than on an objective measure of infant crying behavior. This responded, however, to the fact that we were not set to determine how much infants actually cried because the main focus of this study was to examine maternal perspectives themselves (including patterns and perceptions) as well as help-seeking and other behavioral responses related to infant crying. We also experienced a larger than expected lost to follow-up. Although we did not find differences between women who completed the study and those lost to follow-up, different findings could have emerged had they remained in the study.
Despite these limitations, the study adds important information to the literature on infant crying, especially in low- to mid-income countries. It provides a more complete picture of changing crying patterns in the first 6 months of life and underscores similarities and differences in reported crying patterns across different settings. Insights into the potential role of maternal expectations of the difficulty in soothing their crying infant and how they may relate to anguish and consequent help-seeking behavior contribute to the array of anticipatory guidance that may be helpful to new mothers in better responding to their infant's behavior. Providing new mothers with reassurance and a wider array of coping strategies to soothe their infants, especially among those who expect this will be challenging for them, has the potential of translating into less burden on health services available to parents and more rewarding interactions for mothers and infants alike.
Despite these limitations, this study adds significantly to the available body of crying-related literature in low- to mid-income countries due to its longitudinal nature and the limited cross-sectional snapshots provided by a handful of other studies. Considered in the wider array of publications available from higher income countries, the contribution of this study is marked by the unprecedented frequency of reports of crying behavior across different infant ages and the glimpses provided into the potential effects of maternal expectations and reports on later help-seeking behavior.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis study was supported by the Nestlé Foundation in Lausanne, Switzerland.
Conflict of interestThe authors declare no conflict of interest.
We gratefully acknowledge the contributions of Silvia Nájera Cruz, Filiberto Gómez Mejía, Adrián Alcántara Bautista, Sergio Flores Hernández, Bernardo Turnbull and all the mothers and infants who took part in the study.