To evaluate patterns of association between anxiety and depression and the different elements of the construct of quality of life, in patients with locally advanced breast cancer or disseminated stages.
MethodsWith a single measure over time, HADS and FACIT-B scales were applied in 107 women histologically confirmed to have breast cancer, in stages IIB, IIIA, IIIB, IIIC and IV. Factor analysis and multidimensional scaling methods were used to analyse patterns of association.
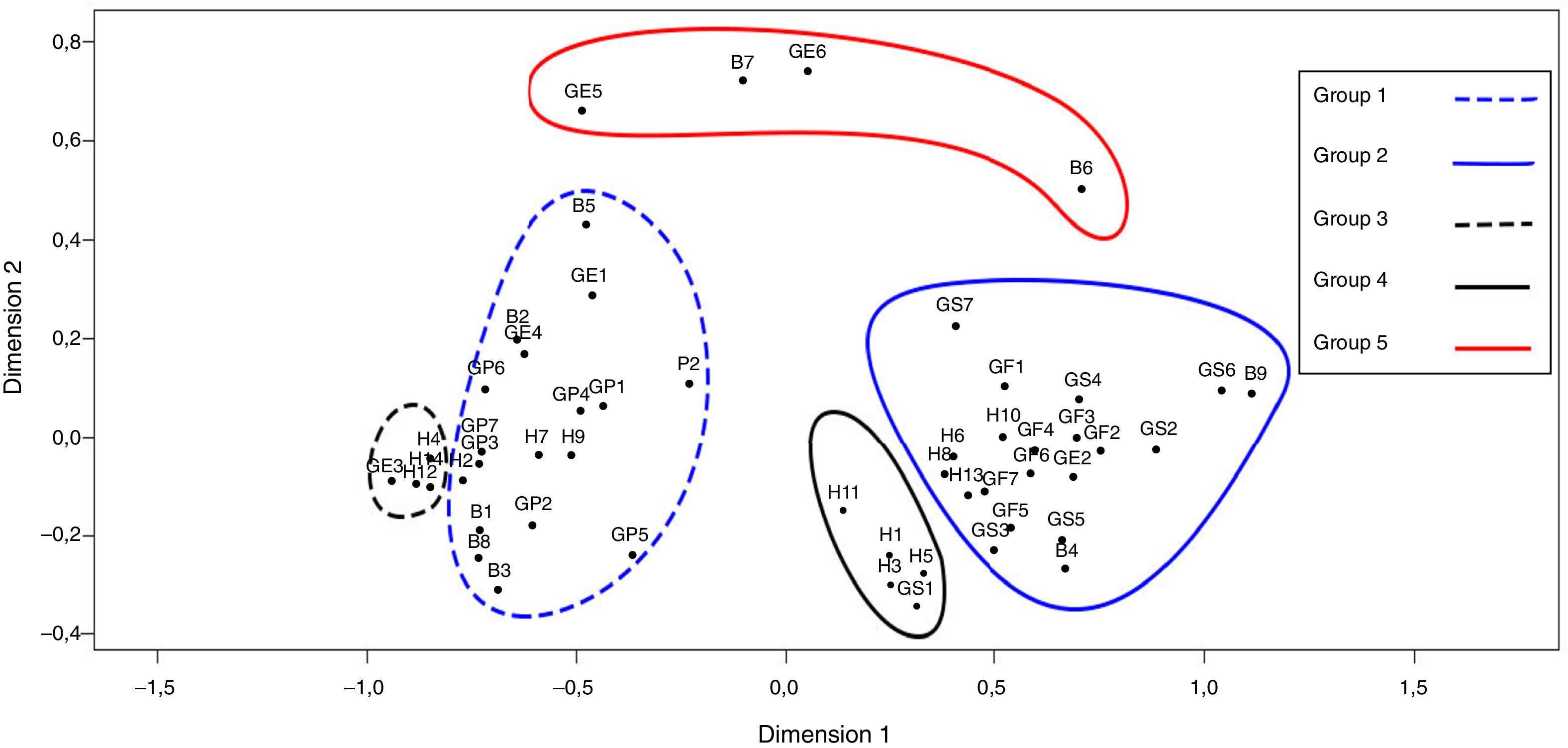
ResultsIn 84.1% of the patients clinical anxiety was found (95%CI, 75.8–90.5%) and clinical depression in 25.2% (95%CI, 17.3–34.6%). Factor analysis groups items of the two scales in 4 domains which accounted for 59% of the total variance, where 2 items (H11 and B8) showed high values of uniqueness and low factor loadings. Multidimensional scaling suggests five groups, showing proximity between depressive symptoms and physical symptoms, as well as between anxious symptoms and related to functionality and social and family environment.
