To analyse the relationship between burden of illness and coping strategies and the demographic variables of caregivers, and the demographic and clinical variables of people diagnosed with schizophrenia.
MethodsMulticentre correlational cross-sectional study including 70 people diagnosed with schizophrenia, or a schizoaffective disorder, and 70 primary informal caregivers. They were evaluated using the Zarit Caregiver Burden Interview, Family Coping Strategies Questionnaire, Scale for the Assessment of Positive Symptoms, Scale for the Assessment of Negative Symptoms, and the brief Disability Assessment Scale.
ResultsBurden of illness positively associated with patient impairment in occupational and social functioning, and negatively with education level. Avoidance, coercion and positive communication were positively associated with impairment in occupational and social functioning of patients. Social interest and friendships showed a positive association with the education level of caregivers. Spiritual assistance negatively correlated with impairment in social functioning and patient age, and resignation was negatively associated with length of the disorder and patient education level.
ConclusionsBurden and dysfunctional coping strategies, such as avoidance and coercion, are associated with functional impairment of the patient. These findings suggest the need to provide support to caregivers, adjusted to the functional level of the patient, in order to prevent burden of care.
Analizar la relación de la carga y las estrategias de afrontamiento con las características demográficas de los cuidadores de personas con esquizofrenia, así como las variables demográficas y clínicas de los pacientes.
MétodosEstudio transversal correlacional multicéntrico en el que se evaluó a 70 personas diagnosticadas de esquizofrenia o trastorno esquizoafectivo y 70 cuidadores informales primarios con la escala de sobrecarga del cuidador de Zarit, el cuestionario de estrategias familiares de afrontamiento, la escala para la evaluación de síntomas positivos, la escala para la evaluación de síntomas negativos y la escala breve de evaluación de la discapacidad.
ResultadosEn este estudio, la carga se correlacionó positivamente con el deterioro del funcionamiento ocupacional y social y presentó asociación negativa con la escolaridad de los pacientes. El escape, la coerción y la comunicación positiva presentaron correlaciones positivas con el deterioro del funcionamiento ocupacional y social de los pacientes. Asimismo, el interés social y las amistades mostraron asociación positiva con la escolaridad de los cuidadores. Además, la ayuda espiritual presentó correlaciones negativas con el deterioro del funcionamiento social y la edad de los pacientes, y la resignación se correlacionó negativamente con la duración del trastorno y la escolaridad de los pacientes.
ConclusionesLa carga y la adopción de estrategias de afrontamiento disfuncionales, como el escape y la coerción, se asocian con el deterioro del funcionamiento de los pacientes. Estos hallazgos indican la necesidad de brindar a los cuidadores apoyos ajustados al nivel de funcionamiento del paciente que prevengan la carga del cuidado.
Providing care to a person diagnosed with schizophrenia means dealing with physical, psychological, social and financial demands deriving from living with the affected family member's disorder and this can lead to a prolonged stressful experience. According to the transactional model of stress and coping proposed by Lazarus and Folkman, burden and coping play a mediating role in the stress process.1 Burden refers to the caregiver's perception of how burdensome the care situation can be for him or her and the impact it has on his or her life.2,3 Although there seems to be consensus about the burden dimensions (subjective and objective), some authors note inconsistencies in the definition of the term and in how the construct is operationalised.4,5 Attention is also drawn both to the negative connotations of the concept of burden, which make any positive aspects of the care experience invisible, and the variability in the way burden is measured.4,5 We should therefore point out that this study focuses on the adverse effects of caring on the mental health of the caregiver. Coping is defined as the set of cognitive and behavioural efforts applied by the individual, in this case the caregiver, to respond to demands he/she judges to be excessive in relation to his/her resources.1
Studies on primary caregivers of people diagnosed with schizophrenia indicate that gender5,6 and kinship7,8 are associated with greater perception of burden by caregivers, and mothers are the ones who bear the greatest burden. Results on the influence of other demographic variables of the caregiver and the family member diagnosed with schizophrenia on the perception of the burden of care are less clear.6,7,9 There is evidence of an association between objective stressors (positive symptoms and low level of patient functioning) and caregiver burden.8,10–14 Other studies, however, report different results.5,15
