Some authors have suggested that the diminished vascular blood supply, peripheral stability and thickness of the discoid meniscus (DM) would make it more prone to tears. The aims of this study are two-fold: (1) To analyse morphological characteristics by magnetic resonance (MRI), and (2) To correlate the size of the meniscus with the presence of meniscal tears.
MethodsThe MRI of patients ≤18 years-old over a period of 5 years were reviewed, and patients with DM were identified. We analysed demographic data, location (medial or lateral), morphology (Watanabe), meniscal tears (Crues classification), pattern, displacement, and other associated findings. Meniscal height and thickness per width (TxW) were also calculated. The correlation between variables: morphology, height and TxW with the presence of meniscal tears were statistically analysed.
ResultsSix hundred and eighty-five MRI (675 patients) were analysed. Forty-three knees (38 patients, 20 males) were found to have a DM (6.3%). The average age was 12.2±3.8 years (range: 4–18 years). Sixty-three percent had some type of meniscal injury. Patients with complete MD had a higher incidence of injuries (77.3 vs. 47.6%; P=.001). Longitudinal (bucket handle) and complex tears (n=11) only occurred in patients with complete DM. DM with tears presented a nonsignificant tendency to have higher meniscal height and higher TxW (6.29±1.26 vs. 5.75±.66mm; P=.20 and 107.5±36.02 vs. 91.54±16.5mm2; P=.162).
ConclusionThe results of this series support the theory that a larger meniscal size would be one of the main predisposing factors for the DM to be injured.
Study designCross-sectional study (Level of evidence: III).
Algunos autores han sugerido que su menor vascularización, la estabilidad periférica y el grosor del menisco discoide (MD) lo predispondrían a lesionarse. Los objetivos de este estudio son: 1) Analizar las características morfológicas por resonancia magnética (RM) de este grupo, y 2) Correlacionar el tamaño del menisco con la presencia de lesiones del menisco afectado.
MétodosSe evaluaron todas las RM de rodilla en pacientes ≤18 años en un período de 5 años y se identificaron aquellas con diagnóstico de MD. Se analizaron datos demográficos, localización, morfología, presencia de lesión intrameniscal, el patrón de la misma, desplazamiento y otros hallazgos asociados. Se calculó además la altura y altura por ancho meniscal (AxA). La correlación entre las variables: morfología, altura y AxA con la presencia de lesión fue analizada estadísticamente.
ResultadosSe evaluaron 685 RM de 675 pacientes. Cuarenta y tres rodillas (38 pacientes, 20 masculinos) presentaban MD (6,3%). La edad promedio fue de 12,2±3,8 años (r: 4-18 años). Los pacientes con MD completo tuvieron mayor incidencia de lesiones (77,3 vs. 47,6%; p=0,001). Las lesiones en asa de cubo y complejas (n=11) solo se presentaron en pacientes con MD completo. Los MD con lesión presentaron una tendencia no significativa a tener mayor altura meniscal y mayor AxA (6,29±1,26 vs. 5,75±0,66mm; p=0,20 y 107,5±36,02 vs. 91,54±16,5mm2; p=0,162).
ConclusiónLos resultados de esta serie apoyan la teoría de que el mayor tamaño meniscal sería uno de los principales factores que predisponen a que el MD se lesione.
Diseño del estudioEstudio transversal (Nivel de evidencia: III).
Discoid meniscus (DM) is an anatomical variation in which the meniscus has a greater than normal size and thickness. Some authors state that it is also associated with a reduction and alteration in the arrangement of the collagen fibres.1 This involvement was described for the first time by Young2 in 1889 in a cadaveric specimen, while Kroiss publicised it in 1910 and described it as the “snapping knee syndrome”.3
The aetiology of this condition is still unclear. Historically it was suggested that the shape of a normal meniscus resulted from the gradual reabsorption of its central part.4 Subsequent anatomical studies have shown that a normal meniscus is never discoid at any stage of embryonic development.5,6 The literature describes an incidence of approximately 0.4% to 17% for external DM and from 0.1% to 0.3% for internal DM.7 Nevertheless, the true incidence of this condition is unknown, given that it may be present asymptomatically.
A DM is more vulnerable to injury than a normal meniscus. Some authors have suggested a range of factors that would predispose it to meniscal lesions. These include its reduced vascularisation and the peripheral stability and thickness of the MD.8–10 However, although the latter factor is constantly mentioned in the literature, it has hardly been studied to date.11
The aims of this study are: (1) To use magnetic resonance imaging (MRI) to analyse the morphological characteristics of a group of patients with DM and (2) to correlate meniscus size with the presence of meniscal tears.
