Preoperative 3D modelling enables more effective diagnosis and simulates the surgical procedure.
Material and methodsWe report twenty cases of acetabular fractures with preoperative planning performed by pre-contouring synthesis plates on a 3D printed mould obtained from a computerised tomography (CT) scan.
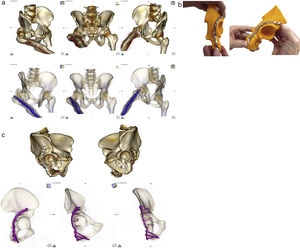
The mould impression was made with the DaVinci 1.0 printer model (XYZ Printing). After obtaining the printed hemipelvis, we proceeded to select the implant size (pelvic Matta system, Stryker®) that matched the characteristics of the fracture and the approach to be used.
ResultsPrinting the moulds took a mean of 385min (322–539), and 238g of plastic were used to print the model (180–410). In all cases, anatomic reduction was obtained and intra-operative changes were not required in the initial contouring of the plates. The time needed to perform the full osteosynthesis, once the fracture had been reduced was 16.9min (10–24). In one case fixed with two plates, a postoperative CT scan showed partial contact of the implant with the surface of the quadrilateral plate. In the remaining cases, the contact was complete.
ConclusionsIn conclusion, our results suggest that the use of preoperative planning, by printing 3D mirror imaging models of the opposite hemipelvis and pre-contouring plates over the mould, might effectively achieve a predefined surgical objective and reduce the inherent risks in these difficult procedures.
La planificación y premodelado 3D nos permiten un diagnóstico más efectivo y poder realizar una simulación del procedimiento quirúrgico.
Material y métodosDescribimos 20 fracturas de acetábulo en las que se premoldearon las placas de osteosíntesis definitivas sobre modelos obtenidos de estudios de tomografía axial computarizada (TAC) y materializados con una impresora 3D doméstica.
La impresión del molde se realiza con la impresora doméstica DaVinci 1.0 (XYZ Printing®). Tras imprimir la hemipelvis se procede a la selección de los tamaños de los implantes (pelvic Matta system, Stryker®) que más se adapten a las características de la fractura y al abordaje seleccionado.
ResultadosLos minutos medios empleados para la impresión de los moldes fueron 385 (322-539), empleando como media 238g de plástico (180-410). En todos los casos se obtuvo una reducción anatómica y no fue necesario realizar modificaciones intraoperatorias en la disposición inicial de las placas. El tiempo necesario para realizar la osteosíntesis completa, una vez reducida la fractura, fue de 16.9minutos (10-24). En un caso fijado con 2 placas, el control radiológico postoperatorio mostró que una de ellas presentó un contacto parcial con la superficie de la lámina cuadrilátera. En el resto el contacto fue total.
ConclusionesNuestros resultados sugieren que el uso de la planificación preoperatoria, mediante la impresión 3D de modelos especulares de hemipelvis contralaterales y el premodelado de placas de osteosíntesis sobre ellos, nos lleva a alcanzar eficientemente un objetivo quirúrgico predefinido y a reducir los riesgos inherentes de estos procedimientos complejos.
Acetabular fractures are a surgical challenge for the orthopaedic surgeon. These fractures are generally a result of high energy trauma, with traffic accidents being the main cause, and they are therefore more common for people in their thirties and forties.1,2
The studies presented by Robert Judet and Emile Letournel revolutionised the therapeutic approach and they are still fully applicable nowadays. They considered that the same principles applied in the treatment of joint fractures (anatomical reduction, internal fixation and early mobilisation of the patient) needed to be applied to acetabular fractures.3,4
The anatomy of the pelvis and the acetabulum has been extensively studied, but precise identification of the pattern of fracturing is still complex for orthopaedic surgeons.4,5 When pelvic ring fractures need treating the correct surgical approach and obtainment of an anatomical reduction of the bony fragments are key elements, particularly when the acetabulum is involved, because functional prognosis may be compromised.6 Absolute congruency between the femoral head and the acetabulum is essential for good long-term outcome. It has been demonstrated that residual displacements over 2mm lead to early arthrosis of the hip, together with poor functional outcome.3 Given the spatial complexity and anatomical relationships with solid structures, these operations are considered complex and require previous experience which may, on occasions, be difficult to acquire due to a relatively low fracture rate of this type.7,8
With regard to imaging diagnosis, computerised axial tomography (CAT) has been in use since 1982 and has become protocolised testing for these patients.4 During recent years, advances in 3D reconstruction of radiologic studies has provided virtual surgical planning tools and these files may even be exported as three-dimensional meshes from which real models can be obtained with 3D printers.
