The history of proprotein convertase subtilisin/kexin type 9 (PCSK9) in medical science is fascinating and the evolution of knowledge of its function has resulted in new medications of major importance for the cardiovascular (CV) patient. PCSK9 functions as a negative control or feedback for the cell surface receptors for low-density lipoprotein including its component of cholesterol (LDL-C). The initial and key findings were that different abnormalities of PCSK9 can result in an increase or a decrease of LDL-C because of more or less suppression of cell surface receptors. These observations gave hints and awoke interest that it might be possible to prepare monoclonal antibodies to PCSK9 and decrease its activity, after which there should be more active LDL-C cell receptors. The rest is a fascinating story that currently has resulted in two PCSK9 inhibitors, alirocumab and evolocumab, which, on average, decrease LDL-C approximately 50%. Nevertheless, if there are no contraindications, statins remain the standard of prevention for the high-risk CV patient and this includes both secondary and primary prevention. The new inhibitors are for the patient that does not attain the desired target for LDL-C reduction while taking a maximum statin dose or who does not tolerate any statin dose whatsoever. Atherosclerosis can be considered a metabolic disease and the clinician needs to realize this and think more and more of CV prevention. These inhibitors can contribute to both the stabilization and regression of atherosclerotic plaques and thereby avoid or delay major adverse cardiac events. (United States)
La historia de la proproteína convertasa subtilisin/kexin tipo 9 (PCSK9) es fascinante y la evolución del conocimiento de su función ha resultado en nuevos fármacos de gran importancia para el paciente cardiovascular. La PCSK9 funciona como un control negativo de receptores en la superficie de células para la lipoproteína de baja densidad con su componente de colesterol (LDL-C). El hallazgo inicial y clave fue que anormalidades diferentes de la PCSK9 resultan en un aumento o una disminución de la LDL-C, relacionados en una mayor o menor supresión de los receptores. Fueron estas observaciones las que proporcionaron evidencias indirectas a la idea de preparar anticuerpos monoclonales de la PCSK9 que pudieran disminuir su actividad y que esto se reflejara en receptores más activos para disminuir la LDL-C. El resto es una historia fascinante que ahora ofrece 2 inhibidores de la PCSK9, alirocumab y evolocumab, los cuales disminuyen la LDL-C en un 50%. Sin embargo, si no hay una contraindicación, las estatinas son el estándar de prevención para el paciente cardiovascular de alto riesgo e incluyen la prevención secundaria y primaria. Estos nuevos inhibidores están indicados en aquel paciente en el que no se obtiene el objetivo de tratamiento con la dosis máxima de una estatina o que no tolera ninguna de ellas. Debemos pensar en la aterosclerosis como una enfermedad metabólica y el clínico necesita darse cuenta de esta realidad y considerar las posibilidades disponibles para la prevención cardiovascular. Estos inhibidores pueden contribuir a la estabilización y regresión de placas ateroscleróticas y evitar episodios cardiovasculares mayores. (Estados Unidos)
There is much controversy related to the relatively new 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guideline and its acceptance. The new ACC/AHA guideline was released and published in 2013 and it subsequently has generated much debate.1 The principal goal of the 2013 guideline is the administration of a high statin dose in a patient with high cardiovascular (CV) risk without specifying a target level for lowering the low-density lipoprotein cholesterol (LDL-C).1 The lack of a specific recommended LDL-C level to attain is considered a problem by many clinicians. Unfortunately, an additional problem associated with the ACC/AHA guideline is the report of a conflict of interest involving more than 50% of the committee charged with preparing the guideline.2 Another recent controversy not limited to the ACC/AHA guideline is whether or not there should be a specific target for LDL-C in the CV patient. In 2012, Hayward y Krumholz published a commentary which stated that there existed no reason to have a specific LDL-C target and that it was better to focus on a tailored approach for the high-risk CV patient without a specific LDL-C target.3 Therefore, regarding the 2013 ACC/AHA guideline and the question of a LDL-C target, there is much evidence in favor of obtaining a very low LDL-C level in the patient with very high CV risk.4 It appears that it would be much better to recognize that each patient represents an individual problem and that this problem warrants a very low LDL-C level specifically selected with a target related to the CV risk and the LDL-C level at the onset of clinical management. There would thus be an initial tailored approach with selection of a LDL-C target. Therefore, the new inhibitors of proprotein convertase (PC) subtilisin/kexin type 9 (PCSK9), for the high-risk CV patient that does not attain an appropriate LDL-C target while taking a maximum statin dose or who cannot take any statin in any dose, offer a new outstanding option for CV disease prevention.
