The Department of Oral and Maxillofacial Surgery of the West General Hospital Dr. José Gregorio Hernández (OMS-WGH) located in the city of Caracas, Venezuela, provides emergency care 24h a day, 365 days a year.
ObjectiveTo determine the age, gender and most frequent reason for consultation in the emergency room of the OMS-WGH between January 2006 and December 2012.
MethodA cross-sectional retrospective epidemiological study was conducted on patients seen in the emergency room of the OMS-WGH, by evaluating 7531 medical records of patients treated in that period.
ResultsThere was a predominance of males with 58.3% (n=4391), and a mean age of 16–30 years old, with 46.5% (n=3509) of the patients having soft tissue trauma 65.71% (n=4949), 15.1% (n=1139) facial fractures, and 15.9% (n=1203) odontogenic infections.
ConclusionThe male population between 16 and 30 years are more prone to soft tissue trauma.
El departamento de Cirugía Bucal y Maxilofacial del Hospital General del Oeste Dr. José Gregorio Hernández (OMS-GTH), ubicado en la ciudad de Caracas (Venezuela) proporciona atención de urgencia las 24h del día, los 365 días del año.
ObjetivoDeterminar la edad, el sexo y el motivo de consulta más frecuente en las urgencias de OMS-GTH entre enero de 2006 y diciembre de 2012.
MétodoHemos realizado un estudio transversal retrospectivo epidemiológico de los pacientes atendidos en las urgencias de OMS-GTH mediante una evaluación de 7.531 historias clínicas de los pacientes tratados entre ese período.
ResultadosPredominó el sexo masculino con el 58,3% (n=4.391); la edad promedio fue de 16 a 30 años de edad; el 46,5% (n=3.509) de los pacientes presentaron trauma de tejidos blandos 65,71% (n=4.949), el 15,1% (n=1.139) fracturas faciales y el 15,9% (n=1.203) infecciones odontogénicas.
ConclusiónLa población masculina entre 16 y 30 años es más propensa a trauma de tejidos blandos.
Buccal and maxillofacial surgery addresses all the diseases associated with the three areas of the face: any wound that involves these areas will be dealt with by a buccal and maxillofacial surgeon, who will contribute to its resolution. The bones of the face serve to protect the associated organs due to their anatomical locations. Attackers or those who commit violent acts often aim for this anatomical area and the maxillofacial region tends to be an area that is associated with many traumas with different aetiologies, including chemical, physical and biological.
There are many epidemiological reports conducted worldwide on the reasons why patients attend emergency rooms seeking maxillofacial treatment, and there is a wide variety of political, social, economic and cultural factors relevant to each individual and country. This type of study has not been conducted in Venezuela, therefore our medical residency programme for buccal and maxillofacial surgery has assumed the responsibility of gathering these data for the benefit of the Venezuelan and Latin American population. We report on an epidemiologic study conducted between January 2006 and December 2012 and focused on determining the age, gender and the most common reasons for consultation at the emergency room of the Surgery Department for Buccal and Maxillofacial Surgery at the Hospital General del Oeste Dr. José Gregorio Hernández (HGO-BMFS), located in the city of Caracas (Venezuela), which provides 24-h emergency assistance 365 days a year.
Materials and methodsWe conducted an observational, retrospective study of the clinical record files from the emergency room at the Buccal and Maxillofacial Surgery Service from the HGO-BMFS in Caracas (Venezuela), for the period between 2006 and 2012. Illegible, incomplete or inexact records were dismissed. All the data was input into forms using Excel software in order to calculate totals. We aggregated a total of 7531 clinical records, from which totals and averages were calculated, according to the distributions of gender, age and diagnoses.