ConclusionsThe HADS in patients with neoplastic disease detects a high frequency of depressive and especially anxious symptoms, which makes it advisable to reevaluate their psychometric properties in patients with cancer. The association between depressive symptoms of HADS and physical symptoms of quality of life construct is in favour of the difficulty of diagnosing depressive disorder in patients with cancer, so it may be necessary to develop instruments that allow locating symptoms or clinical characteristics that facilitate this diagnosis.
Evaluar patrones de asociación entre ansiedad y depresión y los diferentes elementos del constructo de calidad de vida en pacientes con cáncer de mama en estadio localmente avanzado o diseminado.
MétodosSe aplicó una sola medición mediante las escalas FACIT-B y HADS a 107 mujeres con diagnóstico de cáncer de mama en estadios IIB, IIIA, IIIB, IIIC y IV, confirmado histológicamente. Para analizar patrones de asociación, se utilizaron métodos de análisis factorial y escalamiento multidimensional.
ResultadosSe encontró ansiedad clínica en el 84,1% (IC95%, 75,8–90,5%) de las pacientes y depresión clínica en el 25,2% (IC95%, 17,3–34,6%). El análisis factorial agrupa los ítems de los 2 instrumentos en 4 dominios, que dieron cuenta del 59% de la varianza total, donde 2 ítems (H11 y B8) presentaron valores de unicidad altos y cargas factoriales bajas. El escalamiento multidimensional señala 5 agrupaciones, que muestran proximidad entre síntomas depresivos y síntomas físicos, así como entre síntomas ansiosos y lo referente a funcionalidad y ambiente sociofamiliar.
ConclusionesEn pacientes con enfermedad neoplásica, la HADS detecta una alta frecuencia de síntomas depresivos y especialmente ansiosos, lo que hace recomendable revaluar sus propiedades sicométricas para pacientes con cáncer. La asociación entre síntomas depresivos de la HADS y síntomas físicos del constructo de calidad de vida apunta a la dificultad para el diagnóstico de trastorno depresivo en pacientes con cáncer, por lo que puede ser necesario desarrollar instrumentos que permitan ubicar síntomas o características clínicas que faciliten este diagnóstico.
Cancer is usually a traumatic experience for patients due to the various threats associated with the disease, including the diagnosis of a potentially fatal condition, complex treatment regimens, and the side effects resulting therefrom.1,2 Aspects such as these mean that many patients experience cancer diagnosis as a life-threatening situation.3
It has been recognised that the diagnosis of a life-threatening disease is one of the stress factors that might precipitate a post-traumatic stress disorder.4 Cancer diagnosis has frequently been found to be related to psychiatric comorbidities such as depression and anxiety,5 as reported in studies on patients with breast cancer, who showed higher rates of depression than in healthy women, possibly as a response to the threat associated with being diagnosed with the disease.6
The psychiatric disorders most commonly seen in cancer patients and which persist are, firstly, anxiety disorders—specifically phobias—and secondly, mood disorders, specifically major depression.7 Some works have shown a greater mental disorder prevalence among female cancer patients. In the first year following diagnosis in particular, it is highlighted that the prevalence of depression among women with cancer is double that observed in the general female population.8 In breast cancer patients, psychological malaise has been primarily related to mood disorders, anxiety disorders, anger, low self-esteem and low emotional support.9
As well as the psychological disturbances that initially arise following the diagnosis of the disease, in breast cancer patients there are also side effects from the treatments: lymphoedema, sensory disorders, persistent pain associated with reduced arm function and the side effects of chemotherapy, which may impair physical function, psychological well-being and, consequently, quality of life.10 As a result, cancer may be seen as a “long process of adaptation to multiple threats and novel experiences”.11
The World Health Organization defines health-related quality of life (HRQoL) as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the person's physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment”.12 In recent years, there has been an increased output of clinical trials with HRQoL as a primary outcome,13 leading it to be a key factor in clinical decision making.