Function of PCSK9Mechanism of PCSK9 for controlling the cellular receptors of LDL-COf the mechanisms associated with various new medications available to decrease LDL-C, the function of the proprotein PCSK9 is of overwhelming importance. A proprotein is the precursor for a protein with a specific function and a PC is an enzyme that converts a proprotein to its active protein form. There is a family of PCs and PCSK9 is a member of that family. PCSK9 has only one substrate which is itself since the PC is a part of the proprotein molecule and its function is to convert the proprotein to its active protein form.5 This active protein plays a role in forming a bond with cellular receptors for LDL-C followed by degradation of the LDL-C.6,7 Therefore, in the situation of normal metabolism, PCSK9 functions as a negative feedback that decreases the activity of LDL-C receptors, which results in increased LDL-C.
Indications of posible clinical harm or benefit from altered PCSK9The indications for possible value and relevance of PCSK9 in clinical medicine derived from studies of mutations of the proprotein. Genetic studies and observations of increased PCSK9 function, especially those association with familial hypercholesterolemia, demonstrated an increase in plasma cholesterol.8 On the other hand, observations of a loss of PCSK9 function demonstrated decreases in the level of LDL-C.8 Therefore, there occurred a resultant interest in the possibility of utilizing a deactivation of PCSK9 by monoclonal antibodies as a new medication and treatment for hypercholesterolemia with the result of decreasing the total cholesterol and LDL-C by binding PCSK9 and thereby eliminating its negative feedback on the LDL-C cellular receptors that are key in LDL-C metabolism.
PCSK9 inhibitors as monoclonal antibodiesPCSK9 inhibitors are actually human monoclonal antibodies obtained from cell cultures. These antibodies have a high specificity for their PCSK9 target. In addition, the risk for negative interactions is very low and it is possible to administer these antibodies via a subcutaneous route during time intervals of up to one month.9 These medications represent a new category of medicine for CV disease prevention at which time other monoclonal antibody medications are being developed. An example of this as a completely different focus relates to inflammation as a critical factor in the development of atherosclerotic plaques and the possibility of inhibiting various steps in the development of inflammation as another entirely different mechanism of possible benefit in CV disease prevention.9 An instance of this is canakinumab, another monoclonal antibody, which is specific for interleukin-1β. This monoclonal antibody already has approval for the treatment of juvenile arthritis and an outcomes study has been started to evaluate the possible benefit in patients with acute coronary syndrome (ACS) and its association with inflammation.9
The concept of decreasing LDL-CExtent of LDL-C reductionThe amount of LDL-C reduction that should be achieved for primary or secondary CV disease prevention remains unresolved. There is an extensive documentation of medical evidence that a lower LDL-C level is associated with decreased CV risk. This began with the Lipid Research Clinics study, published in 1984, which established the lipid hypothesis.10 Subsequently, the Program on the Surgical Control of the Hyperlipidemias (POSCH) study, which utilized a surgical ileal bypass to decrease LDL-C an average of 38%, resulted in a significant reduction in major adverse cardiac events (MACE) from what is a pure play in LDL-C reduction,11,12 as was also the case with the LRC study that used cholestyramine as its LDL-C lowering medication.10 The LRC and POSCH studies were lacking in the advantage of the significant pleiotropic effects of statins. One study of ACS patients demonstrated less MACE with the groups that had LDL-C <40mg/dL and LDL-C 40–60mg/dL.13 In another ACS study, the group of patients with LDL-C <50mg/dL also had fewer MACE.14 Patients with hypobetalipoproteinemia have less coronary artery disease (CAD)15 and there is epidemiologic evidence of a straight-line decrease in CAD risk down to a LDL-C level of 40mg/dL.16 It is not known if there is a specific LDL-C value below which the level is problematic but there is evidence that a level of 25mg/dL is sufficient for cholesterol metabolism in the human body17 and a newborn baby has a LDL-C level of approximately 30mg/dL.17 Therefore, it appears that for the high-risk CV patient, there is evidence for “the lower the better” regarding the LDL-C.