The diagnoses were divided into three groups according to the reason for consultation. The first group included lesions associated with wounds or open or closed traumas; the second group included fractures of the facial bones and the third group included odontogenic infections. In turn, each group was subdivided: group 1 into 8 sub-groups according to the facial region that was affected (frontal, submental, nasal, nasogenian, labial, orbital, buccal mucosa, auricle and temporoparietal region) and those in whom multiple regions were affected were grouped separately; group 2 was sub-divided according to the bone that was affected (mandibular, maxillary, zygomatic, frontal, nasal and vomer fractures); finally, odontogenic infections (group 3) was sub-divided according to aetiology into radicular remains, osteitis and advanced non-repairable cavities.
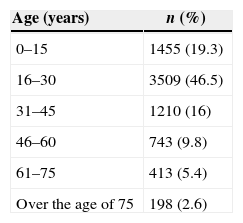
ResultsIn our study, we included 7531 clinical records from the Buccal and Maxillofacial Emergency Service, for patients who were treated between January 2006 and December 2012 at the HGO-BMFS. From the total of those patients, 58.4% (n=4392) were males and 41.6% (n=3139) were females; the most common age group was 16–30 years, representing 46.5% (n=3509) of the cases, followed by 0–15 years, representing 19.3% (n=1455) (Table 1).
Distribution by age of patients who attended the emergency room at the Buccal and Maxillofacial Surgery Service at the Hospital General del Oeste Dr. José Gregorio Hernández, between January 2006 and December 2012.
| Age (years) | n (%) |
|---|---|
| 0–15 | 1455 (19.3) |
| 16–30 | 3509 (46.5) |
| 31–45 | 1210 (16) |
| 46–60 | 743 (9.8) |
| 61–75 | 413 (5.4) |
| Over the age of 75 | 198 (2.6) |
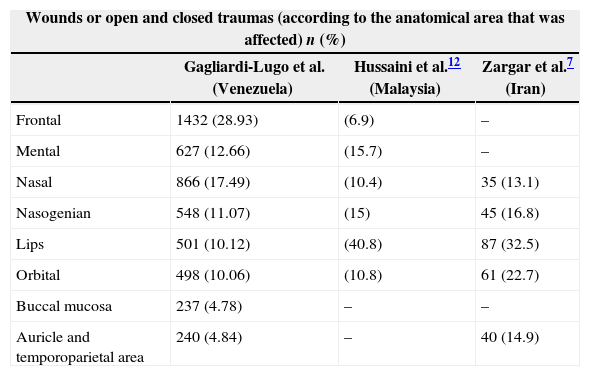
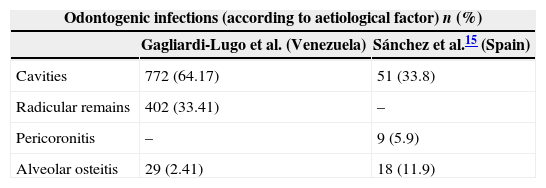
Group 1 (wounds or open and closed traumas) represented the primary reason for consultation at the emergency room, totalling 65.71% (n=4949). Within this group, the frontal region was the area affected most often, representing 28.93% (n=1432) of the cases, followed by the nasal region, at 17.49% (n=866) and the submental region, at 12.66% (n=627) (Table 2). Group 3 (odontogenic infections) represented the second highest group reason for consultation at the emergency room, totalling 15.97% (n=1203) of the cases, with advanced cavities being the main aetiological factor, totalling 64.17% (n=772) (Table 3). Lastly, Group 2, which comprised facial fractures, represented 15.12% (n=1139) of the cases, with the bone most commonly fractured being the mandible, in 51.62% (n=588) of the cases, followed by the maxillary bone in 25.9% (n=296). Both these cases were mainly due to dentoalveolar-type fractures. In third place in this group were nasal bone fractures, totalling 12.55% (n=143) of the cases (Table 4).
