Systemic lupus erythematosus (SLE) exposes patients to physical, psychological, family, work and social stress factors. The health-related quality of life of these patients is less than that of the general population, and stress is associated with worsening symptoms of SLE. Studying the factors that determine the perceptions of an SLE patient toward their disease would allow understanding the mechanisms by which quality of life is adversely affected, and promote interventions that ensure the well-being of these patients.
ObjectiveTo gain knowledge of the perceptions that SLE patients have regarding their disease.
MethodologyA total of 50 patients (11 of them men) participated in 5 focus groups that were guided by a psychiatrist applying a semi-structured interview. The interview transcripts were categorized into the following 3 phases using grounded theory: open, axial and selective coding.
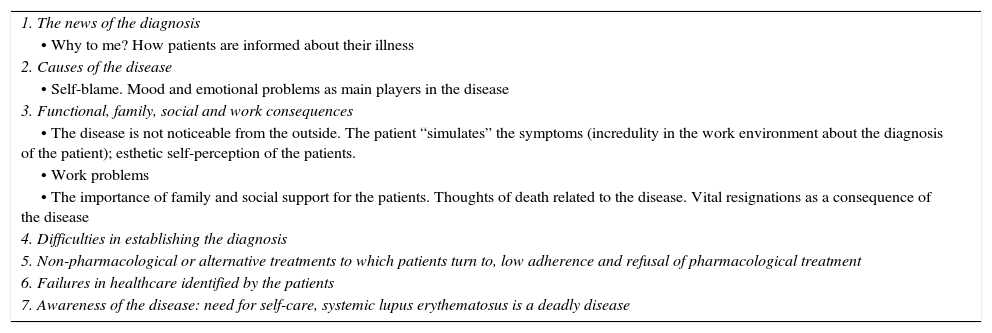
ResultsThe results were organized into 7 categories: news of the diagnosis; causes of the disease; functional, social and work consequences; difficulties in establishing a diagnosis; non-pharmacological, alternative treatments, low or non-adherence and rejection of drug treatment; weaknesses in health care identified by the patient; and disease awareness.
ConclusionsKnowing the perception that SLE patients have of their disease allows the physician, the patient, and the patient's family to take steps toward designing timely and effective interventions for integrated disease management, treatment adherence, and reducing the associated morbidity and costs of medical care.
El lupus eritematoso sistémico (LES) es una enfermedad crónica que expone a los pacientes a situaciones estresantes físicas, psíquicas, familiares, laborales y sociales. Se conoce que la calidad de vida relacionada con la salud de estos pacientes es inferior a la de la población general y que el estrés está relacionado con el empeoramiento del LES. El estudio de los factores que determinan la percepción del paciente con LES permitiría conocer los mecanismos que inciden negativamente en la calidad de vida y promover intervenciones que conlleven su mejoría.
ObjetivoConocer la percepción que los pacientes con LES tienen acerca de su enfermedad.
MetodologíaCincuenta pacientes (11 hombres) con LES y sin otras enfermedades autoinmunes participaron en 5 grupos focales, realizados por un médico psiquiatra mediante la aplicación de entrevista semiestructurada. Utilizando la teoría fundamentada, las transcripciones fueron categorizadas en 3 fases: codificación abierta, axial y selectiva.
ResultadosSe organizaron en 7 categorías: noticia del diagnóstico; causas de la enfermedad; consecuencias funcionales, sociales y laborales; dificultades para establecer el diagnóstico; los tratamientos no farmacológicos o alternativos; baja adherencia y rechazo al tratamiento farmacológico; fallas identificadas por los pacientes en la atención en salud y conciencia de la enfermedad.
ConclusionesEl conocer la percepción que tiene el paciente con LES de su enfermedad les permite al médico, al paciente y a su familia adoptar medidas encaminadas a diseñar intervenciones puntuales y eficaces para el manejo integral, adherencia al tratamiento, disminución de morbilidad asociada y de costos derivados de la atención médica.
