Borderline personality disorder (BPD) is a common and severe mental illness. Early detection is important and reliable screening instruments are required. To date, however, there has been no evidence of any specific BPD screening tool validated for the Spanish-speaking population. The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) is a 10-item self-report questionnaire that can detect the presence of BPD in a reliable and quick manner. The aim of the present study is the validation of the MSI-BPD for its use in the Spanish-speaking population.
MethodPsychometric properties of the MSI-BPD Spanish version were examined in a sample of 344 participants (170 outpatients with the possible diagnosis of BPD and 174 healthy controls).
ResultsExploratory factor analysis revealed the existence of a bi-factorial structure. The scale showed a high internal consistency (KR-20=0.873) and an optimal test-retest reliability (ICC=0.87). Using logistic regression analyses and taking the DIB-R as reference, a best cut-off of 7 was determined, obtaining a good sensitivity (0.71) and specificity (0.68). The area under the curve was 0.742 (95% CI 0.660–0.824). The discriminant analysis showed a classification ability of 72.8%.
ConclusionsThe Spanish version of the MSI-BPD has good psychometric properties as a measure for the screening of BPD. Its ease and quickness of use make it valuable to detect the presence of BPD in clinical and research settings.
El trastorno límite de la personalidad (TLP) es un trastorno mental frecuente y grave. Su detección precoz es importante y para ello se requieren instrumentos fiables de cribado. Sin embargo, no existen hasta la fecha instrumentos de screening específicos para el TLP validados en población castellanohablante. El McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) es un cuestionario autoinformado de 10 ítems que permite detectar la presencia de TLP de forma fiable y rápida. El objetivo de este estudio es la validación del MSI-BPD para su uso en población de habla española.
MétodoSe examinaron las propiedades psicométricas de la versión española del MSI-BPD en una muestra de 344 participantes (170 pacientes con orientación diagnóstica de TLP y 174 controles sanos).
ResultadosEl análisis factorial exploratorio mostró la existencia de una estructura bifactorial. La escala presentó una elevada consistencia interna (KR-20=0,873) y una óptima fiabilidad test-retest (CCI=0,87). Mediante un análisis de regresión logística y con la DIB-R como referencia se estableció un punto de corte óptimo de 7, obteniendo una adecuada sensibilidad (0,71) y especificidad (0,68). El área bajo la curva fue de 0,742 (IC 95% 0,660-0,824). El análisis discriminante permitió observar una capacidad clasificatoria de la escala del 72,8%.
ConclusionesLa versión española del MSI-BPD presenta buenas propiedades psicométricas como instrumento de cribado del TLP. Su aplicación en la práctica clínica y en la investigación puede ser de gran utilidad para la detección del TLP por su rapidez y facilidad de uso.
Borderline personality disorder (BPD) is a common and serious mental disorder which has a prevalence estimated at from 0.5% to 5.9% of the general population, and 10% of psychiatric outpatients.1 Subjects diagnosed with BPD give rise to high direct and indirect economic costs, as well as severe social consequences for themselves, their families and the mental health system. This is due to their difficulties in social adaptation, their increased use of healthcare services and their high rate of suicide.1–4
BPD is characterised by a persistent pattern of instability in interpersonal relationships, self-image and affectivity, together with marked impulsiveness, especially in self-harming behaviour.5 The clinical heterogeneity of BPD, frequent comorbidity with other personality disorders and the periodic appearance of axis I disease add to the difficulty of establishing a reliable diagnosis, so that it is often under-diagnosed in many care contexts.1,4–7 This complexity makes it advisable to use standardised instruments to complement the usual clinical examiniation.8 Semistructured interviews such as the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II)9 and the Revised Diagnostic Interview for Borderlines (DIB-R),10 both of which have been validated in Spanish, are current the standard instruments for the diagnosis of BPD.11 Nevertheless, the need for clinicians to have previous experience to conduct these interviews and the long time they require hinder their use in general clinical practice.
