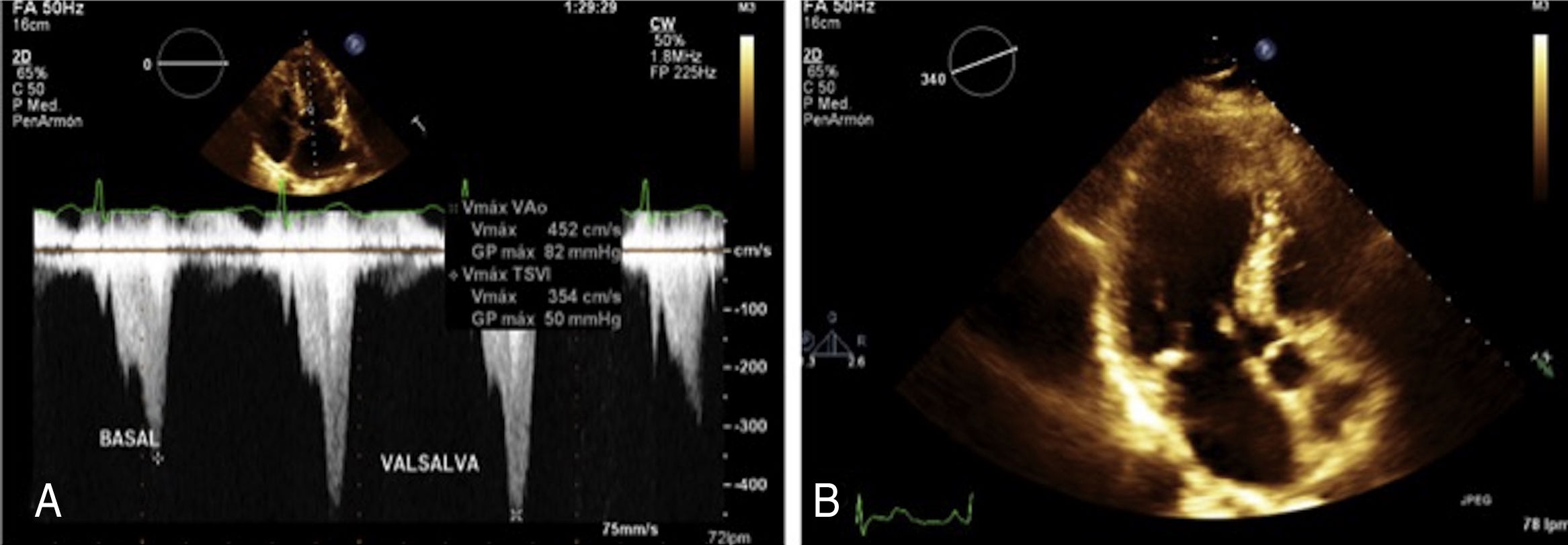
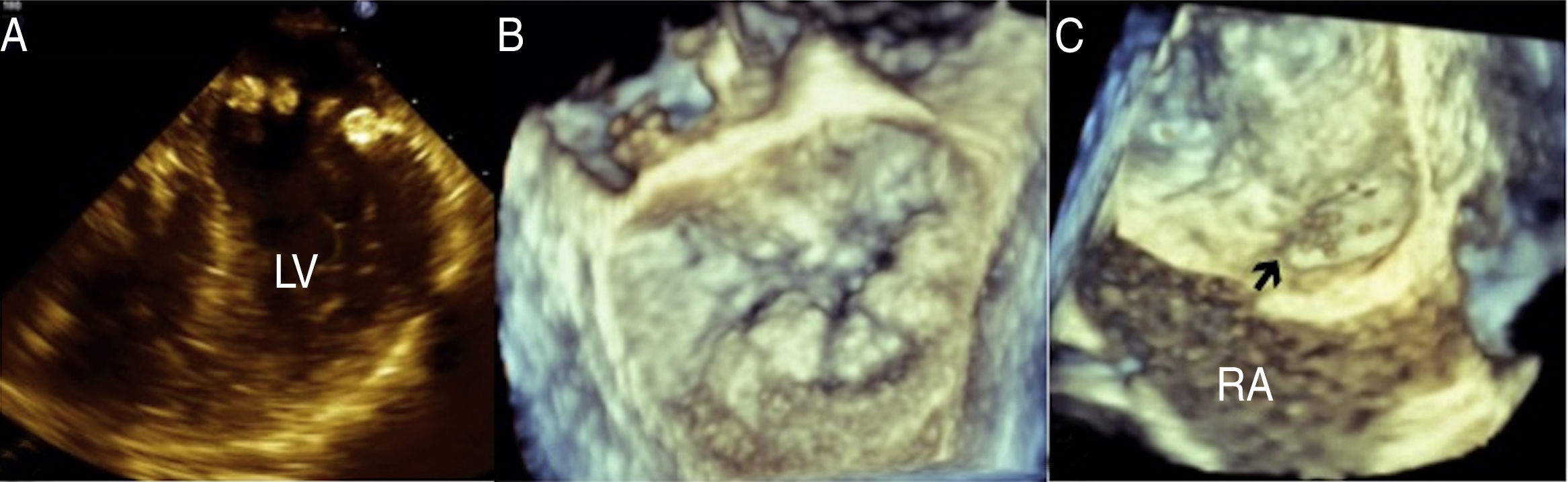
Sixty-six year-old woman with systemic hypertension treated with irbesartan. Her sister had history of patent foramen ovale (PFO). In 2008 she began with lipothymia associated with moderate physical effort, palpitations and exertional dyspnea. She denies migraine or headache. On physical examination a harsch diamond shaped systolic murmur was heard, which becomes quite loud with Valsalva maneuver. Transthoracic and transesophageal echocardiogram shows asymmetric septal hypertrophy (ASH) with left ventricular outflow tract obstruction provoked by systolic anterior motion of the mitral valve at rest (50mmHg) or provocation (82mmHg), mitral annular calcification (MAC) with mild to moderate mitral regurgitation, left atrial enlargement (Fig. 1), mild tricuspid regurgitation, interatrial septal aneurysm with PFO, left ventricular ejection fraction of 77%, global longitudinal deformation of −20% and TAPSE of 22mm. Transesophageal echocardiogram corroborates the presence of ASH and MAC simulating a pearl necklace, interatrial septal aneurysm with PFO with abundant bubbles passing from right to left in the agitated saline contrast study (Fig. 2) and atheromatous plaques in the aortic arch were detected. She is receiving medical treatment with beta-blocker, and oral anticoagulation and is programmed for alcohol septal ablation.
Hypertrophic cardiomyopathy is a primary disease of the myocardium, characterized by the presence of an abnormal hypertrophy of the left ventricle, affecting one in 500 of the general population. Approximately two-third of the patients have left ventricular outflow tract obstruction. The onset and severity of symptoms varies widely, many people do not have symptoms but others experience severe complications, including arrhytmias, shortness of breath with exertion, chest pain, dizziness and fainting spells, dilated cardiomyopathy, mitral valve problems and sudden