Systemic lupus erythematosus (SLE) is an autoimmune, chronic, multisystem and complex disease that is associated with a significant economic burden related to the use of resources invested in health care and the loss of productivity of the patient and the caregiver. The prevalence in the United States is 52/100,000 inhabitants, 21/100,000 in Canada and 25–91/100,000 in Europe.1 The epidemiology in Latin America has been little studied; however, it is known that the disease is more severe in patients of Hispanic origin, low socio-economic strata and lower educational level, with greater renal involvement and mortality than in Caucasian patients.2–4
The clinical evolution of SLE is unpredictable, undulating in time with clinical manifestations and sequels that can affect the physical function and the quality of life.3,5 The above may result in increased morbidity and mortality through accumulated damage in multiple organs and systems. The alteration in the physical, personal, social and family aspects of the patients with SLE can significantly compromise the control of the disease activity, generating higher morbidity and mortality.6
Dealing with a chronic disease like SLE constitutes a major challenge for the patient and his family environment. Those who suffer from the disease must confront various stressful situations such as frequent medical evaluations, visits to the hospital, side effects of the treatment, pain, fatigue and anxiety. The above increases the risk of developing behavioral, social and emotional alterations.7,8
The perception of the disease is mainly cognitive, which influences the emotional response of the patient to his illness and his behavior to cope with it.9 Patients with SLE have representations about their disease, which they elaborate through experiences lived personally or by third parties. For these reasons, it is justified to try to know which is the perception that people have of their disease, especially the cognitive (identity, consequences and duration of the disease, personal control and effectiveness of the treatment) and emotional (awareness about the disease, generated emotions and understanding thereof). The perception of the disease has a direct relationship with the individual's ability to make positive changes toward health protective behaviors and the adequate adherence to treatment, with which is possible to have a better control of the disease and a positive impact on the quality of life.7,9,10
Since 1980, Howard Leventhal developed the model of self-regulation of the disease, which gives rise to the concept of perception of the disease as it is currently known. His model proposes that a stimulus (symptom) generates a cognitive representation, an emotional representation of the disease, that is translated into a treat to health and, therefore, obliges the individual to adopt different behaviors or coping strategies.11,12
The objective of this study is to know the perception of the disease in patients with SLE through the realization of focus groups.
Materials and methodsThe study was conducted in patients older than 18 years with diagnosis of SLE, according to the criteria of the American College of Rheumatology (ACR 1997), evaluated in 2 medical centers of the city of Bogota (Clinic University of la Sabana and Central Military Hospital). In order to achieve the intended objective it was raised a qualitative study based on the grounded theory, methodology that arises from the symbolic interactionism and seeks to develop the theory starting from the data that emerge from the experiences lived by the patients with SLE, focusing on the perception of the disease. These data are captured and analyzed systematically. The perception was measured through the formation of focus groups guided by a specialist in psychiatry with previous experience in the methodology, applying semi-structured interviews. The inclusion criteria were: age over 18 years, diagnosis of SLE, absence of another rheumatic disease, desire to participate in the study and signature of the informed consent. All patients who were unable to attend the scheduled meetings were excluded.
Each focus group was made up of 10 patients with a duration of 2h, for a total of 5 focal groups (n=50 patients). The sample size was obtained by saturation. Using the grounded theory, the transcripts were categorized into 3 phases: open, axial and selective coding. 3 authors intervened in the analysis of these categories.
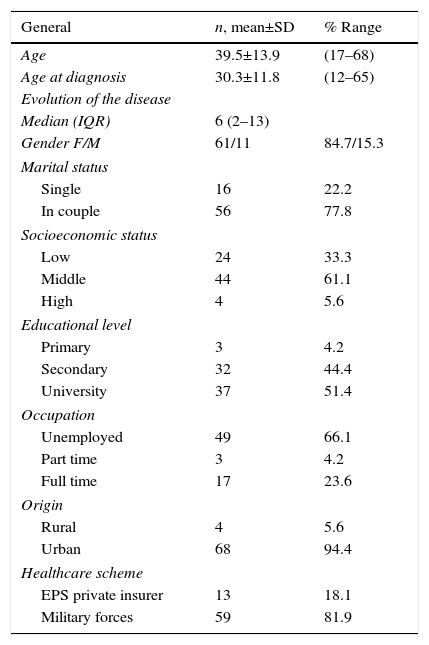
Results50 patients entered the study, 78% were women with a mean age of 39.5±13.9 years and a median duration of the disease of 6 years. 61% belonged to middle social class and 88.8% had high school and university studies. The sociodemographic characteristics of the study population are summarized in Table 1. After the realization of 5 focus groups the axial categories recorded in Table 2 were obtained. Below is an overview of the categories analyzed.