Self-conducted instruments may be a good complementary tool, as they offer certain advantages over those conducted by others: as they are short and self-reporting they can easily be introduced in clinical practice. They save time for clinicians, permit better use in different healthcare or research contexts, reduce defensiveness in replies and, due to their greater standardisation, they usually offer superior psychometric properties. Their speed and ease of use make them especially useful as a screening system; however, it has to be pointed out that they must not be used as the sole diagnostic instrument, but should rather be used in an initial phase as a tool to identify those subjects who have to be examined subsequently more exhaustively.7,12
The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD)7 is the first screening scale for the diagnosis of BPD that is based on the diagnostic criteria of the DSM-IV and DSM-V. It emerged in response to the need for a valid and reliable scale that is easy to administer, making the preliminary identification of BPD possible. Until then the Personality Diagnostic Questionnaire13 was the only available screening method, although it was not specific for BPD and gave rise to a high rate of false positives and a low specificity (0.41). The MSI-BPD is a self-reporting questionnaire with 10 items that score as a disjunction (true-false). Its original version had suitable psychometric properties, especially in adolescent and young adult samples.7 Different studies with community, student and psychiatric populations have confirmed the psychometric reliability of this instrument as a means of screening for BPD.14–16 Due to this in recent years the scale has been adapted and validated in other languages.17–19
Several instruments have now been validated for the diagnosis and evaluation of personality disorders in Spanish-speaking populations. There are interviews and questionnaires for the diagnosis of general personality disorders, such as the SCID-II,9,20 the International Personality Disorder Examination,21,22 the Personality Assessment Inventory,23,24 the Minnesota Multiphase Personality Inventory-2,25,26 the Millon Clinical Multiaxial Inventory27,28 and the Personality Diagnostic Questionnaire-4,29,30 the last of which has a specific scale for BPD. There is also the above-mentioned DIB-R6,10 semistructured interview which is specific for BPD. Finally, in recent years scales have been validated to evaluate the clinical severity of BPD such as the Borderline Symptom List-2331,32 and the Clinical Global Impression Scale for Borderline Personality Disorder Patients.33
However, to date there have been no specific BPD screening instruments validated for Spanish-speaking population. The aim of this study is therefore to validate the Spanish version of the MSI-BPD for use in research as well as clinically for the Spanish-speaking population.
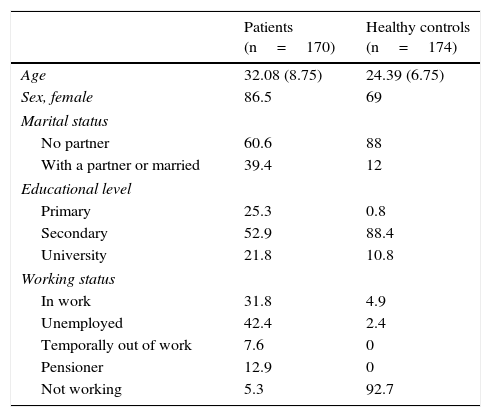
MethodologyParticipantsDepending on the different psychometric characteristics to be evaluated, the necessary sample size is estimated to stand at 150 subjects. Of the different psychometric characteristics to be evaluated, the one that requires the largest number of subjects to be properly studied is the validity of the construct (factorial structure). According to the guide (from 5 to 10 cases per item) proposed by Gorsuch,34 the sample size selected is the most suitable as it is above the high band of the interval which would delimit the necessary number of patients (50–100). The total sample was 344 subjects; Table 1 shows the main sociodemographic characteristics of the sample.
Sociodemographic characteristics of the patient and healthy control samples.
| Patients (n=170) | Healthy controls (n=174) | |
|---|---|---|
| Age | 32.08 (8.75) | 24.39 (6.75) |
| Sex, female | 86.5 | 69 |
| Marital status | ||
| No partner | 60.6 | 88 |
| With a partner or married | 39.4 | 12 |
| Educational level | ||
| Primary | 25.3 | 0.8 |
| Secondary | 52.9 | 88.4 |
| University | 21.8 | 10.8 |
| Working status | ||
| In work | 31.8 | 4.9 |
| Unemployed | 42.4 | 2.4 |
| Temporally out of work | 7.6 | 0 |
| Pensioner | 12.9 | 0 |
| Not working | 5.3 | 92.7 |
In the table data are shown as averages (standard deviations) or percentages.
The clinical group of patients was composed of 170 subjects with an initial diagnostic orientation of BPD, referred to the Hospital de la Santa Creu i Sant Pau and the Igualada Hospital for study and diagnosis. The general profile of the clinical sample was: a great majority of women, with an average age of 32 years old, with no stable partner, secondary education and without a stable job (see Table 1 for more details). The diagnosis of BPD was confirmed for 115 of them and ruled out for 47, who were all diagnosed with another personality disorder. It was not possible to finalise the evaluation of 8 patients as they lost contact with the unit.
The control group of healthy subject was composed of 174 volunteers with no psychiatric history, the majority of whom were students selected to participate in clinical pharmacology studies, together with hospital workers.