cardiac death. Sudden cardiac death is estimated to occur in about 1% of patients of all ages each year, but this condition is most often in younger people (<30 years-old). Recently, Haruki et al.,1 found that in hypertophic cardiomyopathy, the incidence of stroke and embolic events is about 1.0% per year; older age and enlargement of left atrium are considered possible risk factors for embolic events in patients with hypertrophic cardiomyopathy without documented atrial fibrillation. The echocardiography is the method of choose in the diagnosis and follow-up of these patients.2
The mitral annular calcification (MAC) is a chronic, degenerative process in the fibrous base of the mitral valve, associated with both a degenerative process such as atherosclerosis and abnormalities in the metabolism of calcium-phosphorus. MAC may be considered a potential cause of thromboembolism as a mass having propensity for thrombus formation.
The ASH associated with MAC increases with age with a prevalence of 0% at 60 years, 14% at 70, 16% at 80 and 29% at 90 years,3 also it is associated with sudden death.4
It was described that the presence of PFO increases the risk of stroke of 25% in the general population to 30–40%.5
The association between these three pathologies is uncommon and increase the risk of stroke and sudden death. Our patient, despite having important risk factors for stroke, has not yet presented any symptoms suggestive of cerebral infarction, because she has a close medical monitoring.
Conclusions- 1.
The association of obstructive hypertrophic cardiomyopathy with mitral annular calcification and patent foramen ovale is uncommon.
- 2.
This association increases the risk of sudden death and stroke.
- 3.
These patients need a closer monitoring in order to avoid a fatal outcome.
- 4.
The echocardiography is the method of choose for diagnosis and follow-up of these patients.
None declared.
Conflict of interestsThere is no conflict of interest between the authors.