The aim of this study was to study the usefulness of 3D printing for preoperative planning in patients suffering from acetabular fractures who required surgery. We based our study on the use of routine imaging tests carried out on these patients, demonstrating a new methodology for the application of 3D technology through a DIY (do it yourself) process in the field of orthopaedic surgery. Our aim was to see whether we could anticipate intraoperative contouring of the necessary plates to treat these fractures, and also to analyse the advantages and possible drawbacks of this method.
Material and methodsThis was an observational, prospective descriptive pilot study with analytical components. It took place from November 2014 to November 2015 when 20 patients were consecutively recruited, who had been admitted to hospital due to acetabular fracture which required surgery.
The study subjects had the following inclusion criteria:
- -
Men or women, over 18 years of age, who were admitted to hospital with acetabular fractures which required surgery.
- -
Unilateral fractures.
- -
Patients who had undergone a CAT scan of both hemipelvis to categorise the type of fracture prior to surgery.
- -
Patients without dysplastic changes of the hip joint.
- -
Patients without osteosynthesis material or prosthetic implants in the healthy hemipelvis.
- -
Patients who gave their informed written consent to participate in the study.
Anatomical exclusion criteria were the presence of hip dysplasia or metallic material in the contralateral hemipelvis. This research was developed in accordance with good clinical practice guidelines, and with full acceptance of the ethical regulations in force (Declaration of Helsinki, review of Edinburgh 2000). Review, approval and protection was requested from the research committee and from the clinical research ethics committee of the general university hospital of Gregorio Marañón.
Demographic data and hospital patient progress data were obtained.
In these 20 cases of acetabular fractures preoperative planning was made with pre-contouring synthesis plates on a 3D printed mould obtained from computarised tomography which had been performed according to protocol on hospital admittance to diagnose and classify the type of fracture.3
The procedure began with analysis of the DICOM study of the standard multislice CAT scan (Philips Brilliance 64, slice thickness 0.625mm) performed on the patient on admittance to the emergency department. The scan was imported to the OsiriX® radiologic open-source software, using a Macintosh macbook pro (Apple Computers®, Cupertino, CA). Following segmentation to eliminate the sacrum and both femurs, rendering of the 3D surface was applied to the healthy hemipelvis in specular mode (inversion of X axis) to obtain the isosurface which was then exported as a 3D object in STL format. After this, using the Meshmixer® software, also open-source, self-repair of the virtual mesh was made, its final segmentation, its optimum orientation on the print tray and the creation of supports to increase the stability of the object. This programme also offered the possibility of free form hand-moulding to represent the fracture lines on the model, or instead reproduce them with marking ink on the final printed piece, to aid comprehension of the spatial relationships of the fracture and the synthesis material to be used. Finally, exporting the file obtained to the specific printing software XYZware® lamination of the layers of the object was made (where, when and how fast the plastic material should be deposited). The mould print was made with the DaVinci 1.0 (XYZ Printing®) printer which uses fused deposition modelling technology. Acrylonitrite-butadiene styrene (ABS) thermoplastic material was used with a filament diameter of 1.75mm, using standard configuration for the print (0.3mm, 10%, normal speed).
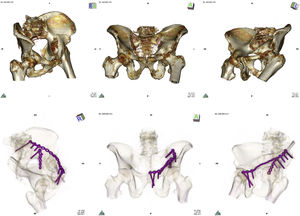
After obtaining the printed hemipelvis the size selection of the implants was made (pelvic matta system, Stryker®) which coincided with the characteristics of each fracture and the approach to be developed. For moulding the final osteosynthesis plates we initially used the templates available in the equipment, adapting its shape to anatomical contours. These were shaped around the plastic model to then reproduce the modelling of the final plates with the usual guiders. The consistency of the printed model made it possible to use surgical instruments directly on it (Fig. 1). Once the appropriateness of the plates had been confirmed with regards to size and anatomical adaptation to the chosen position, they were labelled and prepared for sterilisation using the standard procedures in the central hospital service for proceeding with implantation after fracture reduction. All surgical interventions were performed by the main author of this article. In order to confirm fracture reduction and contact of the osteosynthesis plates with the cortical surface, 3 Judet projections were obtained in plain X-rays. Reduction was considered anatomical when the joint line was restored in all projections. Contact of the plates was considered total in the cases where there was no clearly visible intermediate radiodensity between the cortical bone and the implant, and partial when this was visible.