For the study all those participants who had a history of neurocognitive, schizophrenic spectrum and other psychotic disorders were excluded, together with those with alcohol or other toxic substances dependency and those with bipolar disorder.
ProcedureThe procedure of translation-back translation was followed to adapt the scale. The original scale was translated by a bilingual individual with clinical experience, and it was agreed with the rest of the research team. The first version was translated back into English by an independent translator, and this version was correct by the authors of the original scale, who verified the suitability of the original text (see Appendix 1 with the validation into Spanish of the MSI-BPD).
During the procedure the subjects included in the study with suspicion of BPD were first given the MSI-BPD and subsequently both diagnostic interviews: DIB-R and SCID-II. The Psychiatric Diagnostic Screening Questionnaire (PDSQ)35 was also administered to rule out psychiatric disease. The healthy controls were only given the MSI-BPD. The whole process was undertaken during a period of approximately from one week to 15 days. 3 cases were excluded from the initial sample due to error in filling out the questionnaire. To study the reliability of the test-retest, a subsample of 30 subjects answered the MSI-BPD for a second time, 2 weeks after it had first been administered.
All of the participants read and signed the informed consent form and took part in the study voluntarily.
Instruments- -
MSI-BPD7: is a self-reporting questionnaire with 10 items that score as a disjunction (true-false). It includes one item for each one of the first 8 criteria of the DSM-IV and DSM-V for BPD and 2 items for the ninth criterion of paranoia/dissociation. The original version of the scale has a high level of sensitivity (0.81) and specificity (0.85), where 7 is the optimum cut-off score. The test-retest was also reported to achieve a correct level of reliability (Spearman's rho=0.72, P<0.0001).
- -
DIB-R6: is a semistructured interview composed of 125 items (each one of which scores from 0 to 2 depending on frequency in the last 2 years). The items explore 4 dimensions: cognitive, emotional, impulsive patterns of action and interpersonal relationships. The partial scores in each dimension determine the overall score, which runs from 0 to 10 points, where 6 is the cut-off point compatible with diagnosis of BPD for the Spanish version of the interview.
- -
SCID-II20: is a semistructured clinical interview that makes it possible to evaluate all specific axis II personality disorders of the DSM-IV, as well as the 2 of the appendix and the non-specific ones. It contains 15 items for BPD in yes/no format, corresponding to the 9 criteria of the DSM-IV. Each DSM-IV criterion has a question in the SCID-II, except for the third one (identity alteration), which is included in 4 items, the fifth (recurring suicidal behaviour), with 2 items, and the eighth (inappropriate anger), with 3 questions.
- -
PDSQ35: is a self-administered questionnaire composed of 125 items with a response in the form of a disjunction (yes/no) designed to detect 13 of the most common psychiatric disorders. It questions the subject about the presence of symptoms in the previous 2 week for the first 6 sub-scales: major depression, post-traumatic stress disorder, Bulimia, obsessive-compulsive disorder, anxiety crisis and psychosis; or in the previous 6 months for the other 7 disorders included: Agoraphobia, social phobia, alcohol abuse/dependency, substance abuse/dependence, generalised anxiety disorder, somatisation disorder and hypochondria.
All analyses were undertaken using version 18.0 of the SPSS statistical package for Windows. Once the descriptive statistics of the sample had been calculated, the psychometric properties of the MSI-BPD were examined.
Exploratory factorial analysis was undertaken to evaluate the validity of the construct for the MSI-BPD. The internal consistency of the scale was also studied using the Kuder-Richardson (KR-20) coefficient. Test-retest reliability was analysed in a subsample of 30 patients diagnosed BPD using the intraclass correlation coefficient (ICC) between the MSI-BPD scores obtained in 2 consecutive administrations separated by 2 weeks.
Subsequently the levels of specificity and sensitivity were established to study the diagnostic concordance between the MSI-BPD and the DIB-R (using this as the gold standard scale for diagnosis of the disorder) in the clinical sample, taking different cut-off points into account and establishing the optimum cut-off point for the Spanish version of the MSI-BPD. Once the said cut-off point had been established logistic regression analysis was performed to analyse the diagnostic precision of the scale. The area under the COR curve was interpreted according to the ranges of diagnostic precision recommended by Fischer et al.36
The converging validity with the sub-scales of the SCID-II was estimated using the χ2 test with scores in the PDSQ sub-scales using Spearman correlations. The stepwise procedure was used for discriminatory analysis to examine the capacity of the MSI-BPD to correctly classify positive vs negative BPD cases.