The emotional regulation strategies used by individuals in the face of distressing life events—such as suffering from a potentially fatal disease—have been found to affect not only their initial emotional response, but also their clinical evolution.14,15 Different trajectories of psychological change following the diagnosis of breast cancer are mentioned, defined according to levels of distress, time of onset and changes over time. One such trajectory is known as “resilience”.16
The concept of resilience is described as a mechanism that protects people against the psychological risks associated with adversity17; it is positively associated with physical, emotional, cognitive and social well-being and HRQoL, and negatively associated with anxiety and depression, as shown in certain studies in which patients who expressed high resilience suffered less fatigue and depression and had a better HRQoL. Resilience or recovery capacity is therefore considered a negative predictor of depression and anxiety,18 in accordance with the findings of studies on patients with nasopharyngeal cancer, where depression or anxiety were negatively correlated, and individuals who presented these mood disorders demonstrated poor functioning across all of the HRQoL domains.19
Some authors propose classifying the impact of breast cancer into three areas that may correlate with possible psychiatric disorders: mood disorders (such as anxiety, depression and anger), lifestyle changes (such as physical malaise, relationship or sexual problems, reduced activity level) and fear or concerns (related to the mastectomy and/or breast loss, body image, recurrence of the disease or death).20
The risk of failing to diagnose psychiatric disorders in breast cancer patients in a timely fashion is the consequent lack of treatment, as depression and its associated symptoms have a major impact since, as well as directly compromising HRQoL,21 they may lower adherence to medical treatments22 and even reduce survival.23 According to some studies, treating depression in women with breast cancer has improved their HRQoL and increased survival24; on the other hand, when anxiety and a reduced HRQoL are not managed, they may become barriers to women returning to their former functioning.25
The relationship between HRQoL and anxiety or depression has also been evaluated in individuals with other conditions besides cancer; in patients diagnosed with epilepsy, some results have confirmed the association between HRQoL and depression.26 The possible impact on individuals acting as carers to patients with different forms of cancer has also been assessed and, where there are higher levels of anxiety and depression among the patients, a significant negative association is also observed in terms of the quality of life of their spousal carers, primarily in the mental component.27 In turn, in patients with haematological cancer, it has been reported that fatigue, anxiety and depression are factors that negatively influence HRQoL,28 and the existing relationship between these variables is confirmed.
Considering the importance of emotional symptoms in cancer patients, and the relationship that has been reported between anxiety and depression and HRQoL, as well as the impact of the latter on other variables, this study seeks to evaluate whether there are other patterns of association between emotional symptoms and the different constituent parts of the HRQoL construct in a sample of breast cancer patients in the locally advanced or disseminated stage, taking into account that the severity of the neoplastic disease may be accompanied by significant emotional responses.
Material and methodsFor this study, we sampled a group of patients over 18 years of age with a diagnosis of histologically confirmed breast cancer in the locally advanced (IIB, IIIA, IIIB, IIIC) or disseminated stage, who attended the National Cancer Institute of Colombia in Bogotá to receive treatment and gave their consent to participate in a study on complementary and alternative treatments, the conduct of which was approved by the institution's ethics committee. The data were collected between 2012 and 2015. Sampling was non-probabilistic, consecutive, sequential, convenience sampling, depending on the fulfilment of the above-mentioned inclusion criteria. The excluded patients were those with sensory or cognitive disorders that impeded them from understanding the content and responding appropriately to the items on the scales used or who did not agree to participate in the study.