Descriptive statistics were performed of the measured variables using frequency measurements (absolute and percentages) for categorical variables and measurements of centralisation and dispersion (mean, and standard deviation) for quantitative variables.
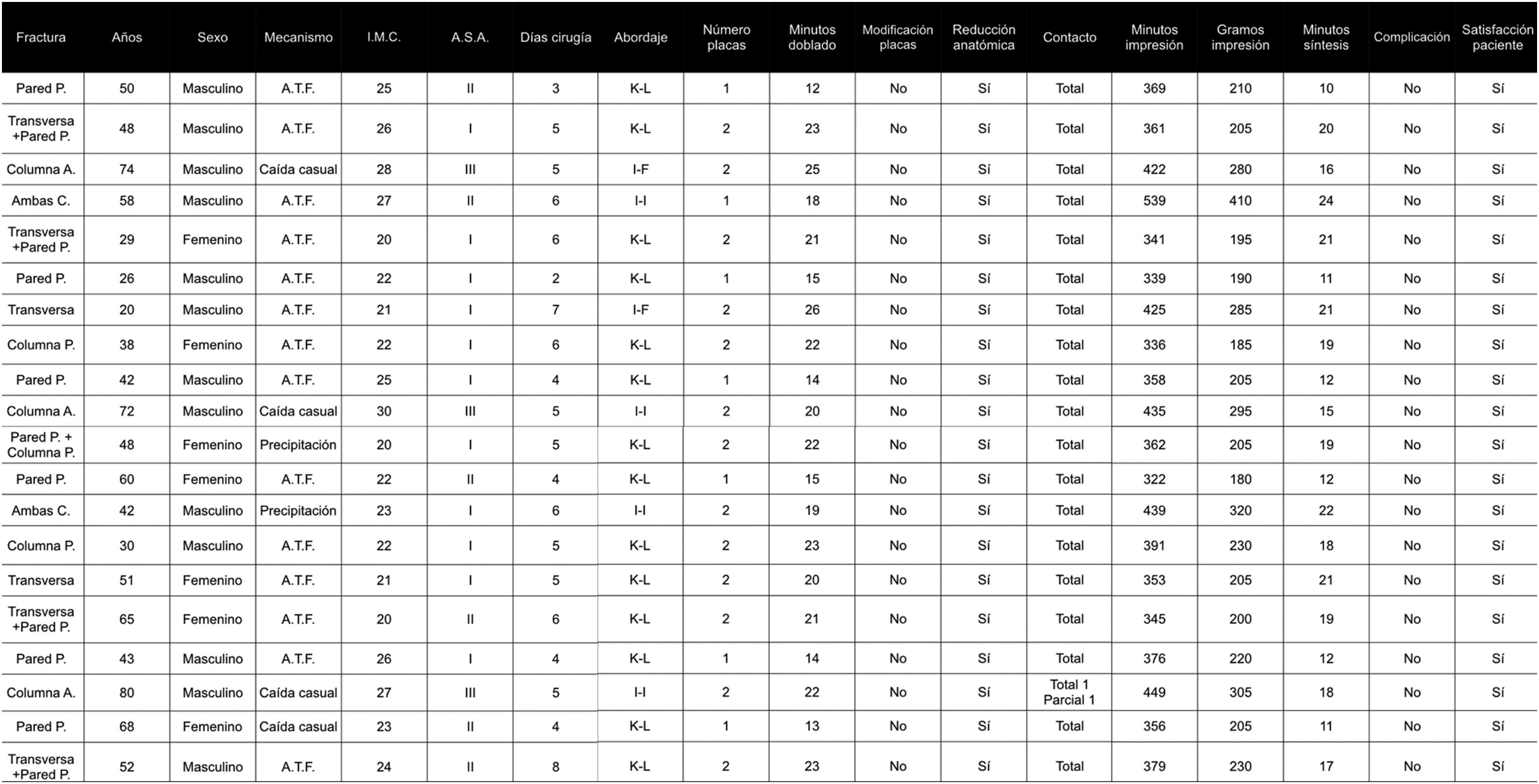
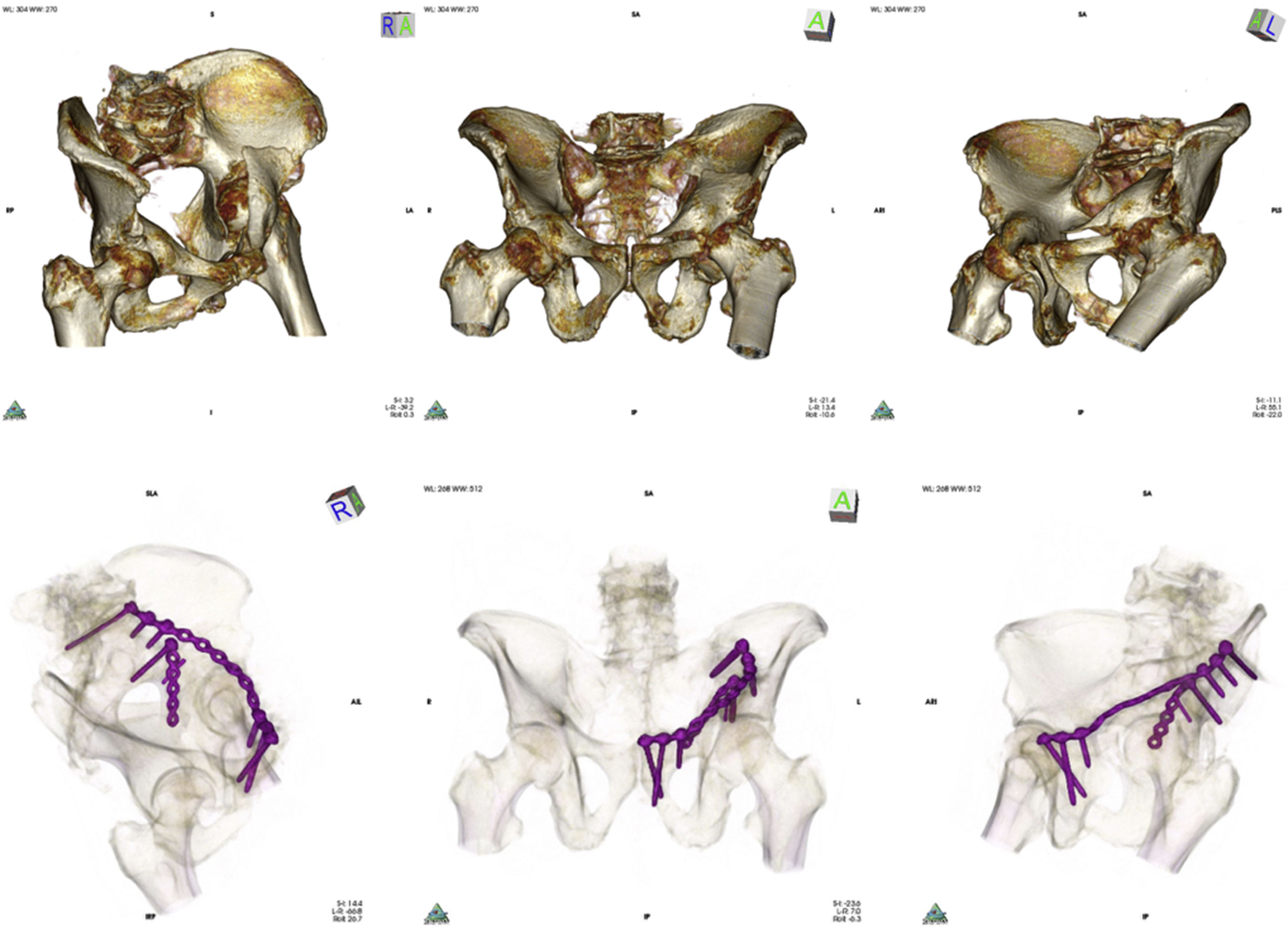
ResultsFig. 2 lists the demographic and surgical characteristics of the 20 patients who underwent surgery. During the inclusion period no cases of acetabular fractures were excluded from the study due to hip dysplasia or metallic material in the contralateral hemipelvis. The mean age of the patients was 49.8 years (20–80). 65% of them were male. The most common cause of fracture was traffic accidents (70%) followed by casual falls (20%) and falls from a height in attempted suicides (10%). The body mass index was 23.7 (20–30). 60% presented with a type I anaesthesia risk score, 25% with type ii and 15% with type iii. Mean time from when the fracture occurred to final osetosynthesis was 5 days (2–8). The most common approach was the Kocher-Langenbeck (14 patients) approach, followed by the ilio-inguinal (4 patients) and limited ilio-femoral approaches (2 patients). The processing of files and printing of the moulds was carried out by the authors of this article. The mean minutes required for processing the DICOM files to obtaining the final “stl” files for printing were 10.7 (9–15). The mean minutes used for printing the moulds were 385 (322–539), using as a mean 238g of plastic to print the model and its supports (180–410). In 7 patients one osteosynthesis plate was used, and 2 were used in the remainder of cases. The implants were folded for a mean of 19.8min (13–26). In all cases an anatomical reduction was obtained and it was not necessary to make intraoperative changes to the initial plates. The time required for complete osteosynthesis, once the fracture had been reduced, was 16.9min (10–24). In 5 patients an abdomen and pelvis CAT scan was performed during the post-operative period, prescribed by a practitioner due to causes other than acetabular injury. In all cases plain X-ray images were obtained, showing 3 Judet projections. In one case which had been fixed with 2 plates, the postoperative control X-ray showed partial contact with the surface of the quadrilateral plate (Fig. 3). In all other cases contact was total. In all patients a postoperative anatomical articular reduction was confirmed in the X-rays. No gap or residual separation was apparent. There were no local complications and when patients were asked about their satisfaction with the procedure on hospital discharge they all stated they were satisfied.
