The placement of central venous catheters (CVC) has become a common procedure. The position of the CVC tip may vary according to the intended use. Ideally it should be placed in the extra-pericardial vena cava due to the potential risk of vascular disruption, cardiac perforation, and/or thrombosis.
A simple, economical, little-used method with a high rate of accuracy for positioning the CVC tip is based on electrocardiographic changes in the P wave that occur as it advances towards the vena cava.
This article explains the procedure for correctly placing the catheter using the technique described.
La colocación de catéteres venosos centrales (CVC) se ha convertido en un procedimiento común. De acuerdo con el uso previsto, la posición de la punta de la CVC puede variar. Idealmente, debería ser colocada en la vena cava extrapericárdica por el riesgo potencial de disrupción vascular, perforación cardiaca y/o trombosis.
Un método poco utilizado, sencillo, económico, con una alta tasa de precisión para el posicionamiento de la punta del CVC se basa en cambios electrocardiográficos en la onda “P” que se producen durante su avance haciala vena cava.
En este artículo se explica el procedimiento para la colocación correcta del catéter mediante la técnica descrita.
A central venous catheter (CVC) is a catheter aimed at cannulating large veins to enable various medications to be perfused at an insertion site. They come with one to three lumens and are 20cm long for insertion near large veins or for peripheral insertion, or as long as 50–60cm which are usually placed in the basilic or cephalic vein in the arm.1
The placement of central venous catheters has become a common procedure due to its numerous indications such as: chemotherapy for cancer patients, amine administration, hyperosmolar solutions as well as parenteral nutrition or dextrose 50%, in addition to its utility for measuring central venous pressure, although this last use is widely debated.2
In the U.S., approximately 5,000,000 central lines are placed each year. The rate of mechanical complications during the procedure ranges from 6% to 19%, which accounts for 250,000 to 1,000,000 complications annually.3 These can be classified as early (during puncture) and late (due to the duration of the catheter). The main complications in the first group are mechanical (pneumothorax, artery puncture) at 12% and increase six-fold after the third insertion attempt. The second group includes infections and thrombosis, with a frequency of 13%.4,5
Several methods have been used to calculate the distance at which the CVC should be inserted to achieve the desired position, although it is always confirmed with a chest X-ray after the procedure. In addition to confirming the catheter is correctly placed, this also serves to rule out potential complications such as pneumothorax and/or haemothorax.
In 1995, Czepizak et al. presented a series of formulas to estimate the optimum placement of a CVC according to the access point and based on the patient's height.6
Depending on how it will be used, the CVC tip position can vary. Most central catheters that are used to measure venous pressure or to infuse solutions function well when placed in a large vessel. If it is placed far from the right atrium (RA) in a small vessel, it is likely that the catheter will be obstructed against the vessel wall and will not function well.7
Vascular damage caused by an incorrectly positioned CVC tip, both during insertion or secondary to chronic injury, has been recognised as an initial event and as perpetuating thrombosis. Should the catheter tip remain positioned against the vessel wall, it can become a source of permanent damage. Correctly placing the catheter can minimise this injury. It should be parallel to the wall of the superior vena cava and the catheter tip should be able to move freely within the vessel lumen.8
Methods used to optimise CVC placementThe veins most commonly used as CVC access routes are the internal jugular, subclavian, or femoral veins or the arm veins. There is a general evidence-based agreement for the preferential use of the right internal jugular vein based on its anatomy vis-à-vis the heart, as it presents a low risk of venous stenosis, thrombosis, and pneumothorax in that area. Traditionally, the central venous catheter insertion site has been determined by palpating anatomical references with a known relation to the vein to be cannulated.
The placement of the CVC tip is essential for it to work correctly. Ideally it should be placed in a vessel with a wide diameter, preferably outside the cardiac cavity and parallel to the vein axis to decrease the presence of lesions.
The ideal placement is in the extra-pericardial vena cava,8 due to the potential risk of vascular disruption or heart perforation with tamponade that has been demonstrated in case reports.9,10 Moreover, the high position of the catheter tip in the superior vena cava increases the risk of thrombosis.