Statins as still the major medical treatment for decreasing CV riskIn association with lifestyle changes, the medical treatment of the patient with high CV risk should always begin with a statin as the gold standard. In support of this, there are multiple outcomes studies of beneficial results using statins.18–20 There are two relevant factors regarding statins which are their effectiveness in decreasing the LDL-C and, in addition, their beneficial pleiotropic effects.21 In relation to this article about PCSK9 inhibitors, although not apparently a significant problem, it is necessary to mention that statins can cause an increase in PCSK9 with a resultant decrease in the LDL-C receptors on the surface of cells.22 It can be postulated that the increase in PCSK9 is an attempt at control with negative feedback following the increase in LDL-C receptors after administration of a statin. Fortunately, the increase in PCSK9 is only about 14% after starting a statin23 and a statin is always appropriate with a PCSK9 inhibitor if there is no problem on the part of the patient in tolerating one. On the other hand, fenofibrate increases PCSK9 more (up to 26%) and this is possibly one reason that this medication is not more effective in reducing LDL-C.23 It appear best to avoid the use of fenofibrate in conjunction with PCSK9 inhibitors.22,24
Other medications aside from a statinIt now appears that there is evidence to support that when a desired LDC-C target is not attained, whatever medication that might contribute to decreasing the LDL-C may offer benefit in reducing CV risk.16 Previously, there were some misgivings about the value of ezetimibe25 but not now. With new evidence-based medicine results, it appears that the value of ezetimibe is no longer in doubt. Therefore, in addition to contributing significantly to LDL-C reduction, there is now good clinical evidence that ezetimibe decreases CV risk.26–28
Results of clinical studies with PCSK9 inhibitorsReduction of LDL-CIn a meta-analysis of 17 randomized controlled studies with 13,083 patients, of which 8250 received a PCSK9 inhibitor, Lipinski et al. found an overall decrease in the LDL-C of 57%.29 Various studies have reported that for alirocumab, there is a decrease in LDL-C of 39–62% and for evolocumab, a decrease in the LDL-C of 47–56%30 In general, in relation to these two inhibitors of PCSK9, it is appropriate to think in terms of a 50% decrease of LDL-C in controlled studies,31 and even up to a 60% reduction.32 In spite of the fact that some academicians want to eliminate LDL-C as a target for decreasing CV risk,3 the reality is that LDL-C is one of the best validated targets in clinical medicine with randomized studies that demonstrate a relationship between the reduction of LDL-C with a decrease in CV risk. The use of PCSK9 inhibitors should help clarify further the efficacy and safety of attaining a low LDL-C level in the management of the patient at high CV risk.33 In the case of patients that are homocygotic for familial hypercholesterolemia, with two matched allelomorphic genes, these monoclonal antibodies to PCSK9 essentially fail to decrease LDL-C because there are not sufficient cellular LDL-C receptors that can be activated by PCSK9 inhibition.31 On the other hand, there is benefit in reducing LDL-C in familial cases in which a cellular receptor is available to be activated. For now, the only PCSK9 inhibitors available for clinical use are alirocumab and evolocumay but more PCSK9 inhibitors are under development and in clinical trials.