Variables of the 20 patients included in the study.
Both C.: both columns; ASA: anaesthetic risk classification system from the American Society of Anaesthesiologists; TA: traffic accident; column A.: anterior column; column P.: posterior column; I-F: ilio-femoral; I-I: ilio-inguinal; BMI: body mass index; K-L: Kocher-Langenbeck; P wall.: posterior wall.
Top: CAT imaging after carrying out volume rendering showing Judet projections (wing, anteroposterior and obturator) in anterior spine fracture and quadrilateral plate of left acetabulum. Bottom: after 16-bit rendering of the postoperative CAT scan total contact of the plate was observed which neutralised the anterior spine and partial contact with the surface of the quadrilateral plate.
The treatment of acetabular fractures requires anatomical reduction to achieve good long-term functional results. Interventions are required which include complex approaches, exposing the patient to major risks, such as haemorrhaging, infection, neurovascular damage and heterotypic ossification.1–3,5,7,9–11 Since every acetabular injury is different, due to the singular traits of the fracture lines, the state of the soft tissues, associated injuries and the individual circumstances of each patient, we must plan each case separately and thereby acquire the habit of previously simulating each operation. Thanks to the development of digital radiology it is increasingly more common to use software for the post-processing of medical imaging. The diagnostic and preoperative design phases have progressed a step further thanks to three-dimensional rendering options. Specifically, in the field of surgery, volume and 3D surface reconstruction is highly versatile and may even be achieved with free programmes such as OsiriX®, using batches of images such as those obtained with helical axial tomography. With this software the orthopaedic surgeon may browse through the injury, take measurements and plan the surgical steps to be followed. 3D printing for planning intervention takes this procedure a step further, with optimisation of diagnosis, a simulation of the act of surgery and making advances in surgery even before it has been performed. After choosing and folding the most appropriate osteosynthesis plates, adjusting them to the poliaxial traits of the surface of the printed model, which precisely reproduces the anatomy of the individual patient, these are sterilised and used in surgery, optimising time in surgery, reducing errors and minimising risks.
3D printing technology, also known as additive manufacturing and rapid prototyping (RP), has been available for 30 years and has various applications in clinical practice. The most outstanding of these is preoperative planning, teaching or communication with the patient. RP is an expression which refers to a series of additive technologies based on the construction of a physical model, layer by layer, as a replica of a virtual model.12 The RP models obtained are accurate reproductions of the virtual model obtained by the CAT, with submillimetre concordance being achieved.13 These models facilitate diagnosis, improving interobserver concordance when classifying injuries14 and provide tactile information, so that the approach can be planned in the virtual model, including the design and the size of the osteosynthesis which is identically reproduced in surgery.15