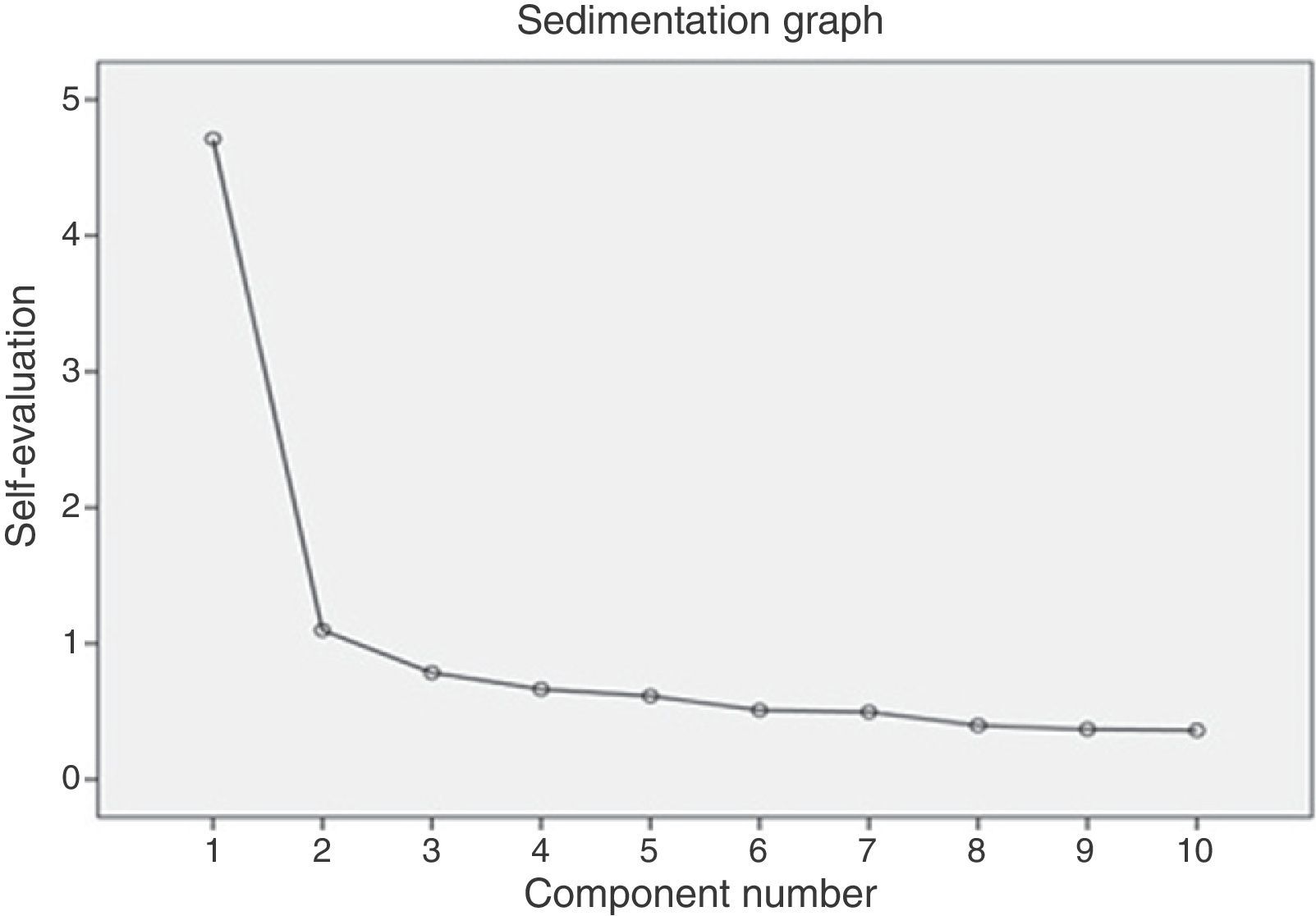
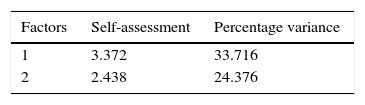
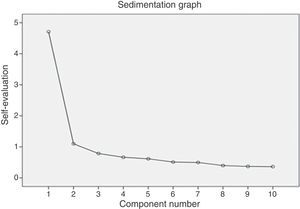
ResultsConstruct validityExploratory factorial analysis was undertaken with the complete sample. After checking that they fulfilled the application conditions (KMO=0.90 and Bartlett's significant sphericity test [χ2(45)=1.301,58, P<.001]), the main axes of the scale were factorised with Varimax rotation. The solution indicated the existence of 2 factors observed in the sedimentation graph (Fig. 1). The first factor showed a variance of 33.71%, and the second factor one of 24.37%. All of the items showed commonalities above 50% except for item 2 (46%) and 6 (49%). Respecting the factorial load, all of the items had high loads with the first factor except for item 7. In the matrix of components rotated by Varimax, items 7, 8 and 9 had high loads in the second factor. Analysis of the content of the items of both factors would show the existence of a principle factor characterised by items connected with the “impulsivity-emotionality” construct, and a second factor with items on “cognitive symptoms” (see Fig. 1). The said bifactor solution explained 58.09% of the total variance of the scale.