The overall rate of complications is given by multiple factors, especially the experience of the medical staff, secondaries of percutaneous insertion, the catheter characteristics and type, the technique used, its indication and management while inserted.
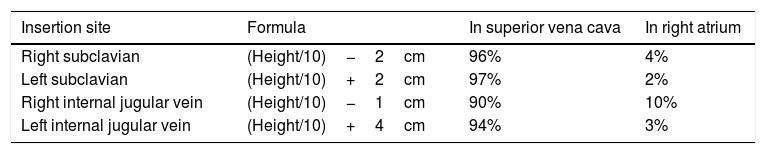
Knowing at what distance the catheter tip will be inserted is necessary, since it can differ according to age, gender, or height. A series of formulas for positioning the CVC tip in adult patients according to height have been described.6 In a 1995 study some formulas that are still used today were validated (Table 1)
CVC insertion length.
| Insertion site | Formula | In superior vena cava | In right atrium |
|---|---|---|---|
| Right subclavian | (Height/10)−2cm | 96% | 4% |
| Left subclavian | (Height/10)+2cm | 97% | 2% |
| Right internal jugular vein | (Height/10)−1cm | 90% | 10% |
| Left internal jugular vein | (Height/10)+4cm | 94% | 3% |
Czepizak CA, O‘Callaghan JM, Venus B. Evaluation of formulas for optimal positioning of central venous catheters. Chest 1995; 107: 1662–1664.
A chest X-ray is considered the most commonly used method for verifying the CVC placement. The catheter tip should be above the carina, thus ensuring placement above the pericardial sac. It stands out for its simplicity, economy, and speed of use. A 95% general efficacy is reported independent of the puncture site, efficacy being understood as the ability to position the CVC tip in the superior vena cava (SVC) and not in the right atrium11,12 (Fig. 1).
CVC in SVC on X-ray.12
Transoesophageal echocardiogram (TOE) enables the right atrium and superior vena cava near it to be visualised, enabling the CVC tip to be located even if it is 2cm or more from the terminal sulcus.11,13