The instruments used were: (a) the Hospital Anxiety and Depression Scale (HADS), validated for use in Colombia, which showed adequate psychometric properties. The use thereof is recommended in the oncology context and it comprises 14 items, 7 referring to anxiety and 7 to depression, scored on a Likert-type scale, each from 0 to 3, to obtain scores for each subscale between 0 and 21,29 and (b) the Functional Assessment of Chronic Illness Therapy Quality of Life-Breast (FACIT-B), which is widely used to evaluate HRQoL in women with breast cancer and validated for use in Colombia. This showed adequate reliability and capacity to detect changes in the construct dimensions30 and is composed of 36 items comprising 5 domains: physical well-being (7 items), social/family well-being (7 items), emotional well-being (6 items), functional well-being (7 items) and a specific subscale for breast cancer (9 items). The items are scored on a Likert-type scale with five levels, ranging from 0 (not at all) to 4 (very much).
Information related to clinical variables—such as stage, tumour-node-metastasis (TNM), medical treatments received for breast cancer and assessments by mental health services—was taken from the digital clinical history system used at the National Cancer Institute of Colombia. A trained research assistant applied the instruments and searched for information in the clinical histories.
Statistical analysisFor the descriptive component, pertinent numerical tools were used based on the type of variable: means±standard deviation or medians [interquartile range] for continuous variables or percentages for categorical variables.
The association between categorical variables was evaluated using Fisher's exact test and the difference between means with one-way ANOVA. For hypothesis testing, 5% significance levels and a two-tailed hypothesis were used.
To analyse patterns of association between the two instruments (FACIT-B and HADS), polychoric correlation coefficients were estimated, given that the scale items are rated on an ordinal scale. On this correlation structure, minimum residual factor analysis (MinRes in R) and multidimensional scaling were performed; very simple structure (VSS)31 and parallel analysis criteria were used to select the number of factors.32 For multidimensional scaling, the SMACOF procedure was applied, which uses a non-metric model to carry out “iterative majorization”.33
The sample size was chosen taking into account that, for multidimensional scaling, procedures with small samples, sizes of between 100 and 200 allow less variability than large samples.34 Statistical analyses were performed with the R programme.
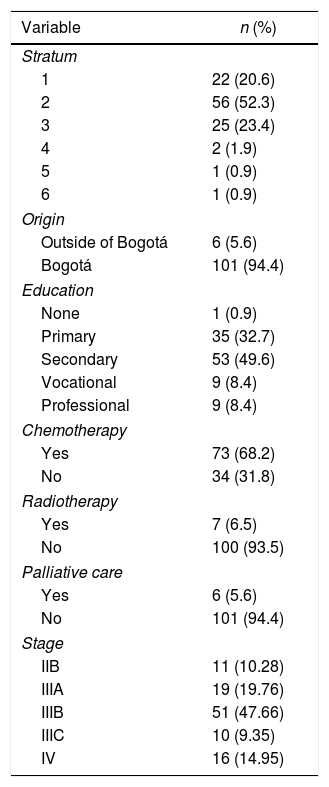
Results107 patients with a mean age of 53.9±8.7 years were evaluated. The majority were from low socioeconomic strata (96.3% of the patients were in a stratum ≤3), 94.4% (n=101) lived in Bogotá at the time of the evaluation and the median number of years spent in education was 7 [7] years (Table 1).
Clinical and demographic characteristics of the patients.
| Variable | n (%) |
|---|---|
| Stratum | |
| 1 | 22 (20.6) |
| 2 | 56 (52.3) |
| 3 | 25 (23.4) |
| 4 | 2 (1.9) |
| 5 | 1 (0.9) |
| 6 | 1 (0.9) |
| Origin | |
| Outside of Bogotá | 6 (5.6) |
| Bogotá | 101 (94.4) |
| Education | |
| None | 1 (0.9) |
| Primary | 35 (32.7) |
| Secondary | 53 (49.6) |
| Vocational | 9 (8.4) |
| Professional | 9 (8.4) |
| Chemotherapy | |
| Yes | 73 (68.2) |
| No | 34 (31.8) |
| Radiotherapy | |
| Yes | 7 (6.5) |
| No | 100 (93.5) |
| Palliative care | |
| Yes | 6 (5.6) |
| No | 101 (94.4) |
| Stage | |
| IIB | 11 (10.28) |
| IIIA | 19 (19.76) |
| IIIB | 51 (47.66) |
| IIIC | 10 (9.35) |
| IV | 16 (14.95) |
In relation to clinical characteristics, at the time of the evaluation, 68% of the patients were receiving chemotherapy, 7 patients were receiving radiotherapy, 6 were having palliative care and 6 had undergone surgery. The time elapsed between the surgical procedure and evaluation was a median of 135 [1,276] days. The predominant clinical stage was III (over 70%) and the median time elapsed between the date of diagnosis to the evaluation was 112 [163] days (Table 1).
