Immune encephalitis is a diverse group of disorders that share some unique diagnostic approaches and specific treatments. Some of the initial manifestations are non-specific and difficult to distinguish from encephalitis of other aetiologies, and even with modern diagnostic tools there are still a number of cases for which definitive causes cannot be clarified. Among these, N-methyl-d-aspartate receptor (NMDAR) encephalitis is a particular form of immune encephalitis that has some distinctive clinical manifestations, which allows the clinical evaluator to suggest a more accurate diagnosis and start treatments even in the absence of specific laboratory tests. Three paediatric patients, who were treated for NMDAR encephalitis are described in this article, as well as comparing their clinical presentation. This specific disorder and some of the more relevant features of its physiopathology are reviewed in order to explain the initial psychiatric manifestations, for which early recognition is critical for an appropriate diagnosis and treatment.
Las encefalitis inmunitarias son un grupo particular de trastornos que se distinguen por su aproximación diagnostica única y manejo específico. Algunas de las manifestaciones iniciales son inespecíficas y difíciles de distinguir de encefalitis de otros orígenes, e incluso con los tests diagnósticos modernos aún hay cierto número de casos en que no se logra aclarar la causa específica. Entre ellas, las encefalitis anti-NMDAR son una particular forma de encefalitis inmunitaria que tiene manifestaciones clínicas distintivas, algunas de las cuales permiten al evaluador médico apuntar a un diagnóstico más preciso e iniciar tratamientos aun sin tener los reportes específicos de laboratorio. En este artículo se presentan 3 casos de pacientes pediátricos tratados como encefalitis anti-NMDAR, y después de comparar su presentación clínica, se revisa este trastorno específico y algunos de los datos más relevantes en su fisiopatología, como una forma de explicar las manifestaciones psiquiátricas iniciales, de cuyo reconocimiento inicial van a depender los apropiados diagnóstico y tratamiento.
Autoimmune encephalitis is a heterogeneous group of neurological diseases that share some unique diagnostic approaches and specific treatments, and should be included in the differential diagnosis of patients with acute or subacute symptoms of encephalitis.1 Although the presenting symptoms of the different types of encephalitis will indicate the correct diagnosis, they will not clearly show the aetiology of the condition, particularly in view of the great variety of nosological agents that cause encephalitis and the fact that a specific microbiological agent cannot be identified in many cases, despite the progress made in technology and analytical techniques.2 For this reason, it is important to take into account the presence of certain clinical variables together with factors reported in the patient's medical history that could suggest a specific cause and thus reorient the diagnostic and treatment algorithms.
Anti-NMDAR encephalitis is a relatively recently described type of encephalitis. It initially presents with a series of neuropsychiatric manifestations that, for those unfamiliar with this clinical entity, are diagnostically unspecific until more obvious neurological symptoms appear. For this reason, therapy is often delayed.1 In this article, we present the initial manifestations of 3 cases of anti-NMDAR encephalitis in the city of Cali, Colombia. We illustrate the variability of symptoms, compare them with those described in the medical literature so far, and assess the role of NMDAR and NMDAR antibodies in the appearance of the wide variety of symptoms associated with this disease.
Case 1A 9-year-old boy who consulted for a 5-day history of emotional lability and unmotivated crying, followed by progressive mutism. The symptoms were associated with mild headache, with no other neurological or alarm signs. The parents did not report fever or other constitutional symptoms that would indicate infection at the onset of the condition. He was initially assessed by the paediatric neurologist, who consulted with psychiatry due to a suspicion of acute anxiety.