Material and methodsStudy designTransversal (level of evidence: III).
A computerised search was used to identify patients ≤18 years old with MRI of the knee performed in the diagnostic imaging department of the Sanatorio Allende over a 5 year period (January 2011 to January 2016). Patients with a history of previous knee surgery were excluded, as this may affect the analysis undertaken in this study.
Magnetic resonance imagingMRI was performed using eight channel 1.5-T Philips equipment. The scanning parameters for the coronal DP Fat Sat axial sequence were: slice thickness: 3mm, TR: 3080ms, TE 36ms. Sagittal DP: slice thickness 3mm, TR: 4700ms, TE: 71ms. Coronal DP: slice thickness 3mm, TR: 2730ms, TE: 23ms. Sagittal T1 and T2: slice thickness 3mm, TR: 540ms, TE: 12ms. Contrast material was not used in any case.
Image evaluationKodak Carestream PACS v. 10.2 imaging software was used to analyse and store the images. Two observers (JM and JP) evaluated the images separately and then established interpretations by consensus. The diagnosis was considered to be DM in cases with a transverse meniscus diameter greater than 20% of the total width of the tibia and/or when in the sagittal plane the bun sign was present in 3 consecutive slices.12
When patients were diagnosed DM their demographic data were analysed, together with their skeletal maturity (open or closed physis), clinical symptoms at the moment of the MRI and location (medial or lateral). Morphology was described as complete or incomplete DM depending on whether or not the tibial plateau was completely covered.13 The presence of meniscal lesions was documented in 4 types, according to the classification by Crues and Stoller,14 together with whether they were horizontal, radial, longitudinal, complex and degenerative.15 The type of displacement was classified according to the system used by Ahn et al.16 This system differentiates between 4 types: (1) no displacement: the peripheral part of the DM has not separated from the capsule and the meniscus is not displaced; (2) anterocentral: the periphery of the rear horn has detached from the capsule and the meniscus is displaced anteriorly or anterocentrally; (3) posterocentral: the periphery of the anterior horn has detached from the capsule and the DM has displaced posteriorly or posterocentrally, and (4) central: the periphery of the posterolateral portion broke or was lost, and the whole meniscus was displaced centrally towards the interchondral space. Other associated findings were recorded in the MRI, such as ligament injuries, osteochondritis and synovial plicas, etc.