Sociodemographic characteristics.
| General | n, mean±SD | % Range |
|---|---|---|
| Age | 39.5±13.9 | (17–68) |
| Age at diagnosis | 30.3±11.8 | (12–65) |
| Evolution of the disease | ||
| Median (IQR) | 6 (2–13) | |
| Gender F/M | 61/11 | 84.7/15.3 |
| Marital status | ||
| Single | 16 | 22.2 |
| In couple | 56 | 77.8 |
| Socioeconomic status | ||
| Low | 24 | 33.3 |
| Middle | 44 | 61.1 |
| High | 4 | 5.6 |
| Educational level | ||
| Primary | 3 | 4.2 |
| Secondary | 32 | 44.4 |
| University | 37 | 51.4 |
| Occupation | ||
| Unemployed | 49 | 66.1 |
| Part time | 3 | 4.2 |
| Full time | 17 | 23.6 |
| Origin | ||
| Rural | 4 | 5.6 |
| Urban | 68 | 94.4 |
| Healthcare scheme | ||
| EPS private insurer | 13 | 18.1 |
| Military forces | 59 | 81.9 |
SD: standard deviation; IQR: interquartile range.
Axial categories.
| 1. The news of the diagnosis |
| • Why to me? How patients are informed about their illness |
| 2. Causes of the disease |
| • Self-blame. Mood and emotional problems as main players in the disease |
| 3. Functional, family, social and work consequences |
| • The disease is not noticeable from the outside. The patient “simulates” the symptoms (incredulity in the work environment about the diagnosis of the patient); esthetic self-perception of the patients. |
| • Work problems |
| • The importance of family and social support for the patients. Thoughts of death related to the disease. Vital resignations as a consequence of the disease |
| 4. Difficulties in establishing the diagnosis |
| 5. Non-pharmacological or alternative treatments to which patients turn to, low adherence and refusal of pharmacological treatment |
| 6. Failures in healthcare identified by the patients |
| 7. Awareness of the disease: need for self-care, systemic lupus erythematosus is a deadly disease |
At the time of receiving the diagnosis of the disease the patients have a significant emotional shock, only the name “lupus” generates fear to some of them and the sensation that they should get everything ready in their lives in case they should die; in some cases they have seen it as another member of their life or their family.
As soon as the diagnosis of SLE is confirmed and the patients begin to have a more precise idea of the implications of the disease and its potential effects, they begin to question themselves and to review what they have done in their lives to suffer from this disease. “Why to me?” is an internal question that removes them all their history, their mistakes and the emotional wounds that have remained unhealed.
It is also a question to life and to their God, a question to the destiny looking for an explanation. In the elaboration of their grief, they think that the disease is a punishment and that there must exist some material or metaphysical reason that explains why something infrequent happened to them. Although this situation occurs, mainly, at the beginning of the disease, even several years after the diagnosis the patients continue wondering the reason why they got this disease; they question themselves why, they say they do not deserve the condition that they are going through. Regarding how patients are informed, it was found that the great majority of the participating patients agree that at the time of diagnosis the physician was not clear with the explanation about what is SLE, its causes and how to treat it. Some of them turned to Internet, where they got more confusing and worrying answers. Many of them, to date, tell that they have been learning about it little by little in each medical appointment. The reports of the patients about how the doctors explained them the diagnosis ranged from the fact that some of them simply restrict the information, and others, even though they explain it widely; they do not do so in terms that the patient can understand.
Causes of the diseaseThe disease is not noticeable from the outside. The patient “simulates” the symptoms.
In that race for understanding the reason that explains why they are affected by a serious, chronic and probably deadly disease, they begin to look for associations related in time with the emergence of the SLE or situations so atypical or intense that would explain this disease.
The patients identify diverse factors as the direct or indirect causes of the disease, some of them, who are better informed, give meaning to pathophysiological and environmental explanations, such as inheritance, eating habits or environmental pollution. Others, for their part, attribute it to emotional and family problems; they have even magical explanations such as witchcraft and divine punishment.
The great majority of patients agree that they have SLE because they did something wrong in the past, that perhaps they are paying for some bad action toward their friends, their family, themselves or to their God. Some of them think that because they were sad and had a bad attitude, their own body could attack them and hence the onset of the disease.
The patients identify low mood and emotional problems as a direct cause of the generation or worsening of SLE.