There seems to be a lack of consistency in the coping strategies applied by caregivers.16 One study conducted in India reported that caregivers of people diagnosed with schizophrenia frequently used emotion-focused coping strategies17; another study conducted in Switzerland found that caregivers more often used problem-focused coping strategies and social support.18 In Chile, it was observed that caregivers of the Aymara indigenous community used the same coping strategies as non-Aymara caregivers, except in regard to spiritual support, which was more frequently used by caregivers in the indigenous community.19
The fact that studies generally use different measurements for the coping strategies used by caregivers makes it difficult to compare results. Few studies have investigated the association between the clinical variables of the patients, the demographic characteristics of patients and caregivers, and the coping strategies used by them. Creado et al.20 found that the use of problem-focused coping strategies was significantly correlated with patients with high levels of functioning. Some studies describe an association between the use of emotion-focused coping strategies (coercion and resignation) and patients with lower levels of functioning and negative symptoms. Other studies state that use of positive communication and over-involvement of the caregiver are associated with the duration of the disorder.21 In terms of demographic characteristics, the evidence indicates that young caregivers, caregivers of younger patients and female informal caregivers more often use problem-focused coping strategies, while married caregivers more often seek spiritual support.21
In view of the contradictory results obtained from studies on burden and coping among informal caregivers of people diagnosed with schizophrenia, this study aimed to analyse the relationship between burden and coping strategies and the demographic characteristics of caregivers, and the demographic and clinical variables of people diagnosed with schizophrenia.
Based on the results of previous research, we expected to find that:
- -
H1: Burden would be significantly associated with kinship (greater burden for mothers), the presence of positive symptoms in the patient and deterioration in the patient's functioning.
- -
H2: Problem-focused coping strategies would correlate negatively with the age of the caregiver and the patient and positively with the level of functioning of the patient; whereas emotion-focused coping strategies would correlate positively with the presence of negative symptoms and negatively with the level of functioning of the patient.
This article presents the results of the descriptive and correlational analysis of the study “Burden, coping, familismo [importance of family] and depression in primary informal caregivers of people diagnosed with schizophrenia in Bogotá, Colombia”, corresponding to caregiver burden and the coping strategies caregivers adopt.
MethodParticipantsConvenience sampling was ‘used to select participants. Participants had links to care services provided by one patient and family association, two private clinics and one public hospital. In total, 99 people diagnosed with schizophrenia spectrum disorders (schizophrenia or schizoaffective disorder) and their primary informal caregivers were invited to take part in the study. The final sample was composed of 70 patients and their primary caregivers (n=70) who voluntarily agreed to take part.
The patient inclusion criteria were: (a) be aged from 18 to 60; (b) have been diagnosed with schizophrenia spectrum disorder (schizophrenia or schizoaffective disorder); (c) have had the disorder for at least 1 year; (d) reside at the same address as the caregiver; (e) receive outpatient psychiatric care; and (f) sign informed consent form.
The inclusion criteria for the caregivers were: (a) be aged over 18; (b) be a relative of the patient; (c) live with and have daily contact with the patient; (d) self-identify as the primary caregiver; and (e) sign the informed consent form. Caregivers who reported a diagnosis of depression, bipolar affective disorder or other serious mental illness were excluded from participation.
InstrumentsDemographic variables of the carers and patientsThe demographic data (gender, age, marital status, educational level, current occupation, relationship with the patient and number of contact hours) were collected through a questionnaire designed ad hoc for the study.
Patient clinical and functioning variablesAn item referring to the duration of the disorder and another related to the diagnosis were included in the demographic data questionnaire. An option was also added about the presence or absence of other comorbid disorders in the patients with schizophrenia or schizoaffective disorder.