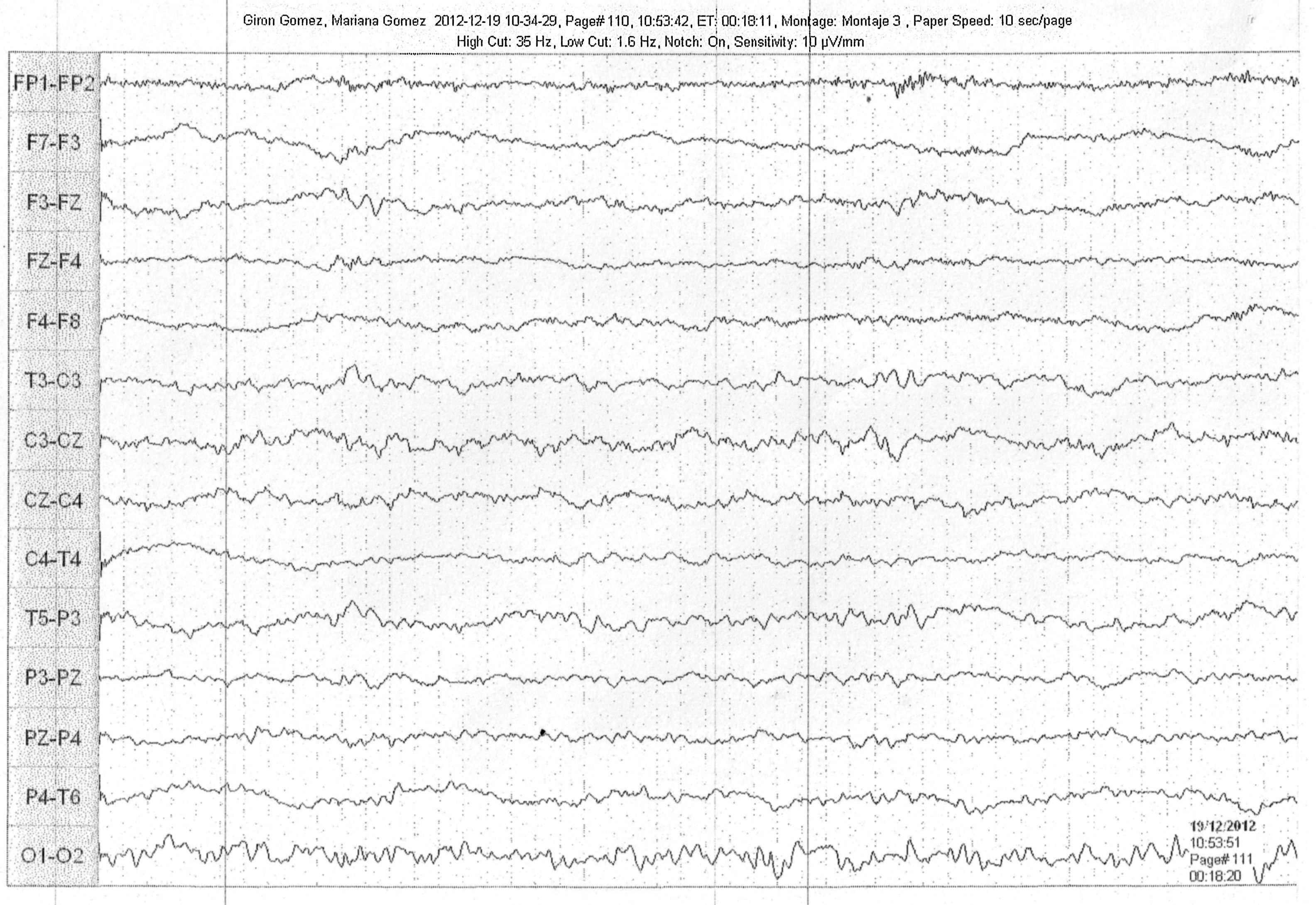
One week later, the patient presented orofacial dyskinesias and choreiform hand movements. This was followed by sleeping difficulties and dysautonomic changes with labile hypertension, followed by progressively impaired consciousness. The electroencephalograms (EEG) performed showed abnormal patterns and slowing. Neuroimaging studies did not identify structural alterations, and CSF studies showed pleocytosis, with no other findings. Due to clinical suspicion of autoimmune anti-NMDAR encephalitis, the patient was treated with pulsed administration of immunoglobulin, systemic steroids and symptomatic treatment with haloperidol and risperidone. The patient showed gradual recovery of consciousness and remission of abnormal and dysautonomic movements, and was discharged approximately 2 months after admission.
In this case the initial diagnosis was infection-related encephalitis, and the patient received broad-spectrum antibiotics and antivirals until infection was ruled out by negative cultures and specific serological tests for infectious disease. The clinical suspicion was reached on the basis of a sequential analysis of the case (acute psychiatric manifestations, followed by abnormal movements and progressively decreased level of consciousness) and by elimination of other more prevalent conditions, such as infection. We did not have access to laboratories capable of determining anti-NMDAR antibodies during the diagnostic process, so this test was not performed.
Case 2A 7-year-old girl consulted for a 1-week history of subjective difficulty in moving the lower limbs, which gradually became progressive and limited her gait and mobility. No other clinical symptoms or signs of infection at the onset of the problem were reported. The patient appeared able to move her lower limbs during provocative manoeuvres, despite her inability to walk. Imaging studies of the brain and spine and electrophysiological evaluation of peripheral nerves were normal.
Somatisation disorder was suspected, so her attending physician consulted with psychiatry and treatment with anxiolytics was started. Despite the treatment, the patient's symptoms had worsened over the course of a week, with onset of agitation and aggressiveness, along with orofacial dyskinesias and paroxysmal clinical events explained as seizures, followed by insomnia, intermittent dysthermia and hypertension, eventually culminating in stupor and coma (Fig. 1). EEG studies showed a pattern of generalised slowing along with focal epileptogenic activity; CSF studies were normal, except for mild pleocytosis, with no other findings or isolation of infectious agents. An analysis of the case led to suspicion of anti-NMDAR encephalitis, and the patient was treated with pulsed steroids and immunoglobulin, and was admitted to the intensive care unit due to neuromuscular respiratory failure and the need for anticonvulsants to treat recurrent seizures. After about 3 weeks, the patient awoke from her coma. She initially required enteral nutrition due to a swallowing disorder, which was later withdrawn, and she was discharged after 3 months.