For years different templates and guidelines have been manufactured, obtained from magnetic resonance, X-rays or axial tomography, and personalised for the execution of osteotomies prior to the implantation of arthoplasties, with good clinical outcome and a considerable reduction in time in surgery.16 To obtain these guidelines, patient information has to be sent to the engineers of marketing firms several weeks prior to performing surgery. Unfortunately this need for an intermediary delays surgery and uses up vast amounts of financial resources. In the field of fractures this preoperative made-to-measure anticipation was not used because the time margin was not available to create templates in a different place, through an independent company. The time periods marked by damage control surgery needed to be respected in many of these patients due to their associated injuries and because the more time that passed until surgery the more difficult anatomical reduction of the fracture would be. All the more so considering this anatomical reduction is the most complex step in surgical treatment of acetabular fractures.11
Scale 1:1 3D printing offers a tactile and visual experience, improving the interpretation of any object. It has been proven that precontouring of plates using 3D technology is possible.17 Preoperative planning using 3D printing models has been used to treat multiple fractures in complex anatomical locations, such as the heel,18 or the sequalae of orbital fractures.19,20 It has also been used for the treatment of jaw defects,21,22 complex tumour surgery23 and surgery of the spine.18 In all of them the injury is reproduced and intervention on it is planned.24–26
The impression of a model of a fractured acetabulum offers no real advantage in identifying the fracture lines compared with virtual rendering of the fracture observed in the computer monitor, and the selection and adaptation of the final osteosynthesis plates cannot be made, since the fracture is not reduced and therefore the anatomical shapes are of no use to us. Several authors have recently communicated good outcomes using segmentation techniques which produce a virtual reduction of the fracture and facilitate the printing of the reduced fractured hemipelvis. Additional 3D reconstruction steps are required here which usually necessitate help from computer or biomedical engineers and greater financial investment as the computer programmes are costly.27 In this article we have shown how precontouring can be directly performed on a printed mould in a similar way to our performance during surgery. We therefore reduce the need for improvising during surgery, reducing time in surgery, cutting complications and total costs, and promoting improvement in the precision of the anatomical restoration as we benefit from the indirect reduction of the fracture.
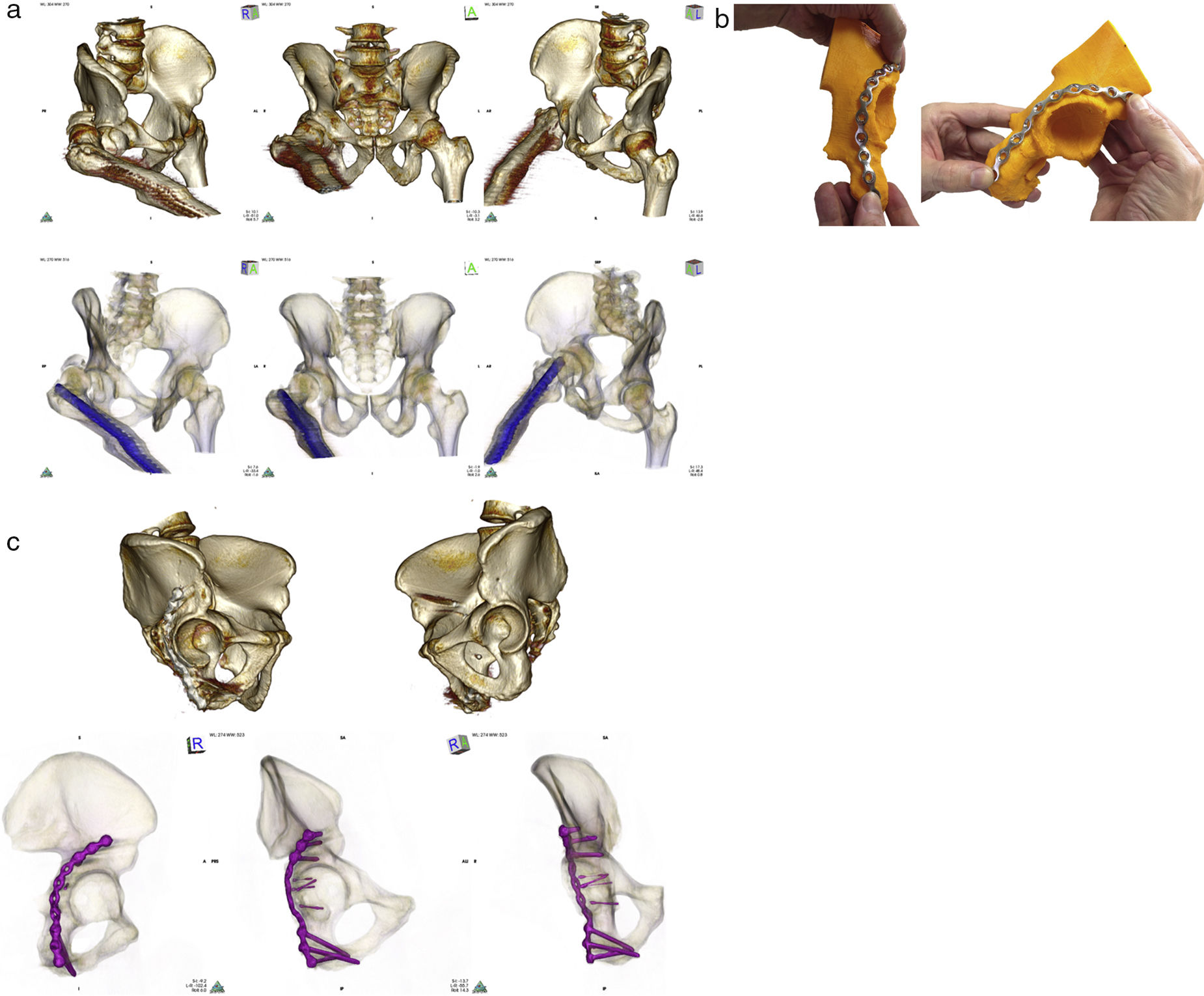
It is of note that in this project it is the surgeons themselves who complete the whole DIY process, from postprocessing of the radiologic imaging to 3D printing of the model, and also the surgical simulation and premodelling of the plates. The specular reflection of the healthy hemipelvis is used (inverse engineering) for the preoperative planning, with the advantage of reproducing the affected area on a mould without fractures or bony defects provoked by multiple fragments. Several studies have demonstrated the symmetry of both hemipelvis in healthy patients, with the exception of some rotational parameters.28 The specular reflection has already been used for other purposes, such as the realisation of osteotomies in the treatment of deformities of the forearm in children.29 It is possible to make use of specular reflection in pelvic ring fractures because the healthy contralateral hemipelvis is included in the standard X-ray imaging for diagnosis of the unilateral fractures and there is no need to increase the dose of radiation in the patient. Only bilateral fractures would be excluded from this technique, CAT scans which do not include a healthy hemipelvis, obvious hip dysplasias and patients with osetosynthesis material or previous prosthetic implants in the healthy hemipelvis. One of the patients in our series presented with a diaphyseal femoral nail which had been implanted due to a fracture years prior to the acetabular fracture. Since the nail was found on the same side as the acetabular fracture, no problems incurred and the specular impression of the model was possible (Fig. 4a).