According to the HADS cut-off score (>8), 90 of the patients had clinical anxiety (84.1%; 95% confidence interval [95% CI], 75.8%–90.5%) and 27 (25.2%; 95% CI, 17.3%–34.6%) had clinical depression according to the same scale's cut-off (>9). It was observed that, of the entire sample, 14% (n=15) of the patients were assessed by mental health services at the institution, 73% (n=11) of whom were considered to have anxiety disorders and 26.6% (n=4) depression disorders.
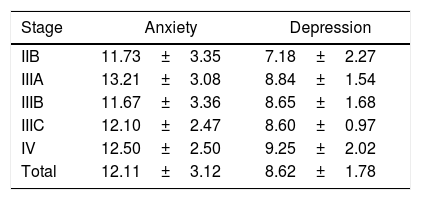
No association was found between age categorised (>50 years) and the presence of anxious or depressive symptoms (Fisher's exact test, p>0.05); the anxiety component scores were 12.3 and 12.0 for patients under and over 50, respectively, and, for depression, 8.8 and 8.5, respectively (both insignificant differences). Similarly, no significant difference was observed between the mean anxiety scores according to clinical stage, but a statistically significant difference was found between the means for depression according to clinical stage (F(4,102)=2.51; p=0.046) (Table 2); said difference is due to the stage IV-stage IIB combination (p=0.029).
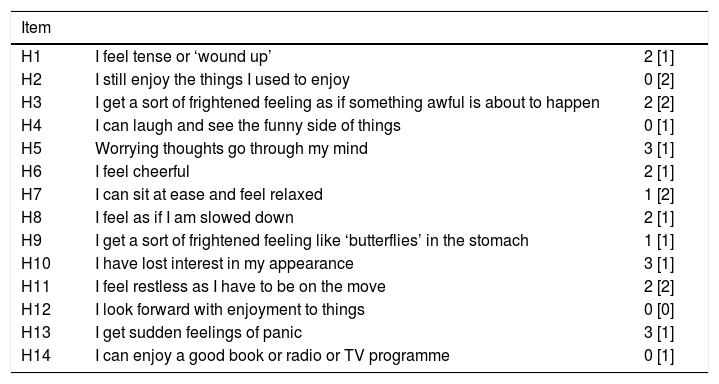
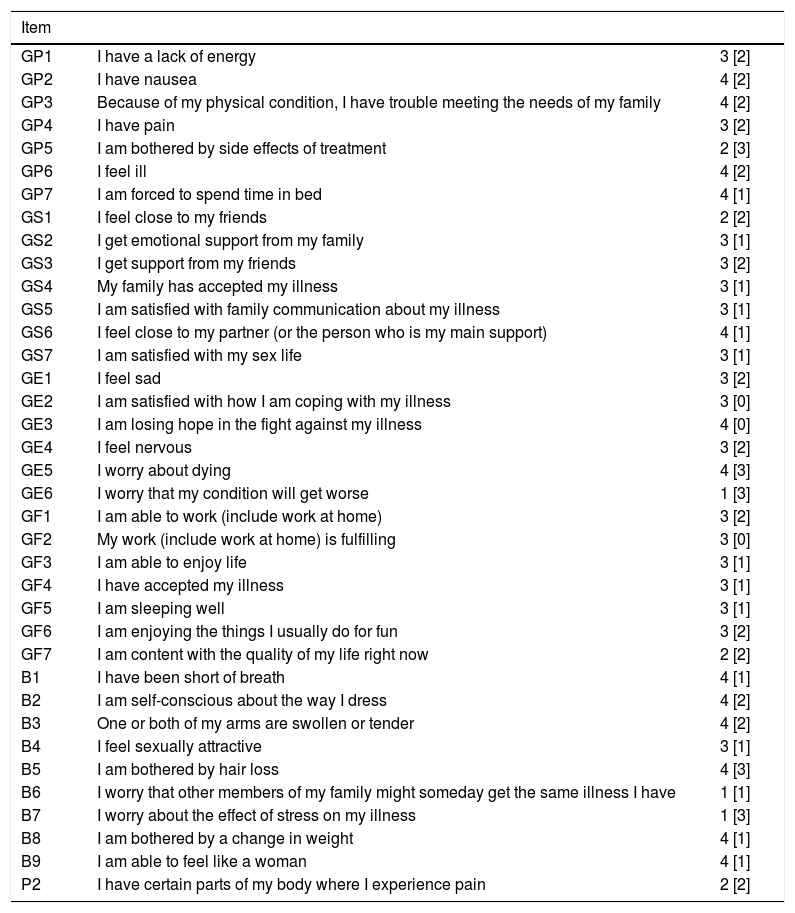
The highest scoring HADS items were “Worrying thoughts go through my mind”, “I have lost interest in my appearance” and “I get sudden feelings of panic”; the lowest scores were given for the items “I still enjoy the things I used to enjoy”, “I can laugh and see the funny side of things”, “I look forward with enjoyment to things” and “I can enjoy a good book or radio or TV programme” (Table 3). Among the medians for the FACIT-B scale items, it can be observed that the lowest scores correspond to the items “I worry that my condition will get worse”, “I worry that other members of my family might someday get the same illness I have” and “I worry about the effect of stress on my illness” (Table 4).
Scores from the HADS items.
| Item | ||
|---|---|---|
| H1 | I feel tense or ‘wound up’ | 2 [1] |
| H2 | I still enjoy the things I used to enjoy | 0 [2] |
| H3 | I get a sort of frightened feeling as if something awful is about to happen | 2 [2] |
| H4 | I can laugh and see the funny side of things | 0 [1] |
| H5 | Worrying thoughts go through my mind | 3 [1] |
| H6 | I feel cheerful | 2 [1] |
| H7 | I can sit at ease and feel relaxed | 1 [2] |
| H8 | I feel as if I am slowed down | 2 [1] |
| H9 | I get a sort of frightened feeling like ‘butterflies’ in the stomach | 1 [1] |