Positive and negative symptomsThe severity of the patients’ symptoms was measured using the scale for the assessment of negative symptoms (SANS) and the scale for the assessment of positive symptoms (SAPS), validated in Colombia by García-Valencia et al.22 The two scales are complementary instruments to assess the severity of positive and negative symptoms of patients with schizophrenia. The SANS measures negative symptoms in 5 categories: affective blunting, alogia, avolition/apathy, anhedonia/asociality and attentional impairment. The SAPS measures positive symptoms in 5 categories: hallucinations, delusions, bizarre behaviour, positive formal thought disorder and inappropriate affect. The SAPS has a range of scores from 0 to 155, while in the SANS the range is 0–95. The higher the score, the more severe the disorder. In the study by García-Valencia et al.,22 Cronbach's alpha for the SAPS was 0.81 and α=0.94 for the SANS. Both scales showed good reproducibility between assessors and test-retest. In this study, α=0.83 and α=0.79 were obtained respectively.
Level of functioning of the patientThe level of functioning of the patient was measured using the Spanish adaptation of the brief disability assessment scale (WHO DAS-S).23 The DAS-S is an instrument recommended by the WHO for the assessment of difficulties secondary to physical problems or mental health disorders in the following areas: personal care, occupation, family and social functioning. The WHO DAS-S scores the patient's psychosocial functioning in different areas from 0 to 5. This scale showed a coefficient of α=0.67.
CopingCoping strategies were assessed using the family coping strategies questionnaire (FCQ),24 a self-assessment questionnaire consisting of 34 items, divided into the following subscales: (a) information: search for information about the patient's disorder; (b) positive communication; (c) social interest: maintaining of leisure activities and social interest by the caregiver; (d) coercion; e) escape: patient avoidance; (f) resignation about the patient's health condition; (g) over-involvement: attempts by the caregiver to involve the patient in family and social activities; (h) alcohol/drugs: use of alcohol and drugs by the caregiver; (i) collusion: permissive reactions to bizarre behaviour and failure to adhere to the prescribed treatment; (j) spiritual support: seeking spiritual support; and (k) friendships: talking to friends about the patient's condition. The use of coping strategies is scored from 1 to 4. In this study, we used the questionnaire translated into Spanish by Higuera and Aragón25 provided by the Grupo Andaluz de Investigación en Salud Mental [Andalusian Mental Health Research Group] which was adapted to the Colombian context. For this study, the FCQ obtained α=0.77.
BurdenCaregiver burden was measured using the Zarit Caregiver Burden Interview (ZCBI),26 which assesses the subjective burden experienced by the primary caregiver of a person with a mental illness. The negative effects of the caring experience are explored in different areas: physical health, mental health, social activities and financial resources. We used the Spanish adaptation by Martín et al.,26 who reported α=0.91. The ZCBI gives total scores from 0 to 88. This scale showed a high degree of internal consistency for this study (α=0.92).
ProcedureThe objectives and methodology of the study were submitted in writing to the Board of Directors of the Asociación Colombiana de Personas con Esquizofrenia y sus Familias (ACPEF) [Colombian Association of People with Schizophrenia and their Families]. Once the research protocol was approved, the project was presented at the monthly ACPEF meeting in August 2014. This was the first announcement for potential participants. A second announcement was made at the monthly meeting in January 2015. At the same time, the Ethics Committees of Clínica de Nuestra Señora de la Paz, Clínica La Inmaculada and Hospital San Blas in Bogotá approved the research protocol and the tests to be used. Interviews with ACPEF participants were conducted in their homes, while interviews of the participants linked to the clinics and the hospital were conducted in three modalities: (a) immediately after their psychiatry follow-up appointments; (b) through appointments arranged by telephone and held at the institutions; or (c) in the participants’ homes, when they agreed to or requested having the meeting at home. The study's principal investigator conducted the interviews. Occasionally, a previously trained final-year psychology student conducted the interviews with the caregivers. The average duration of each interview was 2h.