Distribution by wound or open and closed trauma areas compared with the results from other studies.
| Wounds or open and closed traumas (according to the anatomical area that was affected) n (%) | |||
|---|---|---|---|
| Gagliardi-Lugo et al. (Venezuela) | Hussaini et al.12 (Malaysia) | Zargar et al.7 (Iran) | |
| Frontal | 1432 (28.93) | (6.9) | – |
| Mental | 627 (12.66) | (15.7) | – |
| Nasal | 866 (17.49) | (10.4) | 35 (13.1) |
| Nasogenian | 548 (11.07) | (15) | 45 (16.8) |
| Lips | 501 (10.12) | (40.8) | 87 (32.5) |
| Orbital | 498 (10.06) | (10.8) | 61 (22.7) |
| Buccal mucosa | 237 (4.78) | – | – |
| Auricle and temporoparietal area | 240 (4.84) | – | 40 (14.9) |
Distribution by aetiology of odontogenic infections compared with the results from other studies.
| Odontogenic infections (according to aetiological factor) n (%) | ||
|---|---|---|
| Gagliardi-Lugo et al. (Venezuela) | Sánchez et al.15 (Spain) | |
| Cavities | 772 (64.17) | 51 (33.8) |
| Radicular remains | 402 (33.41) | – |
| Pericoronitis | – | 9 (5.9) |
| Alveolar osteitis | 29 (2.41) | 18 (11.9) |
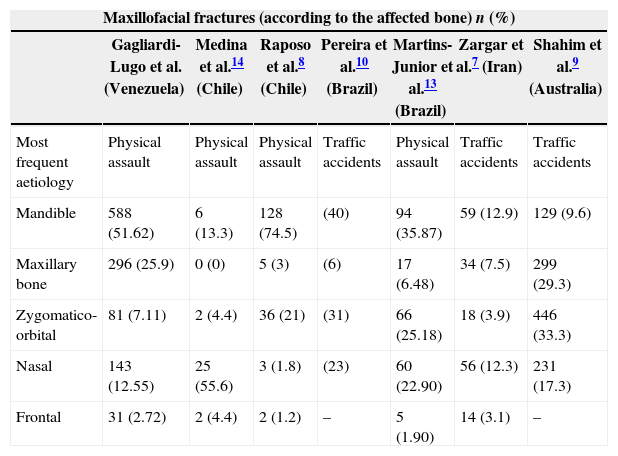
Distribution by affected bone in maxillofacial fractures compared with the results from other studies.
| Maxillofacial fractures (according to the affected bone) n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Gagliardi-Lugo et al. (Venezuela) | Medina et al.14 (Chile) | Raposo et al.8 (Chile) | Pereira et al.10 (Brazil) | Martins-Junior et al.13 (Brazil) | Zargar et al.7 (Iran) | Shahim et al.9 (Australia) | |
| Most frequent aetiology | Physical assault | Physical assault | Physical assault | Traffic accidents | Physical assault | Traffic accidents | Traffic accidents |
| Mandible | 588 (51.62) | 6 (13.3) | 128 (74.5) | (40) | 94 (35.87) | 59 (12.9) | 129 (9.6) |
| Maxillary bone | 296 (25.9) | 0 (0) | 5 (3) | (6) | 17 (6.48) | 34 (7.5) | 299 (29.3) |
| Zygomatico-orbital | 81 (7.11) | 2 (4.4) | 36 (21) | (31) | 66 (25.18) | 18 (3.9) | 446 (33.3) |
| Nasal | 143 (12.55) | 25 (55.6) | 3 (1.8) | (23) | 60 (22.90) | 56 (12.3) | 231 (17.3) |
| Frontal | 31 (2.72) | 2 (4.4) | 2 (1.2) | – | 5 (1.90) | 14 (3.1) | – |
The Bolivarian Republic of Venezuela is located on the Northern coast of South America; it covers 916,445km2 and has a population of 29,105,362 inhabitants, of which 2,903,285 are concentrated in the capital city, Santiago de León de Caracas.1 The city is comprised of five municipalities: Chacao, Sucre, El Hatillo, Baruta and Libertador. The HGO-BMFS is located in the north-western area of the city, in the district of Sucre. This district is subdivided into 13 sectors, one of which is Los Magallanes de Catia, hence the name of the hospital: “Hospital de los Magallanes de Catia”. Its construction was initiated by President Raul Leoni in 1968 and it was inaugurated by President Rafael Caldera in 1973.2
According to the Venezuelan Statistical Office, by 20011 the Sucre district had 352,040 inhabitants, of which 182,106 were females and 164,934 were males. The age of this population was between 15 and 60 years, with this range comprising at least 230,658 inhabitants.1,3
As for violence in Venezuela, according to a non-governmental organisation, there were 7960 homicides in 20013,4 and 19,336 homicides registered in 20114,5; this shows the increasing prevalence of an issue that affects the general population. According to these numbers, there has been a growth rate of 1000 homicides per year over the last decade, with an average of 1611 homicides per month, which breaks down to 53 homicides per day.4,5
The lack of safety and the increasing violence in Caracas has been reported by several organisations at national and international levels.3–6 The 2011 report from the United Nations Office for Drugs and Crime suggests that this issue is associated with the consumption and production of drugs in the country. The report also showed a reduction in violent crime in Colombia due to anti-drug campaigns implemented by the government over the past ten years. Similarly, there has been an inverse relationship in Venezuela where there was a rapid growth in violence between 1995 and 2010, even greater than in other countries such as Ecuador and Bolivia (which have also displayed minor growth).5,7