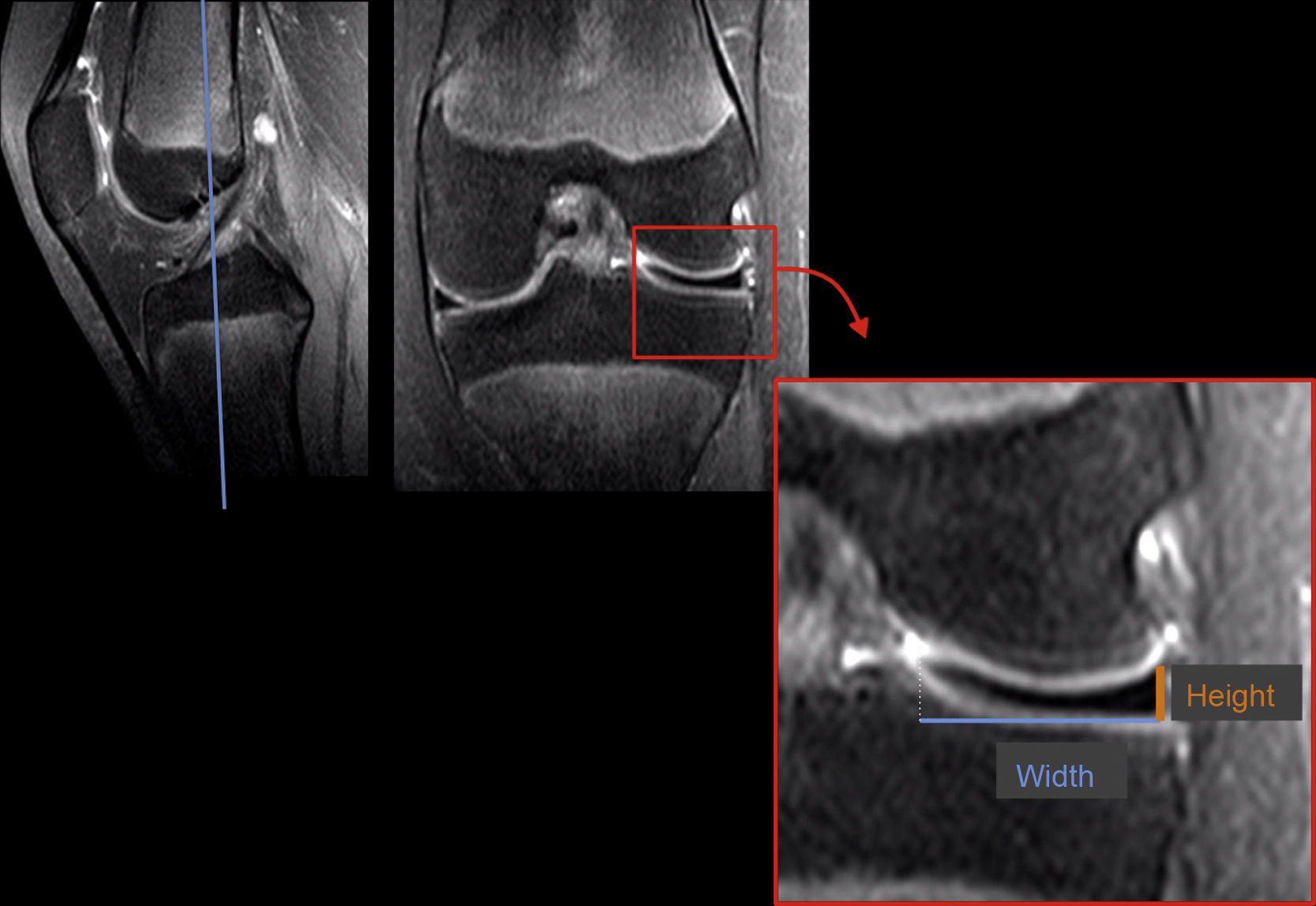
The height and height per width (HxW) of the meniscus were also calculated. The height was evaluated in a central coronal slice that passed through both tibial spines. Height was measured at the most peripheral part of the meniscus. The same coronal slice was used to calculate width, and the distance from the periphery to the free edge of the meniscus was measured. HxW was calculated by multiplying these 2 measurements (Fig. 1). In 4 patients with DM and bucket handle tears and in 2 cases of complex displacement it was impossible to evaluate HxW reliably, so the decision was taken to exclude these cases from the analysis.
Statistical analysisThe continuous variables were analysed using normalcy tests (Shapiro-Wilk) and they were expressed as an average and standard deviation (±SD). Inter- and intra-observer variability was not evaluated, given that this was reported in a previous study.17 The correlations between the morphology, height and HxW variables and the presence of a tear were analysed using the Student t-test. A P value of <.05 was used to indicate statistical significance.
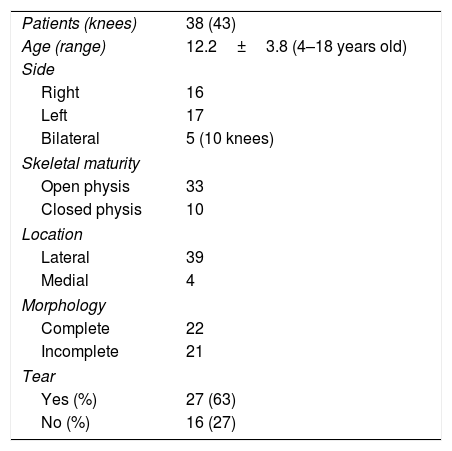
ResultsA total of 685 MRI scans (in 679 patients) were analysed. They were performed from January 2011 to January 2016 in patients under the age of 18 years old. Thirty eight patients (43 knees) were diagnosed DM (an incidence of 6%). The reasons why MRI studies were requested were: pain in 21 patients, blockage of the joint in 21 patients and knee trauma in the others. The demographic data of the sample are shown in Table 1.
63% of the sample had some type of meniscal tear: Crues type I (n=6), II (n=5) and III (n=16). The tear patterns were horizontal in 14 cases, complex in 8, bucket handle in 4 and a combination of vertical and horizontal in one case. According to Ahn's system, 31 cases had no displacement, 7 had anterocentral displacement, 3 posterocentral displacement and 2 central displacement. The patients with complete DM had a higher number of tears (77.3 vs. 47.6%; P=.001). Complex and longitudinal tears were only observed in complete discoid meniscuses. Torn discoid meniscuses showed a non-significant tendency to have a higher meniscus height and a greater HxW (6.29±1.26 vs. 5.75±.66mm, and 107.5±36.2 vs. 91.54±16.5mm2, P=.162, respectively).