Clinical outcomes studiesIn their meta-analysis, Lipinski et al. found a significant decrease of all-cause mortality in patients administered a PCSK9 inhibitor.29 In a summary of the “The Long-term Safety and Tolerability of Alirocumab in High Cardiovascular Risk Patients with Hypercholesterolemia Not Adequately controlled with Their Lipid Modifying Therapy” (ODYSSEY LONG TERM) study (with alirocumab) and “Open-Label Study of Long-term Evaluation Against LDL-C” (OSLER) study (with evolocumab), Hassan showed that, on average, the two studies resulted in a decrease in CV events of 48–53% after prescription of a PCSK9 inhibitor in addition to a statin.32 The beneficial results of these two PCSK9 inhibitors in improving CV outcomes are evident but it is essential to have future clinical outcomes studies that are larger and that are carried out over a longer period of time.32
Costs and approvals for PCSK9 inhibitors (Table 1)A problem very relevant to the clinical use of PCSK9 inhibitors is their cost. A published price for alirocumab is 14,600 United States dollars per year,34 and in perusing the internet, the price for evolocumab is very similar. The secret to obtaining approval for these expensive medications is first and foremost, a carefully documented justification. There are two easily justifiable reasons for the use of these medications. The first is secondary CV disease prevention for the patient with established CAD or the patient with proven peripheral arterial disease, when an appropriate target for LDL-C is not attained while taking a maximum statin dose. The second is for similar patients needing secondary CV disease prevention, who cannot tolerate any statin in any dose. In addition, obtaining approval for primary CV disease prevention for the patient who never has had MACE or other clinical evidence of CV disease is feasible with careful documentation of very high CV risk. If we take into account a negotiated discount of 25%, a saving of 600 United States dollars each year for decreased CV events, and if 5% of the estimated 27% of adults in the United States in the age range of 40–64 with elevated cholesterol levels were eligible for a PCSK9 inhibitor, an increase of 124 United States dollars would be necessary in the annual premiums of medical insurance policies.35
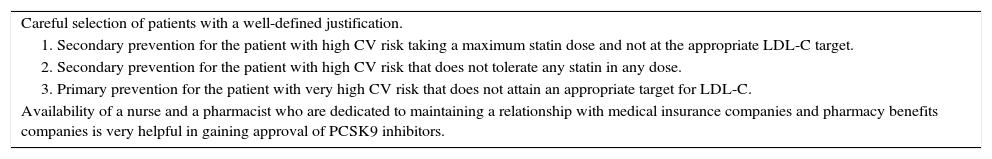
Suggestions to facilitate the approval of a PCSK9 inhibitor.
| Careful selection of patients with a well-defined justification. |
| 1. Secondary prevention for the patient with high CV risk taking a maximum statin dose and not at the appropriate LDL-C target. |
| 2. Secondary prevention for the patient with high CV risk that does not tolerate any statin in any dose. |
| 3. Primary prevention for the patient with very high CV risk that does not attain an appropriate target for LDL-C. |
| Availability of a nurse and a pharmacist who are dedicated to maintaining a relationship with medical insurance companies and pharmacy benefits companies is very helpful in gaining approval of PCSK9 inhibitors. |
A key factor for an ambulatory clinic prescribing PCSK9 inhibitors, based on a personal experience with over 70 patients (from the consultative practice of Thomas F. Whayne, Jr, MD, PhD) is to have a nurse and pharmacist (PharmD in our clinic) dedicated to working with and having relationships with medical insurance companies and pharmacy benefits companies. He or she can manage the required paperwork, know how to justify the prescription, maintain personal contacts with the companies, and learn the system, all of which facilitate incredibly the approval of such important but expensive medications
Secondary effects of PCSK9 inhibitorsA secondary effect to be aware of regarding PCSK9 inhibitors is the controlling effect of PCSK9 on the receptor “Cluster of Differentiation” 36 (CD36), which is present especially in the liver and adipose tissue. Without the controlling effects of PCSK9 on CD36, increased accumulation of lipids occurs in the liver and there is also a resultant increase in adipose tissue.36 The possibility of alterations in this fat metabolism by PCSK9 inhibitors has to be considered. Nevertheless, up to this time, there is no evidence that PCSK9 inhibitors, as monoclonal antibodies, have caused any problem in liver function, glucose metabolism, or adipose tissue in humans.