In this case, the initial diagnosis, due to a high degree of suspicion, was autoimmune encephalitis, and the evolution of the clinical manifestations (acute manifestations of conversion disorder followed by abnormal movements, convulsions, abnormal sleep patterns, dysautonomia and progressively impaired consciousness) rapidly raised suspicion of anti-NMDAR encephalitis. For this reason, the patient did not receive antibiotics or antivirals after specific culture and serological tests ruled out the presence of infection. In this case, other conditions, such as metabolic disorders (tests for ammonium, lactate, urinary excretion of amino acids) and systemic autoimmune diseases (antinuclear antibody panel for lupus erythematosus, rheumatoid arthritis and serum complement determination, among others) were ruled out. The diagnostic strategy included determination of anti-NMDAR antibodies, but it was not possible to send the sample due to administrative problems with the insurance company, so the diagnosis was clinical from the outset, as was the decision to start immunotherapy. During her stay, the patient underwent a pelvic ultrasound to rule out the presence of an ovarian tumour.
Case 3A 5-year-old boy who had not previously presented any abnormalities was brought to the emergency department due to rapid behavioural changes, with unmotivated aggressiveness, marked impulsivity and mutism, which progressed to isolation. The parents also described an unclear event that suggested a partial, isolated seizure that did not occur at a later stage, but was followed 2–3 days later by choreiform movements, multifocal dyskinesias and agitation that progressed to drowsiness, stupor and coma. For this reason, the patient was transferred to the intensive care unit. The EEG showed a pattern of generalised slowing; neuroimaging and CSF studies were normal. Empirical antibiotic treatment elicited no response, so it was decided, on suspicion of anti-NMDAR encephalitis, to administer systemic steroids and pulsed immunoglobulin. Despite the treatment, no neurological improvement was observed, and tracheostomy and gastrostomy were also required. In view of the situation, it was decided to add pulsed administration of immunoglobulin, plasmapheresis, and finally rituximab, which achieved gradual stabilisation and slow improvement in the level of consciousness, with remission of abnormal movements and gradual functional recovery. The patient was discharged after 4 months.
In this case, the initial diagnosis was also based on a high degree of suspicion, and although the patient received antibiotic and antiviral treatment for infectious encephalitis, these were promptly withdrawn due to the evolution of the clinical manifestations (disruptive behaviour and mutism along with seizures, followed by abnormal movements, which gradually progressed to impaired consciousness and eventually coma, at which point ventilatory support was indicated) and the negative results of cultures and serological tests for infection. As in case 2, systemic autoimmune diseases were ruled out, and abdominal ultrasound and imaging studies also helped rule out the presence of tumoural disease. Due to the high suspicion of anti-NMDAR encephalitis, a sample was sent to an outside laboratory for antibody testing. The results, received several weeks after onset of the symptoms, were positive for high levels of NMDAR antibodies. In this case, immunotherapy was started on the basis of the clinical diagnosis, without waiting for the lab report.
DiscussionThe NMDA receptor is a cation channel involved in synaptic transmission. It is a heteromeric complex with glutamate and glycine binding sites. Overexpression of NMDA receptors is associated with epilepsy, dementia and stroke, whereas low expression produces symptoms of schizophrenia.3 Due to their widespread distribution across the brain, blockade of NMDA receptors produces several different effects: when their activity is reduced by specific antibodies and synaptic NMDA receptor-mediated currents are eliminated, GABAergic neurons innervated by glutaminergic synapses lose this excitatory effect, leading to disinhibition of excitatory pathways and increased levels of extracellular glutamate.4 This disturbance in the striate cortex manifests as psychosis, catatonia, mutism and dystonia, while orofacial dyskinesias and other involuntary movements are explained by the disinhibition of the central pattern generators located in the brain stem. Impairment of the dopaminergic and noradrenergic systems explains the dysautonomia, and the respiratory depression is thought to be caused by the antibody activity on the ponto-medullary respiratory network.1
Because the initial symptoms of anti-NMDAR encephalitis are primarily neuropsychiatric, definitive diagnosis is often delayed because patients are usually seen by clinicians who do not consider this diagnosis until other neurological symptoms appear.2 Considering that prognosis worsens the longer treatment is delayed (specifically immunotherapy), a high level of suspicion is crucial to achieve diagnosis.