Internal consistencyFor the total sample the Spanish version of the MSI-BPD showed a good level of internal consistency (KR-20=0.873), indicating a high level of overall reliability with total scores that varied from 0 to 10 and an average score of 4.43 (DE=3.27).
Stability over timeThe test-retest reliability of the MSI-BPD was studied in a sub-sample of 30 participants. The scores obtained in two administrations separated by 2 weeks were compared using the ICC between both total scores (ICC=0.87).
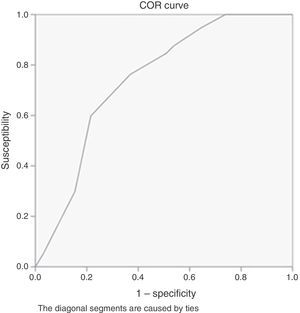
Sensitivity and specificityIn the clinical sample the MSI-BPD displayed a sensitivity of 0.71 and a specificity of 0.68 with the DIB-R, using a cut-off point located at 7 (as was set for the original version of the MSI-BPD).7 When a cut-off point of 6 was used, a slightly higher sensitivity of 0.84 was found, with a lower specificity of 0.51. The low specificity observed with the cut-off point at 6 justifies the use of the cut-off point at 7 for the Spanish version, the same as for the original one (Table 2).
Exploratory factorial analysis: explained variance and configuration matrix.
| Factors | Self-assessment | Percentage variance |
|---|---|---|
| 1 | 3.372 | 33.716 |
| 2 | 2.438 | 24.376 |
| Rotated components matrix | ||
|---|---|---|
| Component | ||
| 1 | 2 | |
| 1. Have there been problems in any of your closest personal relationships due to multiple arguments or frequent breaking-offs? | 0.778 | 0.206 |
| 2. Have you intentionally tried to harm yourself physically (burning, cutting or hitting yourself)? Have you ever attempted suicide? | 0.732 | −0.037 |
| 3. Have you had at least two of the following problems with impulsiveness; frequent over-eating, disproportionate expenses, alcohol abuse, episodes of verbal aggression? | 0.685 | 0.229 |
| 4. Have you felt extremely bad-tempered? | 0.681 | 0.297 |
| 5. Have you felt or do you feel angry most of the time? Have you often acted furiously or sarcastically? | 0.601 | 0.359 |
| 6. Have you often felt distrust in people? | 0.568 | 0.447 |
| 7. Have you often felt yourself to be unreal or that the things around you were not real? | 0.535 | 0.417 |