Functional, social and work consequencesWhen the disease does not produce clinical manifestations visible to others, is controlled or in mild to moderate activity, the patients agree in affirm that at some point they have been labeled as liars or simulators. The other people have not believed that they suffer from the disease. This was more visible in the focus groups conducted with patients belonging to the military forces, who due to their militia ideology must always demonstrate character and never tiredness or weakness, to the point that some patients felt violated by their superiors.
Many patients interviewed say that their family and coworkers only believed them that they were really sick when they presented severe manifestations of the disease that led them to prolonged hospitalizations and, of course, to labor incapacities.
The esthetic self-perception of the patientsAll patients, at some point, have experienced a change in their body such as increased body hair, weight gain, stretch marks or skin lesions, which caused them problems with the perception of their body image and self-esteem, to the point of isolating themselves from every activity of daily life which would imply contact with other people in order to avoid being judged or ridiculed. These problems with the body image were more noticeable in the woman of the study and during their stage of adolescence.
Work problemsWork problems are caused by the work absenteeism generated by the disease when it is active (incapacities), added to the fact that it is a disease not easily recognizable from the outside by other people, causing that bosses or co-workers do not believe they are sick, reject them, subject them to long work days or even, sometimes, do not respect them their medical incapacities as reported by some patients.
The importance of family and social support for the patientsAll patients interviewed in the focus groups agreed that something worse that not having family who would support them was to expect this support from the family and do not obtain it. A great part of the patients, at some point, have felt themselves abandoned by their family group, by friends, by the society in general. While some of them already have this support so longed for, there are others who are still facing the disease alone.
Positive aspects that they identify when they are sickNot everything has been negative since the diagnosis of the disease in the patients studied, because over time they have managed to find some positive factor in relation to strengthening their family ties.
Vital resignations as a consequence of the diseaseThe patients with SLE may have some degree of temporary or permanent limitation, which depending on the affected organ can be more or less disabling. A clear example is the arthritis, which prevents patients from carrying out activities of daily living and, depending on the occupation or trade carried out, it can become an obstacle not only personal but in their professional life.
Thoughts of death related to the diseaseIn patients with SLE is frequent the coexistence of mood disorders, either due to the disease per se or because of the reaction to the diagnosis which is manifested, sometimes, with wishes of death and “rest”.
Difficulties in establishing a diagnosisMany of the patients who attended the focus groups felt themselves disconcerted when they saw that for several months or even years, their symptoms did not have a logical explanation for them and even for the physicians to whom they turned to. After time and the realization of several paraclinical exams, the diagnosis was reached.
Non-pharmacological or alternative treatments to which patients turn toIn relation to this aspect, almost all patients have tried some type of alternative therapy or medication for the treatment of the lupus. The opinions about their effectiveness are divided since some patients believe that these have caused them well-being, although they have never suspended the medication formulated by their rheumatologist; while others say that these alternative therapies have brought them worse adverse effects and have complicated their illness. In what all patients agree is in the high costs of these alternative therapies.
For the patients that have experienced improvement with the alternative treatments, the benefit seems to come from the fact of feeling heard by a professional, of being able to find explanations for their disease and their symptoms, reducing stress, improving mood and feeling that leading a healthier lifestyle and with more self-care they can have greater vitality.
Low adherence and refusal of pharmacological treatmentThe patients who at some point have suspended their pharmacological treatment have done so because of the side effects, mainly those related to antimalarials at the gastrointestinal level and to glucocorticoids such as overweight, acne, iatrogenic Cushing, gastrointestinal disorders and, in other cases, due to clinical manifestations that are not of the drug but they attribute them to it. Other patients have discontinued their medication because they feel that when the disease is inactive they do not need it anymore.
Failures in healthcare identified by the patientsThe main complaints of the patients are regarding the opportunity for appointments with rheumatology, the delivery of medications, the availability of resources for the realization of laboratory tests and the administrative arrangements, in general, to which they are subjected after being seen in consultation. Finally, another complaint of a few patients is the indifferent attitude of some doctors and of the healthcare service providers.
Awareness of the disease: need for self-care, lupus a deadly diseaseAs the patients know more about their disease, they become aware of the importance of self-care, of looking after their own well-being, and taking measures aimed to their protection in order to avoid relapses and possible negative consequences and even death.
Systemic lupus erythematosus, a deadly diseaseAll patients seen in the focus groups consider that SLE is a fatal disease and that it will be the cause of their death. To some extent they express hopelessness about the distant future.