While early descriptions emphasised psychotic behaviour as the first psychiatric manifestation of this condition,5 more recent studies report a variety of behavioural symptoms, such as anxiety, insomnia, unmotivated fear, grandiose delusions, hyper-religiosity, mania and paranoia. Social withdrawal and stereotypical behaviour are less frequently observed.6 However, these should be taken into consideration, particularly in young children, in whom the initial symptoms may be more difficult to identify due to their inability to express their thoughts and their tendency to present temper tantrums, hyperactivity or irritability, rather than frank psychosis.7
It can be difficult to differentiate between the typical presenting symptoms of this condition and symptoms characteristic of other, exclusively psychiatric, disorders. In these situations, the following considerations can be helpful: conversion or dissociative disorders are rare in infancy, and most suspected cases do not present the required number of symptoms to meet the diagnostic criteria, or are extremely uncommon. Diagnosis is by exclusion, and is only guided by the temporal relationship between the physical symptoms and certain stressful life events.
A less frequent manifestation of conversion disorders is denial of anxiety while manifesting anger, aggressiveness, perfectionism and high personal expectations. Patients are self-sufficient, highly responsible, with an apparently problem-free family life, and denial of family conflicts. They are hypervigilant, and alert to bodily sensations they perceive as alarming. Most are very concerned about their symptoms, and it is important to consider the existence of a secondary gain, since all children get more attention when they are ill. It is also useful to enquire about similar symptoms or disability in another family member, who may be the “role model” for the child's symptoms. In the 3 cases reviewed in this article, the initial manifestations, though varied, shared certain elements: abrupt onset, with no personal or family history suggestive of psychiatric or other types of disease. In all cases, an initial evaluation was made by a child psychiatrist, including interviews with the patient and family members, while awaiting the results of other laboratory tests and clinical evaluations performed. With the exception of case 1, where specific treatment was given until additional symptoms appeared, the psychiatrist adopted a “wait and see” strategy until other diagnostic options could be ruled out.
In anti-NMDAR encephalitis, diagnostic tests such as imaging studies have little value. In most cases, brain magnetic resonance imaging will be normal, and if abnormalities are identified, they will be transient and non-specific, with no bearing on the duration of the disease or the prognosis.8 EEG is abnormal in most patients, and exhibits slow and highly disorganised activity that becomes more evident as the patient's level of consciousness deteriorates, but does not correlate with the presence of seizures, and is not modified by anticonvulsants.5,8 On the other hand, studies of the cerebrospinal fluid show abnormalities in almost all patients, such as lymphocytic pleocytosis and slightly elevated proteins. These findings are non-specific. These studies were performed in all 3 patients reported here, and the results were similar to those reported in the medical literature. Except for the finding of pleocytosis in cerebrospinal fluid, which prompted us to order complete bacteriological and viral cultures together with serology to rule out infection and to start antibiotic or antiviral therapy, none of the neuroimaging or EEG findings caused us to vary the therapeutic strategy. However, they did help to increase diagnostic suspicion by ruling out other conditions (herpesviral encephalitis, neoplasias or cerebral cortical malformations, among others).
A positive finding of anti-NMDAR antibodies in cerebrospinal fluid is confirmatory, but titres may vary and may even be undetectable if testing is delayed or performed after the start of immunotherapy.5,9 In addition, antibody titres may appear in other clinical, infectious or autoimmune entities (for example, herpes or systemic lupus erythematosus), and such tests are not readily available in many hospitals. In the cases presented here, specific serological tests were ordered in view of the high clinical suspicion of anti-NMDAR encephalitis. However, due to administrative difficulties related to the international dispatch of samples, these tests were only performed in one of the patients. Nevertheless, specific treatment was started on the recommendation of all the specialists involved based on the high clinical suspicion and the exclusion of other more prevalent aetiologies.
The foregoing considerations show the importance of clinical diagnosis in the decision to start the immunotherapy that these patients require, and highlight the importance of diagnostic awareness in the early detection of this condition. Some studies suggest that suspicion of anti-NMDAR encephalitis should take priority over other diagnostic options in all patients presenting severe psychotic symptoms together with other manifestations, such as catatonia.10 Interdisciplinary teamwork and discussions with other specialists will allow clinicians to recognise the cardinal symptoms, differentiate them from other disorders with primary behavioural manifestations, and therefore achieve a timely diagnosis. Understanding the pathophysiology of antibody interaction with synaptic receptors in the brain helps to understand the complex clinical course of this disorder and can help to predict its evolution, guide the diagnostic approach, and thus establish the corresponding therapeutic algorithms.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gómez Castro JF, Salazar O, Conde Z. Índice de sospecha: manifestaciones psiquiátricas de la encefalitis por anticuerpos anti-NMDAR en pacientes pediátricos. Rev Colomb Psiquiat. 2017;46:252–256.