(a) Top: CAT imaging after volume rendering showing Judet projections (obturator, anteroposterior and wing) in patient with posterior hip luxation and fracture of the right acetabular posterior wall. The patient had a diaphyseal nail in the right femur due to previous trauma. Bottom: the same projection with 16-bit rendering, where to show the relationship between the nail and the fracture, the transparency of the layer representing bony values was increased and the opaqueness of the layer representing the values corresponding to the metal was increased. (b) Printed model of the right acetabulum obtained after specular inversion of the healthy hemipelvis, left, and its segmentation, over which the final osteosynthesis plate has been adapted to neutralise the posterior wall. As no intermediate sizes were available, the selected plate was extended very distally over the ischium surface. (c) Top: CAT images after volume rendering and segmentation of the femoral head of both hemipelvis. Anatomical reduction of the fracture was observed compared to the healthy acetabulum. Bottom: total contact of the osteosynthese plate in Judet projections after segmentation and 16-bit volume rendering.
We should point out the advantages of being able to have previous well-adapted plates to the acetabular columns and walls. They may indirectly aid reduction of the fragments. They are an indicator of the final reduction of the fracture, since if there is not good cortical contact the reduction achieved is questionable. They optimise the distribution of the available space when 2 plates are implanted. This space is usually limited and if a plate is positioned in an inappropriate space it may remove space for the second plate. The use of more rigid plates is enabled. These are difficult to manage but offer extra stability and in some cases there is no need to use interfragmentary nails, which are always a risk in intra-articular structures. Partial contact in the neutralisation plate of the quadrilateral plate was only observed in one patient who had an anterior spine fracture and quadrilateral plate into which 2 plates had been implanted. This plate is only fixed with a nail and initial contact is more difficult to obtain and the introduction of the nail can move the plate and lead to loss of contact (Fig. 3).
The cost of RP is one of its potential disadvantages and is determined by the amount of material used, the cost of the 3D printer and the cost of the software licences.30 The cost of the manufacturer printing a model is between 500 and 900Euros.31 The recent fall in production costs has led to a situation where the end consumer has access to this technology, and 3D printers for domestic use is now within everyone's reach. Realistic reproductions may now be obtained autonomously at minimum cost, using the DIY trend and free tools. This autonomy and the lower cost has resulted in printers being introduced into many orthopaedic surgery departments. The printer model used in this study cost 390 Euros and a 600g plastic cartridge costs 24 Euros. The models were therefore obtained for under 12 Euros per unit.