The TOE enables two-dimensional vision and immediate correction in the case of misplacement; however, this requires an experienced operator.14
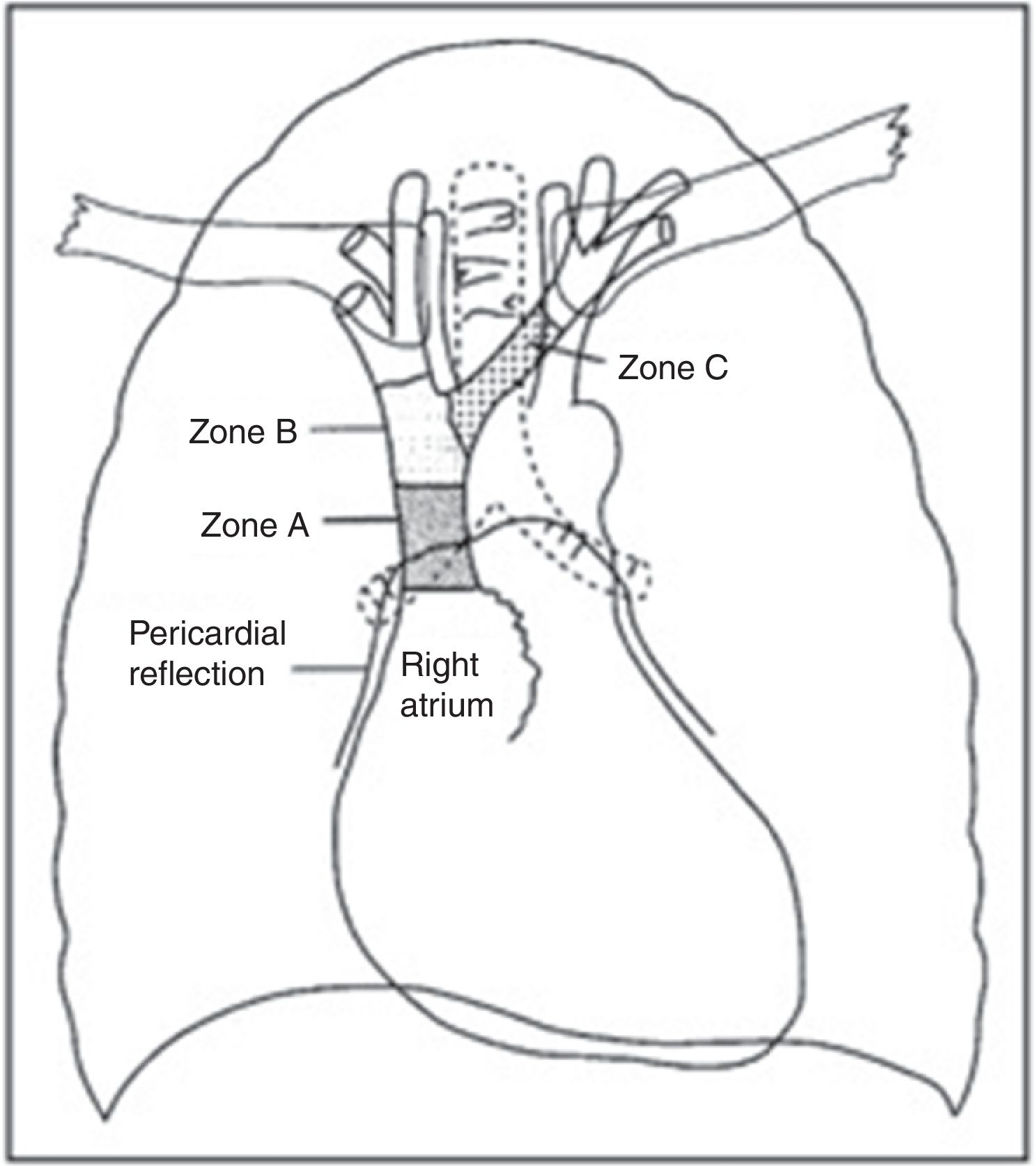
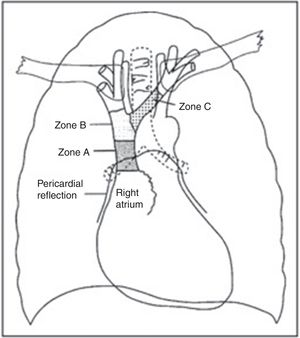
Three schematic zones have been proposed for the placement of the CVC tip.13
- –
Zone A (lower SVC and LAD) would be a safe zone for left-sided CVC tip insertions since it would enable great parallelism between the catheter tip and the vertical.
- –
This is an unsafe zone for right-sided insertions, therefore it is recommended they should be removed if placed in this zone.
- –
Zone B (upper SVC and brachiocephalic vein junction) would result in a safe zone for right-sided CVC tip insertions. However, it would be dangerous for catheters with left accesses due to the probability of forming a >40° angle with the vertical with the resulting risk of perforation. In these cases, the authors recommend advancing them.
- –
Lastly, zone C (proximal left brachiocephalic vein) would be a zone of questionable safety, only to be used for infusions over a short period and for fluid replacement (Fig. 2).
Figure 2.Schematic zones for positioning the CVC tip.13
(0.13MB).
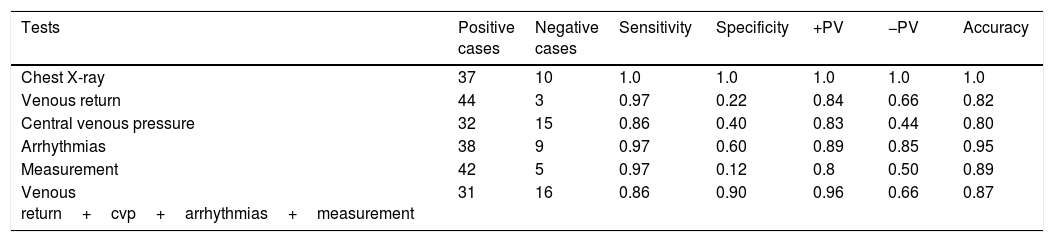
A study by Martinez et al.,15 assessed the validity of four tests to determine the CVC situation (venous return, central venous pressure waveform, arrhythmias, and difference between external measurement before and after the catheter placement) and position by comparing them on the chest X-ray. They found that the described tests are highly sensitive and non-specific for determining the position of the central venous catheter. Joining the four had more reliable values (Table 2).