When the images were analysed, other associated findings were observed in 23% of them: parameniscal cyst (n=5), synovial plica (n=2), osteochondritis dissecans (n=2) and breakage of the ACL (n=1).
DiscussionDM is an anatomical variation that is liable to degeneration and tears. Papadopoulos et al.1 suggested that this discoid lesion is a structural rather than a morphological variant. In their histological study they found disorganisation of the circular collagen network and a heterogeneous course of the collagen fibres arranged around the circumference of the DM structure. These histological alterations, in association with poor vascularisation and sometimes poor peripheral insertion of the capsule, predispose the meniscus to tearing more easily than a normal one.10,18 It has sometimes been reported that the higher incidence of tears would also be associated with a larger meniscal size and thickness.11 The aim of our work was to analyse the morphological characteristics detected by MRI in patients with DM under the age of 18 years old, and to correlate meniscus size with the presence of tears in the same.
In our series, more than half of the cases had meniscal tears. It is hard to compare the incidence of tears with those reported by other studies, given that asymptomatic patients are not usually subjected to imaging studies. The most frequent tear pattern found in our series was horizontal. This finding is consistent with those in other series.15,19,20 This pattern of tear is believed to arise due to the shearing forces of the femoral condyle on an abnormally shaped meniscus.21
The knees with complete DM in our sample had a higher incidence of lesions. We also observed that complex and longitudinal bucket handle tears, i.e., those with the worst prognosis, were only present in cases of complete DM. Likewise, we found a tendency in those with a greater height and HxW to suffer tears. We believe that there is logic in this relationship, given that a larger diameter would generate a biomechanical alteration in knee functioning with a large amount of meniscus tissue under stress, and that this could lead it to tear. Ayala et al.11 reviewed 33 patients with DM and classified them into 2 types, depending on the thickness of the free edge of the meniscus: wedge and tablet. The latter type had greater height and an 83% incidence of meniscal tear, while corresponding figure for the wedge type was only 33% (P<.005). They also observed that the patients with tablet morphology suffered tears at an earlier age. Although the latter point was not analysed in our study, anecdotally we noticed that patients who consulted at a younger age with pain or blockage of the joint usually had a larger discoid meniscus and more complex tears. Some authors11 have suggested performing partial meniscectomies on patients with a complete discoid meniscus due to the high risk that they will develop tears. In our practice we only prescribe surgery for patients with sufficient mechanical symptoms (with or without a torn meniscus) to justify the operation. Although patients with a large complete DM would be at greater risk of tearing, some of them display adaptive changes in the knee that allow it to function satisfactorily without the need for surgery.22 On the other hand, although the clinical results of saucerisation (partial meniscectomy) are usually favourable over the short term, they tend to worsen over longer periods of follow-up. In a recent study that evaluated the results of saucerisation after 11 years of follow-up, 37% of the patients required revision surgery and 42% had functional results that were mediocre or poor.23
Our study has some limitations that should be mentioned. The sample size is relatively small, and it may explain some of the findings obtained. However, the condition is a rare one, and after evaluating a large number of images only 6% showed DM. We admit that it is possible that this overall incidence and the frequency of tears are overestimated, given that patients subjected to MRI have a symptom that motivates them to undergo the study. Nevertheless, this selection bias is probably less than it is in studies that evaluate incidence in arthroscopy. It was impossible in some patients with bucket handle or complex tears to reliably evaluate HxW, so that they were excluded. In spite of these limitations data were obtained that help to understand how the morphology of DM would affect the development of meniscus tears, and these data could be applied in everyday practice.
A higher frequency of meniscus tears was observed in patients with complete DM and those with higher examples at a great height. The results of this series support the theory that a larger meniscus would be one of the main factors that predispose to a torn DM. These findings should be taken into account when advising parents about the prognosis for a patient with DM.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that for this research no experiments took place in human beings or animals.
Data confidentialityThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Masquijo JJ, Bernocco F, Porta J. Menisco discoide en niños y adolescentes: correlación entre la morfología y la presencia de lesiones. Rev Esp Cir Ortop Traumatol. 2019;63:24–28.