This method begins with a radiologic study which has always be performed for diagnosis. Once the medical image has been obtained an added use is made of it, which does not increase costs or radiation and the product of an already completed medical study is capitalised from a clinical point of view.
To reduce printing time and the plastic material costs it is recommended that only the parts of the hemipelvis to be adapted to the implants be selected instead of printing out the complete hemipelvis. By doing this the possibility of the part breaking up on impact of printing is also reduced since they are smaller pieces,with stable bases and generally print out with fewer technical difficulties. Although ABS plastic material was used, the use of polylactic acid material (PLA) should be assessed because although it is less resistant it leads to lower deformation of the pieces during printing, is much more adherent, has higher maximum printing speeds and cools down faster. Furthermore, ABS is more likely to produce ultrafine particles than PLA, and good ventilation is therefore recommended due to the unpleasant smell of burnt plastic during extrusion.32
Using anatomical models notably improves communication between the surgeon and the patient and family members. It aids comprehension and increases trust regarding the surgical techniques to be used, which also increases overall satisfaction rates.33
Another advantage of the 3D models is their use as learning tools for young surgeons, where they may practise complex operations because they have models that reproduce the different fracture patterns.34 The surgical techniques require excellent spatial vision and manipulative skills. Nowadays, not only is it possible to simulate surgery it is also possible to manipulate the anatomical area as many times as necessary prior to the real surgical intervention, thanks to 3D printing.
Disadvantages to 3D printing are the resolution limitations (.1mm maximum) or the difficulty of including cartilage and soft tissues, which are excluded in the segmentation process of the radiologic imaging. Even so, we should be aware that 3D printing complements but does not replace the 2D interpretation of radiologic imaging by batches. 3D surgical printing is a valuable aid in simulating treatment when planning our operations. Another disadvantage of adapting to the plate measurement may be that the available implants are not as versatile as our requirements, and we may find cases in which the measurements available on the market are too large or too small, with no intermediate ones. We therefore have to use sizes which do not completely adapt to the individual case (Fig. 4b and c). A further drawback is that training in this field is essential to make full use of the information. It is also an added workload for the surgeon responsible for the surgical intervention. Instead of regarding this as a drawback this training is positive and necessary for the surgeons to improve their future performance in surgery and to optimise osteosynthesis time. Improving the adaptation of the implants justifies the work carried out prior to the intervention.
One limitation of this series is that CAT control was not obtained in all cases, with cases only being assessed with the plain Judet X-ray projections. This could have more precisely described the anatomical relationships obtained. However, we do not consider it ethical to obtain a postoperative control CAT to confirm plate contact, since this would involve further exposure to ionising radiations.
Although prospective studies with a control group are necessary, it seems obvious that pre-surgical work made on plate adaptation involves a reduction in time in surgery and could therefore reduce the risk of perioperative infection and other complications. The positive side of tailor-made surgery may be likened to the opportunities offered by haute couture over ready-to-wear, prêt-à-porter clothes. With 3D surgical printing techniques intraoperative radioscopy times are minimised, as are reduction and osteosynthesis times because we have prior experience of handling the printed model and the premoulded plates adapted to each individual case are available.
ConclusionsThe results presented suggest that the use of preoperative planning, using the printing out of 3D plastic models, obtained from mirror imaged CAT scans of the healthy hemipelvis and the use of previously premoulded osteosynthesis plates on these plastic models, may induce a predefined surgical objective. The osteosynthesis plates may also be better adapted, fracture reduction better processed, time in surgery shorter, and the inherent risks from this type of technically complex procedures lowered. As a result the treatment of these patients is optimised, and all at a very low cost.
Level of evidenceLevel of evidence iv.
FundingThe research team received a grant for this project which was the “SECOT 2014 research project award”.
Conflict of interestsThe authors have no conflict of interests to declare.
Our thanks to Mr. Félix Ballesteros Fominaya for his initial advice, to Mr. Guillermo Rodríguez Lozano for his help in printing out several models and the SECOT Foundation for providing us with a grant for research from its 2014 research projects award programme.
Please cite this article as: Chana Rodríguez F, Pérez Mañanes R, Narbona Cárceles FJ, Gil Martínez P. Utilidad de la impresión 3D para el tratamiento quirúrgico de las fracturas acetabulares. Beca proyecto de investigación SECOT 2014. Rev Esp Cir Ortop Traumatol. 2018;62:231–239.