DiscussionDespite the recognition of SLE as a serious illness with a significant impact on the live of the patients, in whom the depressive disorder can be found in up to 39% and the anxiety as a reaction to the diagnosis in 24% of them,13 few studies have evaluated the psychological functioning of the sick people. There are only few studies evaluating the perception of the disease, which are not comparable with each other given their methodological differences.6,14–17
This study was carried out in a diverse population of patients with SLE, of both sexes, different ages, different time of evolution and heterogeneous clinical manifestations.
The representation of the disease and its perception are consistent with Leventhal's self-regulation model. Within the selected categories can be identified components such as the identity in the first category, where the patients, only with the name “lupus” have significant emotional reactions, or when they refer to the symptoms of the disease or to the adverse effects caused with the treatment. Regarding the causes, self-blame was previously mentioned, it is also noteworthy that many of the patients identify the stress at all levels (family, work, social) as an important cause of the disease. This same factor was found in a qualitative study on the emotional representations of the patients with SLE, where they stated that the stress was the main cause of their disease14 and in another one more recent that explored the perception of the disease in patients with lupus nephritis.6
The answers of the participants to the questions about the consequences of SLE in their lives, the lives of other significant persons and the future were very detailed. The great majority expressed negative consequences in all aspects of their lives and only a few patients found something positive in the fact of having SLE. One of the interesting negative aspects is the esthetic self-perception, which was more striking in female patients, especially in those in whom the disease began in adolescence. In this regard, the literature in SLE is scarce; however, some authors coincide with what was found by us, evidencing that the body image is impaired in the patients with SLE and is inferior to that of the people who do not suffer from the disease, especially in those with cutaneous involvement and depression.18
All the participants in our study agreed that they are not given enough information about the disease at the time of diagnosis and they would like that the health care personnel would be more involved in the education of the patients. These findings are consistent with a recently published study, where they conducted focus groups in 28 women with SLE in order to design an intervention to improve the health care and the quality of life of these patients; like our patients, they pointed out the need for education to the patient and his family. In this article is raised even the creation of “passports” (information cards) and “counselors”, individuals who would educate them and accompany them through their disease.19
Finally, the current weaknesses of the Colombian healthcare system are reflected in the difficulties for timely access to medical evaluations by Rheumatology, diagnostic studies and appropriate treatments. All this problems are corroborated by national studies such as the one conducted by the Ombudsman Office in 2009, on the users satisfaction index, which demonstrates that at some point 22.9% of users have had problems with the dispensation of drugs (partial or never made delivery). Regarding the opportunity for specialized medical appointments, this study reports an average of 18.6 days, which is in contraposition with what was experienced by our patients, although the study does not discriminate between the different specialties. The same happens in the accomplishment of laboratory tests and diagnostic images for which the Ombudsman Office reports 3.7 and 8.4 days, respectively.20
ConclusionsSLE as a disease closely related to death that requires interdisciplinary management and psychological support to the patient and his family, from the moment of diagnosis and during its course, which accompanies the patient and explains him and those who are closest to him everything concerning the disease, in order to generate an adequate doctor-patient relationship, a complete and accurate understanding of the disease, and thus promote a good adherence to treatment, which may impact the outcomes. Decision-making in the healthcare sector should take into account the perception of the patients, supported by scientific basis, which considers, in addition to the classical quantitative indicators (mortality, morbidity, life expectancy) and the costs, the qualitative indicators, such as the perception of the disease that expresses the impact on the quality of life and satisfaction of the patient.
While there is little evidence on whether the perception of the disease can change with treatment, specifically with cognitive behavioral therapy as some have suggested,15 the incorporation of tools of evaluation of the perception of the disease is required in all patients with SLE. It is necessary to explore if the representations of the disease can predict the response to the interventions, and if so, to generate health policies for the patients, their families and attending physicians, which are aimed at a total understanding of the biopsychosocial being in order to avoid complications, sometimes fatal, reduce healthcare costs and generate an optimal health-related quality of life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Valencia P, Mora C, Rossinni Y, Arbeláez AM, Plazas M, Londoño J. Análisis de grupos focales en pacientes colombianos con lupus eritematoso sistémico: una mirada cualitativa a las representaciones de la enfermedad. Rev Colomb Reumatol. 2017;24:11–17.