| H10 | I have lost interest in my appearance | 3 [1] |
| H11 | I feel restless as I have to be on the move | 2 [2] |
| H12 | I look forward with enjoyment to things | 0 [0] |
| H13 | I get sudden feelings of panic | 3 [1] |
| H14 | I can enjoy a good book or radio or TV programme | 0 [1] |
Values are expressed as the median [interquartile range].
Scores from the FACIT-B scale items.
| Item | ||
|---|---|---|
| GP1 | I have a lack of energy | 3 [2] |
| GP2 | I have nausea | 4 [2] |
| GP3 | Because of my physical condition, I have trouble meeting the needs of my family | 4 [2] |
| GP4 | I have pain | 3 [2] |
| GP5 | I am bothered by side effects of treatment | 2 [3] |
| GP6 | I feel ill | 4 [2] |
| GP7 | I am forced to spend time in bed | 4 [1] |
| GS1 | I feel close to my friends | 2 [2] |
| GS2 | I get emotional support from my family | 3 [1] |
| GS3 | I get support from my friends | 3 [2] |
| GS4 | My family has accepted my illness | 3 [1] |
| GS5 | I am satisfied with family communication about my illness | 3 [1] |
| GS6 | I feel close to my partner (or the person who is my main support) | 4 [1] |
| GS7 | I am satisfied with my sex life | 3 [1] |
| GE1 | I feel sad | 3 [2] |
| GE2 | I am satisfied with how I am coping with my illness | 3 [0] |
| GE3 | I am losing hope in the fight against my illness | 4 [0] |
| GE4 | I feel nervous | 3 [2] |
| GE5 | I worry about dying | 4 [3] |
| GE6 | I worry that my condition will get worse | 1 [3] |
| GF1 | I am able to work (include work at home) | 3 [2] |
| GF2 | My work (include work at home) is fulfilling | 3 [0] |
| GF3 | I am able to enjoy life | 3 [1] |
| GF4 | I have accepted my illness | 3 [1] |
| GF5 | I am sleeping well | 3 [1] |
| GF6 | I am enjoying the things I usually do for fun | 3 [2] |
| GF7 | I am content with the quality of my life right now | 2 [2] |
| B1 | I have been short of breath | 4 [1] |
| B2 | I am self-conscious about the way I dress | 4 [2] |
| B3 | One or both of my arms are swollen or tender | 4 [2] |
| B4 | I feel sexually attractive | 3 [1] |
| B5 | I am bothered by hair loss | 4 [3] |
| B6 | I worry that other members of my family might someday get the same illness I have | 1 [1] |
| B7 | I worry about the effect of stress on my illness | 1 [3] |
| B8 | I am bothered by a change in weight | 4 [1] |
| B9 | I am able to feel like a woman | 4 [1] |
| P2 | I have certain parts of my body where I experience pain | 2 [2] |
Values are expressed as the median [interquartile range].