| 8. Have you felt or do you feel chronically empty? | 0.026 | 0.845 |
| 9. Have you often felt the feeling that you do not know who you are or that you do not have your own identity? | 0.280 | 0.800 |
| 10. Have you made desperate efforts to prevent feeling abandoned or being abandoned, for example by: repeatedly calling someone so that they confirm they are concerned about you, begging them not to leave you, physically grabbing them? | 0.499 | 0.630 |
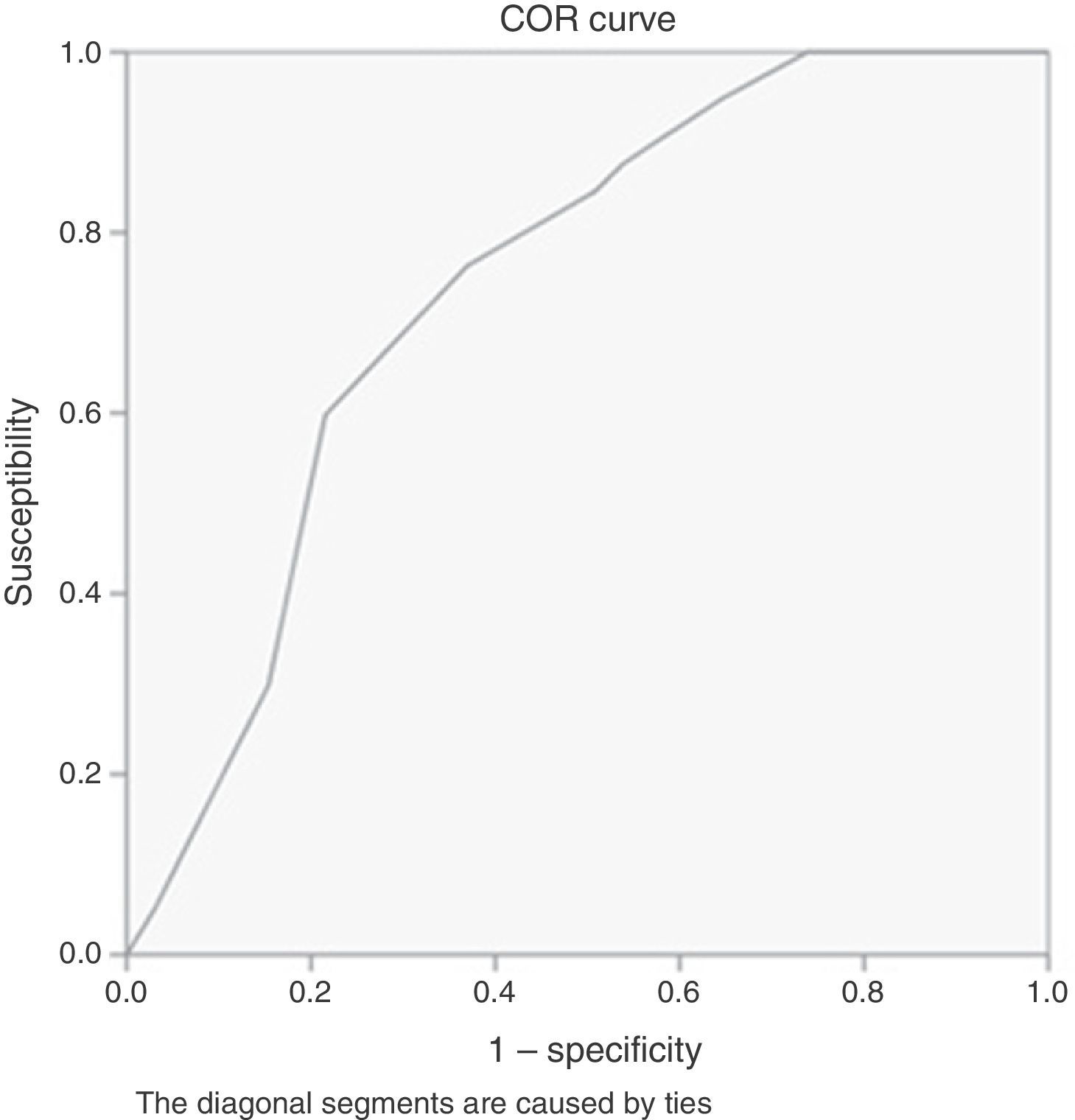
Analysis of the COR curves was undertaken by taken the DIB-R as the reference. For the cut-off point at 6, the area under the curve (AUC) was 0.752, P<.001 (with an interval of confidence of 0.65–0.85). For the cut-off point at 7 the AUC was 0.742, P<.001 (with an interval of confidence of 0.66–0.82) (Fig. 2).
Converging validityFor the converging validity analysis the result of the MSI-BPD was compared with the BPD sub-scale of the SCID-II, observing a significant relationship (χ2=15.42, P<.01), as well as with the Histrionic and Antisocial sub-scales (χ2=4.66 and χ2=6.67, P<.05). The sub-scales for Avoidance, Obsessive, Depressive, Paranoid and Narcissist showed a relationship of independence (P>.05), and with the others, the relationship between the variables could not be defined due to very low values in some of the theoretical frequencies.
A Spearman correlation was used to compare the scores of the MSI-BPD with those of the PDSQ (n=67), obtaining moderate correlations with the sub-scales of Agoraphobia (rho=0.63), major depression (rho=0.59), generalised anxiety (rho=0.53), social phobia (rho=0.55), Psychosis (rho=0.59), anxiety crisis (rho=0.49) and post-traumatic stress disorder (rho=0.43) (all with P<.01); and weaker correlations with the sub-scales of Bulimia (rho=0.34) and obsessive-compulsive disorder (rho=0.39) (P<.01), and somatisation disorder (rho=0.31) and Hypochondria (rho=0.27) (P<.05). No significant correlations were observed between the MSI-BPD and the other sub-scales of the PDSQ: alcohol abuse/dependency (rho=0.20) and substance abuse/dependency (rho=0.07) (P>.05).