Validity of clinical tests for determining the central venous catheter position.
| Tests | Positive cases | Negative cases | Sensitivity | Specificity | +PV | −PV | Accuracy |
|---|---|---|---|---|---|---|---|
| Chest X-ray | 37 | 10 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Venous return | 44 | 3 | 0.97 | 0.22 | 0.84 | 0.66 | 0.82 |
| Central venous pressure | 32 | 15 | 0.86 | 0.40 | 0.83 | 0.44 | 0.80 |
| Arrhythmias | 38 | 9 | 0.97 | 0.60 | 0.89 | 0.85 | 0.95 |
| Measurement | 42 | 5 | 0.97 | 0.12 | 0.8 | 0.50 | 0.89 |
| Venous return+cvp+arrhythmias+measurement | 31 | 16 | 0.86 | 0.90 | 0.96 | 0.66 | 0.87 |
Martínez F et al. Validez de las pruebas clínicas para determinar posición del catéter venoso central. Rev Med Inst Mex Seguro Soc 2009; 47 (6): 665–668.
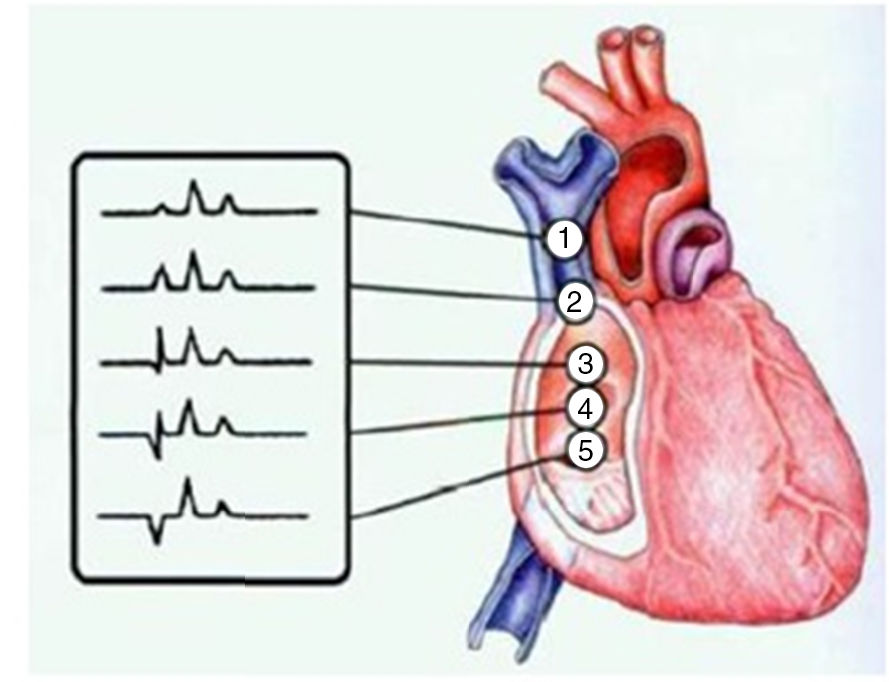
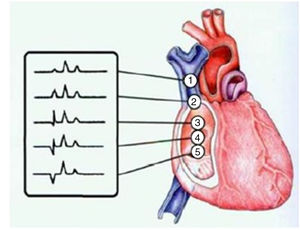
This system is based on electrocardiographic changes that occur as the CVC advances towards the vena cava which are visualised on the EKG monitor. Parallel to this advance, the P wave on the electrocardiogram (EKG) varies in amplitude. We know that when this amplitude peaks, the catheter tip is in the ideal position (distal segment of the vena cava) and when the P waveform become negative, the catheter has passed the vena cava and entered the right atrium, losing its ideal position. It is essential that the catheter tip be positioned correctly. An incorrect position can translate into complications such as: thrombosis, erosion, shifts and retractions with neck movement, or increased intrathoracic pressure. The only contraindication for using the intracavitary EKG method (IC-EKG) is the difficulty identifying the serial P wave on a surface electrocardiogram, although this type of patient is easily identified before the procedure, and other positioning methods will be used.