Among the scores for the different domains corresponding to both of the scales applied, the lowest medians within the quality of life domains correspond to functional well-being (18 [6]) and social/family well-being (19 [7]); on the HADS, the lowest median was for depression (9 [2]). For the other domains, the results were as follows: physical well-being (21 [8]), emotional well-being (20 [8]), breast cancer-related well-being (28 [8]) and HADS anxiety (13 [4]).
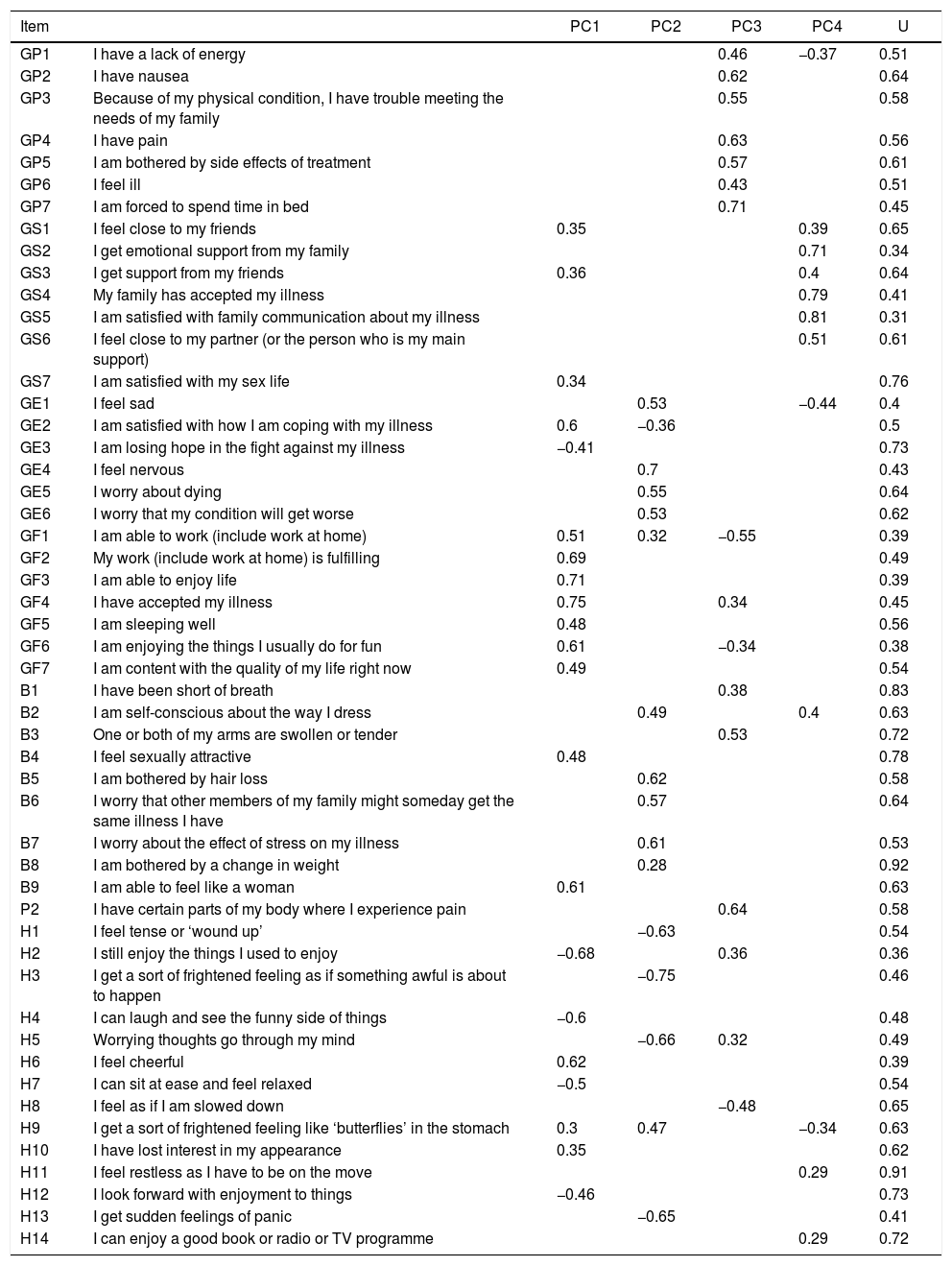
Factor analysisUsing VSS and parallel analysis criteria, an optimum number of four domains was determined, accounting for 59% of the total variance. The structure that proved most suitable for interpretation corresponded to a promax-type oblique rotation (Table 5).
Factor analysis of the HADS and FACIT-B scale.
| Item | PC1 | PC2 | PC3 | PC4 | U | |
|---|---|---|---|---|---|---|
| GP1 | I have a lack of energy | 0.46 | −0.37 | 0.51 | ||
| GP2 | I have nausea | 0.62 | 0.64 | |||
| GP3 | Because of my physical condition, I have trouble meeting the needs of my family | 0.55 | 0.58 | |||
| GP4 | I have pain | 0.63 | 0.56 | |||
| GP5 | I am bothered by side effects of treatment | 0.57 | 0.61 | |||
| GP6 | I feel ill | 0.43 | 0.51 | |||
| GP7 | I am forced to spend time in bed | 0.71 | 0.45 | |||