There are more females than males in the Sucre district population, however, males are worst affected. This agrees with the results obtained by other studies around the world.8–12 Pereira et al. analysed the clinical records of 521 patients with maxillofacial trauma in Goiana (Brazil), of which 412 (79.07%) were males.10 Other research studies from around the world also show this trend. Shahim et al. analysed data from 4430 patients with maxillofacial trauma in the state of Victoria (Australia) and identified that 73% of the affected patients were males.10 Zargar et al., from the city of Tehran, reported maxillofacial trauma as a ratio of 4.5:1 for males and females respectively.13 In Malaysia, Hussaini reported that 73% of the cases were males.12 A disproportionate tendency skewed towards the male gender can be observed, which demonstrates that men are more prone to suffering maxillofacial traumas, regardless of cultural, political or economical class.9,10,13,14
The age range most affected in our population was between 16 and 30 years old. These results seem to agree with others reported worldwide, for example, Martins-Junior et al., in Brazil, reported an average age of 29.6 years14; Pereira, also in Brazil, reported a range of 21–39 years10; the Tehran group reported a mean of 30.2 years,13 and the Australian group reported a predominance in the range between the age of 15 and 24 years. Adolescence and adulthood appear to influence the susceptibility of the male gender to maxillofacial traumas, perhaps because of the freedom that these individuals attain at this time.9,10,12 This led us to perform an aetiology analysis of the traumas which, although not registered in our study, allows us to confirm that violence due to robbery, street fighting and domestic violence was the commonest cause, followed by traffic accidents. Pereira's study in Brazil reported a predominance in traffic accidents followed by violence10; the group from Tehran reported traffic accidents followed by falling from a height13 and the group from Australia also reported traffic accidents as the primary cause.10 Martins-Junior et al. in Brazil reported physical aggression as the main cause of maxillofacial traumas,14 as did Raposo et al. in Chile.8 This agrees with our study. The hospital where we conducted the study is located in a popular area in which crime rates have increased. This coincides with the increase in violent incidents over the last few years. In our analysis, an increase in maxillofacial traumas was evidenced at our emergency room between 2006 and 2012.4,5,7
In our study, the main reason for consultations was wounds or open and closed traumas mainly affecting the frontal area. Hussaini et al. reported that, in the population studied in Malaysia, 23% of the cases affected the upper lip, followed by the lower lip in 18% of the cases, closely followed by the cerebral region in 16% of the cases and the nose in 10%. The frontal area was last, in only 7% of the cases.12 The significant difference between our results and the results in Malaysia is notable, since the patterns are complete opposites: in our study, the lips were the fifth most affected area amongst soft tissues, whereas the nasal and the cerebral area were second and third, respectively (Table 2). The most common aetiology reported by Hussaini was, once again, traffic accidents.12 Hussaini's results agree with the group in Iran, where they report that wounds to soft tissues were predominant in the lips and the buccal cavity13 followed by the eyelids and the periorbital area. Both authors reported traffic accidents as the most common aetiology.12,13