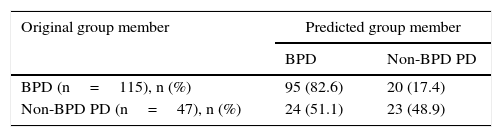
Discriminatory analysisFinally, discriminatory analysis was performed using the stepwise procedure to compare a sub-sample of patients with BPD (n=115) and another of patients with a non-BPD personality disorder (n=47). Analysis showed a Wilks’ λ=0.806, χ2=34.20 (P<.01). The discriminatory function counted for 100% of intersubject variability. The canonical correlation was 0.441 and the classification competence of the MSI-BPD was 72.8% (Table 3).
Discriminatory analysis of the MSI-BPD: capacity to detect cases of BPD versus non-BPD PD.
| Original group member | Predicted group member | |
|---|---|---|
| BPD | Non-BPD PD | |
| BPD (n=115), n (%) | 95 (82.6) | 20 (17.4) |
| Non-BPD PD (n=47), n (%) | 24 (51.1) | 23 (48.9) |
Classified correctly in 72.8% of the original grouped cases.
Although BPD is the most common personality disorder in the clinical field and the most widely researched at the current time,1 to date no screening scale had been validated for the Spanish-speaking population. This instrument may be highly useful in clinical practice and research, due to its ease and rapidity of use and because it is self-reporting. In this study the validation of the MSI-BPD in Spanish displays suitable psychometric characteristics.
Analysis of the dimensional structure of the Spanish version of the MSI-BPD showed a bifactorial solution, with a predominant main factor that we term “impulsiveness-emotionality” and a second factor labelled “cognitive symptoms”, which would include items 7, 8 and 9. In spite of the said resolution into 2 factors, a single overall score in the scale should be considered for reasons of consistency with the clinical concept of the disorder. As BPD is a disorder with heterogeneous symptoms and up to 5 areas of dysfunction the appearance of more than one factor is consistent with this, even though it is a single clinical entity.37 This is why the original version of the MSI-BPD7 was considered to be about a single factor with a single final score. In a similar way to our study, other validations of the scale have also reported a multifactor structure of the MSI-BPD; thus in a previous study in a Chinese population14 up to factor different factors were observed (affective deregulation, impulsiveness, chronic void and interpersonal problems), corresponding to the 4 main dimensions in the symptoms of BPD.
The internal consistency (KR-20=0.873) and test-retest reliability (ICC=0.873) of the Spanish version of the MSI-BPD were high, higher than those of the original version. Acceptable values were obtained for sensitivity (0.71) and specificity (0.68), with an optimum cut-off point at 7. This cut-off point was also used in validating the original version of the scale, although with higher diagnostic efficiency, sensitivity=0.81 and specificity=0.85. In our case we ruled out a cut-off point at 6 because although we obtained a high level of sensitivity (0.84), specificity fell considerably (0.51). The majority of adaptations have used the same cut-off point as the original scale, except for the ones by André et al.,38 Noblin et al.16 and Chanen et al.,39 whose cut-off points were ≥5, 5.5 and >7, respectively, giving slight differences in their results. The AUC observed in our study (0.742) would indicate that the MSI-BPD achieves moderate diagnostic precision. The different results obtained in other studies are largely due to the different populations and contexts in which they were undertaken. Studies such as that by Noblin et al.16 with hospitalised teenagers, the community study with women by Patel et al.15 or the one by Kröger et al.,18 with a heterogeneous population of outpatients, are good examples of this (with an AUC of 0.73, 0.79 and 0.90, respectively).
This study used the DIB-R as the criterion measurement, as this interview is considered to be the most reliable for diagnosis of BPD.6 The original version as well as the study by Patel et al.15 used the DIPD-BPD, while in other adaptations the SCID-II was the measurement selected (for example, by Melartin et al.,17 André et al.38 and Chanen et al.).39 This diversity in the choice of gold standard instrument as well as the other points mentioned above may also explain the different results of different validations respecting the validity of the criterion.
