Primary care guidelines recommend the utilisation of low-dose β-lactams, mainly penicillin V, in patients non allergic to penicillin's with suspected bacterial pharyngitis.1 Group A β-haemolytic streptococcus (GABHS), which causes 10–15% of all the episodes of pharyngitis in adults, is universally susceptible to penicillin and no meaningful differences have been observed among the different antibiotic choices for this condition.2 Over the last years an increase of the defined daily doses of antibiotics per 1000 inhabitants and day has been observed in Spain, with a sharp increase in 2013.3 This study was aimed to know general practitioners’ (GP) attitudes about management of streptococcal sore throat in Spain. A cross-sectional survey among a sample of the Spanish GPs was conducted over a 3-month period, from July to September 2013, using an internet-based survey. Participants were able to respond the questionnaire only once. The inquiry was available online in the semFYC website (semfyc; www.semfyc.es). All respondent answers were automatically entered into a data file which was checked for accuracy by two independent researchers. Descriptive analysis was carried out.
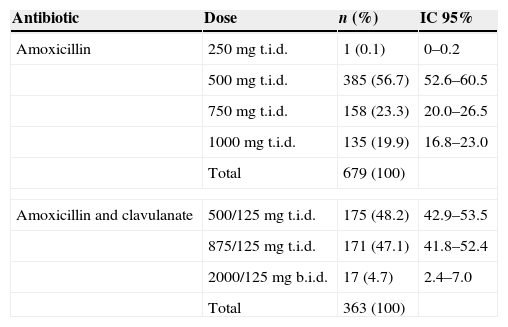
A total of 1239 GPs completed the questionnaire. In suspected streptococcal pharyngitis, 152 GPs considered penicillin as the first-choice antibiotic (12.3%). The antibiotic most commonly mentioned as being prescribed by Spanish GPs for patients with sore throat was amoxicillin (679 cases, 54.8%), followed by amoxicillin+clavulanate (363 cases, 29.3%). The recommended doses of β-lactams were stated by 724 GPs (58.4%) while the remaining 41.6% of GPs declared to use higher doses of antibiotics (more than 500mg for amoxicillin and amoxicillin and clavulanate thrice daily and more than 600mg for penicillin V twice daily) for the treatment of suspected streptococcal pharyngitis (Table 1).
Doses of amoxicillin and amoxicillin and clavulanate declared to be used by the respondents when treating patients with suspected bacterial sore throat.
| Antibiotic | Dose | n (%) | IC 95% |
|---|---|---|---|
| Amoxicillin | 250mg t.i.d. | 1 (0.1) | 0–0.2 |
| 500mg t.i.d. | 385 (56.7) | 52.6–60.5 | |
| 750mg t.i.d. | 158 (23.3) | 20.0–26.5 | |
| 1000mg t.i.d. | 135 (19.9) | 16.8–23.0 | |
| Total | 679 (100) | ||
| Amoxicillin and clavulanate | 500/125mg t.i.d. | 175 (48.2) | 42.9–53.5 |
| 875/125mg t.i.d. | 171 (47.1) | 41.8–52.4 | |
| 2000/125mg b.i.d. | 17 (4.7) | 2.4–7.0 | |
| Total | 363 (100) | ||
b.i.d., twice daily; t.i.d., thrice daily.
It is remarkable that despite the fact that GABHS remains universally susceptible to penicillin this antibiotic was only preferred by 12% of the GPs, and nearly 30% reported using amoxicillin and clavulanate. It is also surprising that high doses of β-lactams are preferred by four out of ten GPs for the treatment of suspected streptococcal pharyngitis. Advantages of using electronic surveys are their relative ease of implementation, and the potential to conduct large-scale surveys whilst eliminating the costs of postage and administration.4 However, this internet-based questionnaire may have introduced selection bias, as only internet users were invited to participate in the study. Another difference is the gap between opinion and actual practice. This was a study of opinions which therefore does not necessarily reflect what is in fact prescribed in primary healthcare consultations. One strength of this survey, however, is the fact that this is one of the largest studies on public views of management of sore throat. The preference for higher doses of β-lactams might be due to the fact that high doses have been recommended in the last decade in an attempt to empirically cover penicillin-intermediate strains of common community-acquired respiratory germs, such as Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in mainly lower respiratory tract infections but also in rhinosinusitis and otitis media.5 However, the role of these germs in sore throat is negligible and the antibiotic treatment should be targeted to treat the infection caused by GABHS, which is absolutely susceptible to even low doses of β-lactams.6 In addition, current guidelines recommend these antibiotics to be given twice daily instead of the common thrice-daily regimens and even some authors back up the only-daily use of β-lactams for patients with streptococcal pharyngitis.7 Therefore, the use of high doses of antibiotics is not justified for patients with sore throat.
FundingThis study was funded by Reckitt Benckiser. The funding source has not influenced the study design, the writing of the manuscript, or the decision to submit the manuscript for publication. No ethical approval was required for this questionnaire study.
Conflicts of interestDr Llor reports having a grant from the Fundació Jordi Gol i Gurina for a research stage at the University of Cardiff in 2013. He also reports receiving research grants from the European Commission (Sixth and Seventh Programme Frameworks), Catalan Society of Family Medicine, and Instituto de Salud Carlos III (Spanish Ministry of Health). The other authors report no conflicts of interest.
To all the GPs who voluntarily participated in this study.