Statistical analysisThis study used a cross-sectional design to evaluate the proposed hypotheses. The data was processed using the IBM SPSS version 20 statistical program for Windows. Normality and homogeneity of variance were checked and the burden variable was normalised. Descriptive statistics were used to account for the demographic characteristics of the sample and the results of each scale. We analysed the differences in the level of burden and the use of coping strategies according to the demographic variables of the caregiver and the patient, as well as psychiatric comorbidities, using the Student's t-test or the Mann–Whitney U test (for comparisons between two groups) and one-way ANOVA or the Kruskal–Wallis test (for comparisons between two or more groups), depending on the distribution of the variables. The relationships between burden and coping strategies with age, schooling, daily contact hours and clinical variables were investigated using the Pearson correlation coefficient when the dependent variable met the parametric assumptions or the Spearman correlation coefficient otherwise. In addition, a multiple regression analysis was performed with the burden variable as dependent, introducing the independent variables that showed a significant association with this variable. A value of p<0.05 was selected as the significance threshold.
ResultsDemographic characteristicsWith regard to the patients, we found that they were predominantly male (68.6%) with an average age of 35.6±10.63 years, single (91.4%), with completed Bachillerato (A-level equivalent) (45.7%) and unemployed (74.3%). In terms of clinical variables, the majority of patients had a diagnosis of schizophrenia (91.4%), with no psychiatric comorbidities (83%), and time since onset of five or more years (73%). The patients reported hallucinations (9.8%) and anhedonia (25.5%) as their most common symptoms. Assessment of the level of functioning revealed poor occupational functioning (1.26±1.03) and poor functioning in a broad social context (1.76±1.09).
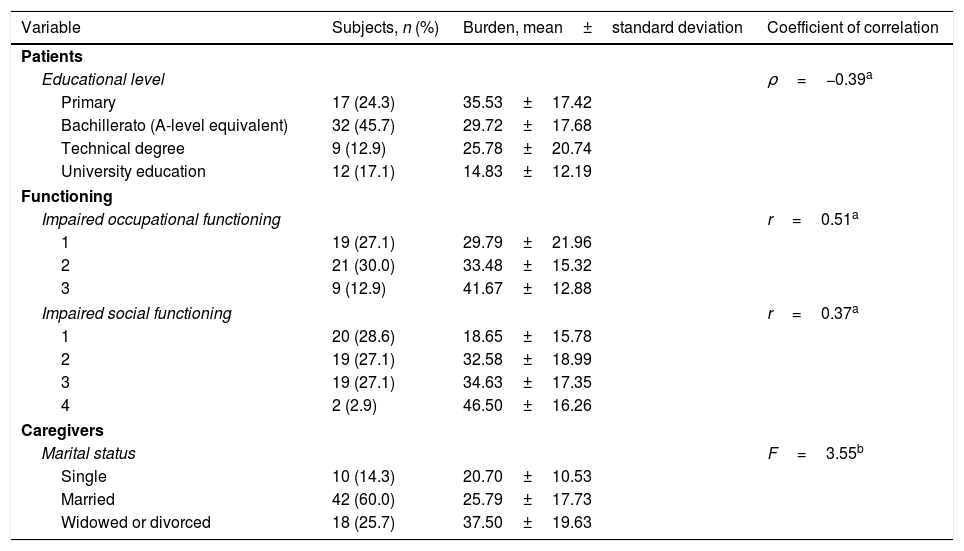
With regard to the caregivers, we found that they were predominantly female, mostly mothers (74%), with an average age of 60.1±9.20 years, married (60%), with completed university education (34.3%), and employed (50%), and they reported 7h or more of daily contact with the patient (58.6%). In this study, the caregivers had an average burden score of 28.07±18.18. Table 1 shows the significant correlations found between the demographic characteristics of the caregivers, the demographic characteristics and clinical variables of the patients, and burden.