As for the most reported maxillofacial fractures, Shahim and his team in Australia reported a higher incidence of fractures in the zygomatico-orbital complex, followed by the maxillary bone and the nasal bones9; these results agree with the findings reported by Pereira and his team in Brazil, with a higher incidence (30%) of cases in the zygomatico-orbital complex and 23% in the nasal bones.10 Raposo et al. reported a higher incidence of fractures to the mandible.8 The main aetiology of all the studies was traffic accidents.8–10 Martins-Junior and his team in Brazil also reported a higher incidence of cases of mandible fractures (n=90).14 The Raposo et al. and Martins-Junior et al. results agree with our study, where the main reason for consultation was physical aggression and the largest incidence of fractures was to the mandibles. There seems to be an association between the reason for consultation and the bones fractured: traffic accidents tend to generate fractures in the medial third of the face,9,10,13 while violence and physical aggression tends to generate fractures in the lower third of the face.8,14 However, it is noteworthy that Zargar and his team in Iran reported a high rate of mandible fractures associated with traffic accidents13 and, conversely, Medina et al. in Chile reported a higher incidence of zygomatico-orbital fractures associated with physical aggression15 (Table 4).
This research study is the only one in the literature consulted that includes odontogenic infections in the analysis of reasons for emergency consultation. Within our results, odontogenic infections were the second most common reason for consultation at the hospital's emergency room. Sánchez et al. reported that odontogenic infections represent the first reason for emergency consultations at all dental practices and that they represent 10% of the prescriptions for antibiotics in Spain.15 If odontogenic infections are not treated at an early stage then they can lead to complications, to the point that the patient's life could be at risk, and they can present as actual maxillofacial emergencies, such as Ludwig's Angina16 or Lemierre's Syndrome.17 Sánchez et al. reported an average age of 40 years in a total of 151 patients with odontogenic infections, of which 81 were hospitalised. The main reasons for odontogenic infection were cavities, in 33.8% of the cases, followed by postoperative periods after dental extractions and pericoronitis.15 These results agree with our study, where dental cavities represented the main aetiology in 64.17% (n=772) of the registered cases, followed by the existence of radicular remains in 33.41% (n=402) of the cases; pericoronitis was included along with cavities since in all these cases the third molar presented cavities associated with pericoronitis processes. However, this latter group represents a significant aetiological factor akin to that referred to by Haug et al. in their study, where pericoronitis was the main aetiological factor for odontogenic infections18 (Table 3). Due to the limited literature specific to this topic, further research into the epidemiology of odontogenic infections is recommended.
ConclusionThe male population between the ages of 16 and 30 years from Western Caracas was most susceptible to suffering open or closed traumas in the soft tissues of the maxillofacial area, particularly in the frontal and nasal areas. The second most frequent reason for attending an emergency room was odontogenic infections, mainly caused by cavities. Lastly, the mandible bone is the most prone to suffering fractures in situations of physical aggression, followed by the maxillary bone.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe aforementioned authors certify that there are no conflicts of interest of a financial or personal nature regarding other people or organisations. This study did not require any kind of external funding.
To all the postgraduate Buccal and Maxillofacial Surgery members; to the medical, nursing, administrative and maintenance staff from the Hospital General del Oeste Dr. José Gregorio Hernández, Los Magallanes de Catia, Caracas (Venezuela). Particularly to those who helped to carry out this study, Od. Rafael Zeballos Peltrini, Od. María Daniela Viamonte, Od. Sandra D’Caro and Od. Pablo Colmenares.
Please cite this article as: Gagliardi Lugo AF, Contreras Ravago MG, Gudiño Martinez RA. Motivo de consulta de urgencias por cirugía maxilofacial en un hospital venezolano desde 2006 hasta 2012. Estudio retrospectivo. Rev Esp Cir Oral Maxilofac. 2015;37:215–219.