The position of the catheter tip in the interior of the vena cava can be detected by considering the catheter (or its guide) as an intravascular electrode that replaces the “red” electrode on the right shoulder of the normal surface electrocardiogram (EKG).
Steps to take- 1.
Check the presence of the P wave on the EKG.
- 2.
Observe the changes in the P wave on the EKG monitor while the catheter progresses towards the heart.
- 1.
Upper segment of the SVC: when the P wave has similar dimensions to normal, i.e. those of the surface EKG, this indicates that the catheter tip is in the upper segment of the superior vena cava.
- 2.
Lower segment of the SVC: When the height of the P wave is approximately half of the peak that it will reach at the cavo-atrial junction, this means that the catheter tip is in the lower segment of the superior vena cava, just about at that junction.
- 3.
Cavo-atrial junction: When the P wave is at its peak amplitude and no negative segments are seen in the standard P wave, the catheter tip is in the cavo-atrial junction, i.e. in the entrance to the right atrium (crista terminalis).
- 4.
Right atrium: When a negative incision is seen in P wave before the positive P wave, this is the first sign that the catheter tip has entered the right atrium. When the P wave becomes biphasic, the catheter tip is in the lower part of the right atrium16 (Fig. 3).
Figure 3.P-wave morphology changes according to the position of the CVC tip.16
(0.06MB).
- 1.
Aseptic and antiseptic techniques are used on the anterior chest wall below the right clavicle as well as the right anterior neck (or in the area where the venous access will be performed).
- 2.
A puncture is made below the right clavicle, seeking the subclavian vein.
- 3.
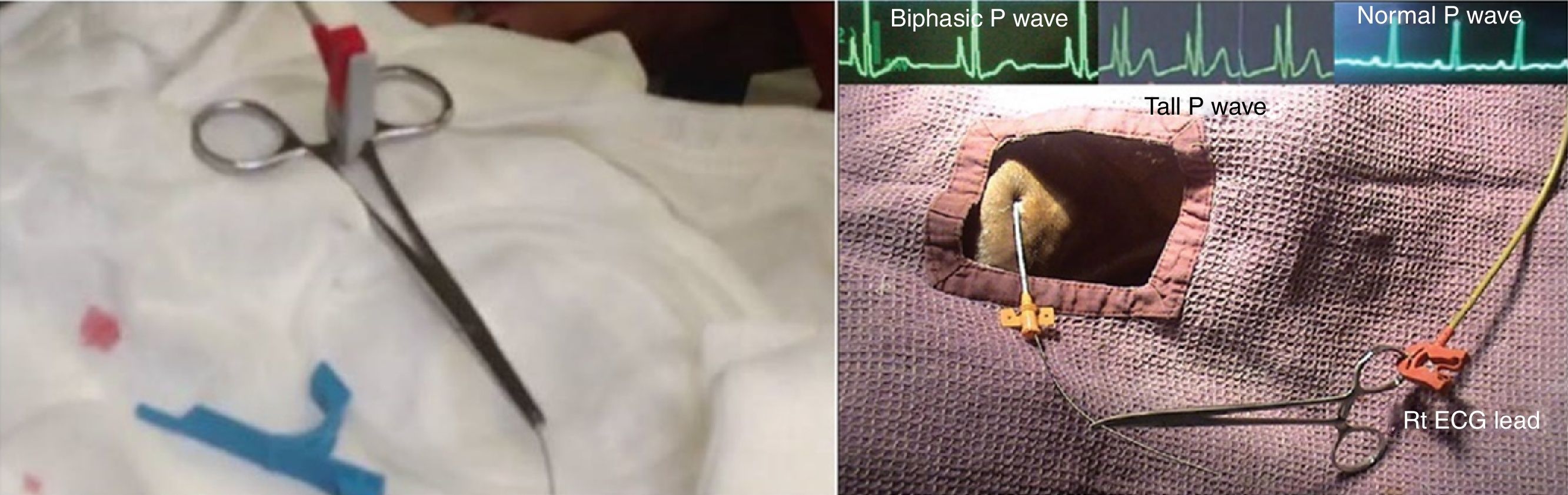
The metal guide wire is introduced using a syringe and the syringe needle is withdrawn (Fig. 4).