Safety of PCSK9 inhibitorsIn a meta-analysis of 25 randomized trials, Zhang et al. found that alirocumab and evolocumab were safe and well-tolerated from the point of view of what the authors called “most-tolerated analyses”, with more than a 50% decrease in LDL-C for both monoclonal antibodies, both of which were safe and well-tolerated.37 In a clinical study with evolocumab, it was necessary to stop the placebo in 2.2% of cases and to stop evolocumab in 1.9% of cases38 In another meta-analysis of 20 randomized trials of PCSK9 inhibitors, Li et al. did not find any serious adverse event related to PCSK9 inhibitors and there was no significant difference between placebo and medication with essentially the same chance of needing to terminate the placebo as the PCSK9 inhibitor (risk ratio [RR] 1.07, confidence interval [CI]: 0.86–1.34).39 In general, the major concern with PCSK9 inhibitors regarding safety has been a change in cognition, which has been shown not to have any significant associated risk40 and there is even some evidence of a possible decrease in dementia associated with PCSK9 inhibiors.41
Consideration of use of PCSK9 inhibitors in ACSProbably, hospital administrators have hoped to leave the use of PCSK9 inhibitors to the ambulatory clinic and avoid the disagreeable subject of the cost of these medications. Unfortunately for these executives, there is now some evidence, although not yet well-established, of a benefit of PCSK9 inhibitors in ACS. In a recent review, Navarese et al. commented that PCSK9 levels are increased in ACS, which then contribute to an inflammatory state.42 PCSK9 inhibitors have an anti-inflammatory benefit and in addition, have an inhibitory effect on platelet aggregation.42 It is possible that such results may have a direct beneficial effect in stabilizing a vulnerable atherosclerotic plaque involved in ACS. For now, more studies are necessary to establish and justify the acute use of PCSK9 inhibitors in the hospital. However, there is a basis of information to justify such clinical trials.
Should PCSK9 inhibitors replace statins?The answer to this question is absolutely no with respect to replacement. In general, PCSK9 inhibitors should be used as an additional means to attain a “target”43 LDL-C level that has been “tailored”43 as appropriate to the individual patient. PCSK9 inhibitors offer a reinforcement to statins for secondary prevention in the high CV risk patient and for primary prevention in the very high CV risk patient. In both such patients, initial treatment should begin with a statin. The role of the new PCSK9 inhibitors is decrease the LDL-C further when an appropriate target is not attained with a maximum statin dose or when the high-risk patient cannot tolerate any statin at any dose. PCSK9 inhibitors should only be used to replace statins in cases of complete statin intolerance.
ConclusionsPCSK9 inhibitors represent a major contribution to CV disease prevention, both secondary and primary. The clinician should always begin medical management for prevention with a statin unless there is a good reason not to do so. The purpose of these new monoclonal antibody inhibitors is as a complement to statins to facilitate attaining a desired target LDL-C level in the high-risk CV patient on a maximum statin dose or to achieve the same goal in the patient completely intolerant of statins even when administered in a low dose. Replacement of statins should only occur when a statin cannot be administered. These novel new monoclonal antibodies appear to be very safe, to not have any significant associated problems up to this point in their history, and will undoubtedly contribute to the improvement and prolongation of life when used appropriately and intelligently.
FundingThe author confirms that no financial support was received for the research or writing of this article.
Conflict of interestThe author has no conflicts of interest whatsoever to declare with any pharmaceutical or medical device Company.
The author thanks Abraham Prades-Mengibar, Spanish PhD Candidate, for his excellent editorial critique of the initial Spanish version including the Spanish abstract.