Significant correlations between the demographic characteristics of the caregivers, the demographic characteristics and clinical variables of the patients and burden.
| Variable | Subjects, n (%) | Burden, mean±standard deviation | Coefficient of correlation |
|---|---|---|---|
| Patients | |||
| Educational level | ρ=−0.39a | ||
| Primary | 17 (24.3) | 35.53±17.42 | |
| Bachillerato (A-level equivalent) | 32 (45.7) | 29.72±17.68 | |
| Technical degree | 9 (12.9) | 25.78±20.74 | |
| University education | 12 (17.1) | 14.83±12.19 | |
| Functioning | |||
| Impaired occupational functioning | r=0.51a | ||
| 1 | 19 (27.1) | 29.79±21.96 | |
| 2 | 21 (30.0) | 33.48±15.32 | |
| 3 | 9 (12.9) | 41.67±12.88 | |
| Impaired social functioning | r=0.37a | ||
| 1 | 20 (28.6) | 18.65±15.78 | |
| 2 | 19 (27.1) | 32.58±18.99 | |
| 3 | 19 (27.1) | 34.63±17.35 | |
| 4 | 2 (2.9) | 46.50±16.26 | |
| Caregivers | |||
| Marital status | F=3.55b | ||
| Single | 10 (14.3) | 20.70±10.53 | |
| Married | 42 (60.0) | 25.79±17.73 | |
| Widowed or divorced | 18 (25.7) | 37.50±19.63 | |
The results for functioning (WHO DAS-S) do not include values corresponding to 0, “Absence of disability at all times”.
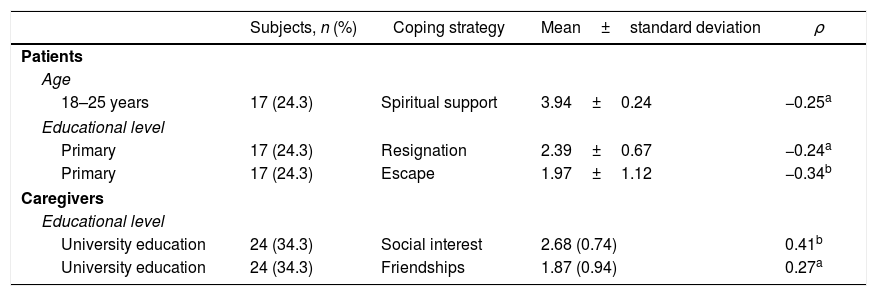
Assessment of the coping strategies showed that spiritual support (3.55±1.03) was the coping strategy most used by caregivers in this study, followed by social interest (2.25±0.80), resignation (2.09±0.82) and positive communication (2.07±0.86).
As regards the correlations between the patients’ clinical variables and the coping strategies used by the caregivers, a negative correlation was found between the duration of the disorder and resignation (ρ=−0.25; p<0.05). Positive correlations were found between impaired occupational functioning and caregivers’ use of escape (ρ=0.34; p<0.01) and positive communication (ρ=0.31; p<0.01), and between impaired social functioning and use of coercion (ρ=0.29; p<0.05). Negative correlation was also found between spiritual support (ρ=−0.27, p<0.05) and impaired social functioning.
In terms of demographic variables, significant differences were found according to the occupation of the caregiver in the use of information as a coping strategy (U=206.5, p 0.05); unemployed caregivers were found to adopt this strategy more frequently (2.34±0.98). Table 2 shows the significant correlations found between other caregiver and patient demographic characteristics and coping strategies. The higher the score (1–4), the more often the coping strategy was used.