In the analysis of convergence between the MSI-BPD and the SCID-II, the correlation with the BPD sub-scale was significant, as could be expected. This was also the case with the Histrionic and Antisocial sub-scales, which could be expected due to the high level of comorbidity described and because they share certain diagnostic criteria, while all 3 are located in Cluster B Personality Disorders.40
Positive and significant correlations were observed between the MSI-BPD and different sub-scales of the PDSQ. The said results were expectable given the broad spectrum of symptoms that patients with BPD usually present and the high comorbidity with anxiety and affective disorders.1 In the same way the study by Noblin et al.16 also shows concurrencies between the MSI-BPD and axis I psychopathology and suicidal ideas. The validation of the Dutch version of the MSI-BPD19 also reported a moderate correlation (r=0.62) with the depression scale. Contrary to what could be expected, our study showed no convergence with the MSI-BPD for the PDSQ sub-scale for the consumption of toxic substances. Likewise, nor did Gardner and Qualter41 observe predictive validity of the MSI-BPD in connection with substance abuse or eating disorders. Discriminatory analysis between patients with BPD and individuals with other personality disorders showed that the Spanish version of the MSI-BPD seems to be able to correctly classify 72.8% of clinical cases.
It is important to point out the limitations of this study. Firstly, it has to be said that the group of patients was primarily composed of women, and this fact should be taken into account most especially given that the disorder is now thought to be more prevalent in men than was initially thought to be the case.1,15 Secondly, the fact that the clinical sample of BPD was selected in units that are specifically for BPD at a tertiary level must be taken into account. The severity of the cases selected may be greater than would be the case in the community or in primary care. This may have influenced the observed discriminatory power of the scale, as this discriminatory power would be lower in other environments with less severe cases. Sociodemographic variables may lead to significant differences in connection with the limit symptoms evaluated by the MSI-BPD, with comorbidity and social deterioration, etc., and these should be controlled in future studies. It also has to be pointed out that the size of the sub-sample of 30 subjects used to evaluate the stability of the scale over time was somewhat limited. Another aspect to be considered is the limited sub-sample of patients with a non-BPD personality disorder (n=47). Future studies should include a larger clinical sample for comparison, to permit better examination of the specificity of the scale.
To conclude, the Spanish version of the MSI-BPD has good psychometric properties and a high level of sensitivity for use as a screening tool for BPD. It may be highly useful in clinical practice for an initial diagnosis in patients with the suspicion of BPD in the Spanish-speaking population. Its rapidity and ease of use make it especially useful as a screening system in different contexts, such as primary care or mental health clinics. Nevertheless, the recommendation should be to use it as an instrument to identify those subjects who should be examined later on more exhaustively. It may also be useful in the field of research to quickly and simply rule out the possibility of a diagnosis of BPD.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed are according to the ethical norms of the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the paper. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Name:
Date:
Answer 1 (YES) or 2 (NO) in the following questions:
During this last year:
- 1.
Have there been problems in any of your closest personal relationships due to multiple arguments or frequent breaking-offs? 1 (YES) 2 (NO)
- 2.
Have you intentionally tried to harm yourself physically (burning, cutting or hitting yourself)? Have you ever attempted suicide? 1 (YES) 2 (NO)
- 3.
Have you had at least two of the following problems with impulsiveness; frequent over-eating, disproportionate expenses, alcohol abuse, episodes of verbal aggression? 1 (YES) 2 (NO)
- 4.
Have you felt extremely bad-tempered? 1 (YES) 2 (NO)
- 5.
Have you felt or do you feel angry most of the time? Have you often acted furiously or sarcastically? 1 (YES) 2 (NO)
- 6.
Have you often felt distrust in people? 1 (YES) 2 (NO)
- 7.
Have you often felt yourself to be unreal or that the things around you were not real? 1 (YES) 2 (NO)
- 8.
Have you felt or do you feel chronically empty? 1 (YES) 2 (NO)
- 9.
Have you often felt the feeling that you do not know who you are or that you do not have your own identity? 1 (YES) 2 (NO)
- 10.
Have you made desperate efforts to prevent feeling abandoned or being abandoned, for example by: repeatedly calling someone so that they confirm they are concerned about you, begging them not to leave you, physically grabbing them? 1 (YES) 2 (NO)
Please cite this article as: Soler J, Domínguez-Clavé E, García-Rizo C, Vega D, Elices M, Martín-Blanco A, et al. Validación de la versión española del McLean Screening Instrument for Borderline Personality Disorder. Rev Psiquiatr Salud Ment (Barc.). 2016;9:195–202.