- 4.
A small incision is made in the skin and the tract expanded for the central venous catheter.
- 5.
The entire central venous catheter is introduced through the metal guide wire, the metal guide wire is withdrawn until its first mark.
- 6.
Forceps are placed at the tip of the metal guide wire and the V5 electrode for the electrocardiograph monitoring the patient is attached to the forceps (Fig. 5).
- 7.
The catheter is taken and withdrawn little by little until an isobiphasic P wave is seen on the monitor (Fig. 6).
- 8.
This shows how many centimetres our catheter is away before the metal guide wire is withdrawn and the catheter fixed to the skin.
- 9.
A plain-film chest X-ray is taken.
Most guidelines dictate the correct placement of the CVC to measure CVP when the catheter tip is located in the lower segment of the SVC, near its junction with the RA, thus preventing intracardial placement to prevent complications such as perforation, tamponade, arrhythmias, and thrombosis.17,18
No method for assessing the correct tip placement can truly exclude deviations or early complications with absolute certainty. Perhaps only by applying all the known methods (X-ray check, computed tomography, magnetic resonance imaging, multi-plane transoesophageal echocardiogram, electrocardiography) could we reach this objective. However, obviously, this is not possible due to geographical and financial reasons.19
Studies also suggest that ultrasound-guided placement of central venous catheters decreases the number of attempts, procedure time, and, as a result, the frequency of complications. The number of failed attempts decreases 86% with the use of ultrasound, the presentation of complications by 57%, and failed first attempts (catheters by jugular route) by 41%.20,21 The reduction in the number of complications implies a reduction in the hospital stay as well as in the cost of care. Three large problems are described for the universal incorporation of ultrasound-guided central venous punctures: low availability of ultrasound equipment, lack of training for professionals and their familiarity with the ultrasound, and increased costs, basically represented as the time spent in a determined clinic department before, during, and after ultrasound-guided insertion of the catheters, the costs of the ultrasound machines, and the costs for educating and training the specialists.
Several clinical studies have demonstrated a high precision rate for EKG-guided CVC placement. It has been proven that this practice has a 97.3% sensitivity and 100% specificity and a false positive rate of zero. All suspected cases of misplacement are detected by the intracavitary electrocardiogram.17,22
The use of an EKG is an alternative, high-precision technique for placing the CVC tip immediately and directly during the procedure, it prevents radiation exposure, it is a simple technique that can be performed by all members of the medical team, and no special equipment is needed. Moreover, the time required for the placement does not increase significantly by using this technique.18,19,23
Some studies conducted in recent years such as comparison of the bedside central venous catheter placement techniques: landmark vs electrocardiogram guidance and the intracavitary ECG method for positioning the tip of central venous catheters: results of an Italian multicenter study; have demonstrated that using an intracardiac EKG can eliminate the need for routine X-rays to verify the placement of the CVC since the EKG derivation provides information on the required depth during the insertion of central venous catheters, which reduces the possibility of complications and also increases the level of safety.23,24
ConclusionIntracavitary EKG is advisable, not only for economic reasons, but also for its high placement success rate. It helps to detect the atrial placement in each patient individually, reducing the impact of anatomical differences that can give rise to different distances between the point of insertion, the atrium, and the SVC-atrial junction.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.