Significant correlations between the demographic characteristics of caregivers and patients and coping strategies (FCQ) used by caregivers.
| Subjects, n (%) | Coping strategy | Mean±standard deviation | ρ | |
|---|---|---|---|---|
| Patients | ||||
| Age | ||||
| 18–25 years | 17 (24.3) | Spiritual support | 3.94±0.24 | −0.25a |
| Educational level | ||||
| Primary | 17 (24.3) | Resignation | 2.39±0.67 | −0.24a |
| Primary | 17 (24.3) | Escape | 1.97±1.12 | −0.34b |
| Caregivers | ||||
| Educational level | ||||
| University education | 24 (34.3) | Social interest | 2.68 (0.74) | 0.41b |
| University education | 24 (34.3) | Friendships | 1.87 (0.94) | 0.27a |
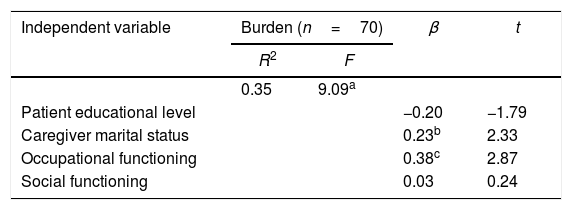
A multiple regression analysis was performed using the variables that correlated significantly with the burden of care. The results of the regression analysis are shown in Table 3. The regression model explained 35% of the variance in burden. The t-scores indicated that the variables of the patient's impaired occupational functioning (t=2.87, p<0.01) and caregiver's marital status (t=2.33; p<0.05) contributed significantly to the prediction model.
DiscussionThe objective of this study was to analyse whether or not caregiver demographic characteristics and the demographic and clinical variables of patients with schizophrenia were related to caregiver burden and coping strategies. The results showed positive correlations of burden with impaired occupational and social functioning of the patient, as well as negative association with their level of schooling. We found significant differences in the measurements of the burden of care according to the marital status of the caregiver. However, the findings showed no correlation of the burden with the type of relationship and the positive symptoms presented by the patient. Consequently, the results partially support H1.
Emotion-focused coping strategies (social interest, escape and coercion) were positively correlated with the level of schooling of the caregiver and impairment of the patient's occupational and social functioning. There was negative correlation (spiritual support, resignation and escape) with the age and level of schooling of the patient, impaired social functioning and the duration of the disorder. Problem-focused coping strategies (positive communication and friendships) correlated positively with impaired occupational functioning of the patient and the level of schooling of the caregiver. Significant differences were found in the use of information as a coping strategy according to the occupation of the caregiver. Contrary to expectations, no significant correlations were found between the use of problem-focused coping strategies and the ages of the caregiver and patient or between emotion-focused coping strategies and the negative symptoms of the patient. Therefore, the results of this study partially support H2.
Most research studies show that caregivers of people with schizophrenia suffer from high levels of burden.7,8,11,12,27 However, at least one study reported a level of burden similar to that found in the sample of Colombian caregivers.28 The variability between studies in the way burden was measured may have contributed to the differences observed in the results. Moreover, some studies indicate that social and cultural aspects may play an important role in the perception of informal caring for a person with schizophrenia as burdensome.5,9,15,29 Weisman et al.30 reported that high levels of family cohesion may have a protective effect against emotional stress in family caregivers of Latin American descent who look after people with schizophrenia. That would raise the question of whether, as Weisman et al. suggest,30 cultural values relating to the family play a modulating role in the stress process for Latin American informal caregivers.
As we mentioned earlier, two demographic variables correlated with the burden of care: the marital status of the caregivers and the educational level of the patients. The role of social support as a coping resource13,31 may partially explain the association between marital status and burden found in this study, as while widowed/divorced caregivers had the highest levels of burden in relation to this variable, the lowest levels were reported by single caregivers. This raises the question of whether the coping strategies put in place by the caregivers might play a mediating role in the above finding. Among caregivers, the association between a high educational level and their adoption of coping strategies, such as maintaining leisure activities and social interest and talking to friends about the patient's condition, may partly explain the difference in burden according to whether they were single or widowed/divorced; 60% of single caregivers had completed university education, as opposed to 11% of widowed/divorced caregivers. We were unable to find other studies that reported on the correlation between patient schooling history and caregiver burden. Such a correlation may be associated with impairment of the patient's functioning. In fact, impaired social and occupational functioning in patients correlated positively with an increase in the caregivers’ level of burden; a finding in line with previous studies.12,13 Unlike other studies, however, we found no significant associations between the burden of care and the duration of the disorder, the presence of comorbidity, or positive or negative symptoms.10,11,13,14,28 That could be because the majority of patients reported mild symptoms and little comorbidity.
As regards coping strategies, in line with previous studies,17,32 caregivers used emotion-focused (spiritual support, social interest and resignation) more than problem-focused strategies. However, the clinical variables of the patients were correlated with the use of both emotion-focused and problem-focused strategies. With impairment in the patients’ occupational and social functioning, caregivers reported using emotion-focused coping strategies (escape and coercion) more often. Nehra et al.17 found a significant association between impaired social functioning in patients and the caregivers using coercion as a coping strategy. Also, in contrast to what was expected, Colombian caregivers reported seeking spiritual support less frequently when the patient had a higher degree of impaired social functioning (ρ=−0.27; p<0.05). A similar association was found between the caregiver seeking spiritual support and the age of the patient (ρ=−0.25; p>0.05). We should mention that the majority of patients under the age of 25 (60%) reported shorter duration of the disorder (1–3 years) than the overall sample; a variable that correlated with more frequent use of resignation as a coping strategy by caregivers. These results suggest that caregivers of younger patients with a shorter duration of the disorder may be in the process of adaptation, and so require specific support to effectively cope with the demands of caring for their affected family member.
With regard to demographic variables, caregivers of patients with a lower level of education frequently used emotion-focused coping strategies (resignation and escape). Meanwhile, caregivers who reported using problem-focused coping strategies were more often those with higher levels of education (talking to friends about the patient's condition) and the unemployed (seeking information about the patient's disorder). In contrast, other studies have found that problem-focused coping strategies were more common among young caregivers, caregivers of younger patients and female caregivers, while seeking spiritual support was the most common option among married caregivers.21
Our study shows that, in the case of Colombian caregivers, the burden is associated with impairment in the patients’ functioning rather than the positive and negative symptoms they may suffer. Our findings also suggest that the level of education of the caregiver may be a protective factor against stress; on the one hand, caregiver education level is negatively associated with the use of coping strategies proven to be dysfunctional, such as resignation and escape, while on the other, it is associated with the use of strategies known to be effective and adaptive, i.e. social interest and friendships. At the same time, we identified a profile of potentially vulnerable caregivers: widowed or divorced caregivers and caregivers with a low level of education. The use of dysfunctional coping strategies (escape and coercion) was associated with impairment of the patient's occupational and social functioning and shorter duration of the disorder. These findings point to the need to provide primary informal caregivers of people diagnosed with schizophrenia support adapted to the phase of the disorder the patient is in and any functional impairment the patient may suffer from.
Limitations and future studiesFirst of all, the sample in this study is not sufficiently broad and representative, as it is made up of families from the capital connected to medical and psychosocial care services. Research studies need to be carried out in other areas of the country, including in rural settings with less access to medical and healthcare resources, which might provide more information about the stress process in caring for people with schizophrenia. Moreover, as this was a cross-sectional study with patients in stable phase, it was not possible to verify possible changes in both the levels of burden and the coping strategies adopted by the caregivers in response to changes in the patients’ symptoms. Longitudinal studies would be required to address that problem. Lastly, future research should investigate the role of cultural values relating to the family, possible consequences of informal care, such as caregivers developing depressive symptoms, and the mediating role of burden and coping strategies in relation to the consequences of family-based care.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Mora-Castañeda B, Márquez-González M, Fernández-Liria A, de la Espriella R, Torres N, Borrero ÁA. Variables demográficas y clínicas relacionadas con la carga y el afrontamiento de los cuidadores de personas diagnosticadas de esquizofrenia. Rev Colomb Psiquiat. 2018;47:13–20.