| GS1 | I feel close to my friends | 0.35 | 0.39 | 0.65 | ||
| GS2 | I get emotional support from my family | 0.71 | 0.34 | |||
| GS3 | I get support from my friends | 0.36 | 0.4 | 0.64 | ||
| GS4 | My family has accepted my illness | 0.79 | 0.41 | |||
| GS5 | I am satisfied with family communication about my illness | 0.81 | 0.31 | |||
| GS6 | I feel close to my partner (or the person who is my main support) | 0.51 | 0.61 | |||
| GS7 | I am satisfied with my sex life | 0.34 | 0.76 | |||
| GE1 | I feel sad | 0.53 | −0.44 | 0.4 | ||
| GE2 | I am satisfied with how I am coping with my illness | 0.6 | −0.36 | 0.5 | ||
| GE3 | I am losing hope in the fight against my illness | −0.41 | 0.73 | |||
| GE4 | I feel nervous | 0.7 | 0.43 | |||
| GE5 | I worry about dying | 0.55 | 0.64 | |||
| GE6 | I worry that my condition will get worse | 0.53 | 0.62 | |||
| GF1 | I am able to work (include work at home) | 0.51 | 0.32 | −0.55 | 0.39 | |
| GF2 | My work (include work at home) is fulfilling | 0.69 | 0.49 | |||
| GF3 | I am able to enjoy life | 0.71 | 0.39 | |||
| GF4 | I have accepted my illness | 0.75 | 0.34 | 0.45 | ||
| GF5 | I am sleeping well | 0.48 | 0.56 | |||
| GF6 | I am enjoying the things I usually do for fun | 0.61 | −0.34 | 0.38 | ||
| GF7 | I am content with the quality of my life right now | 0.49 | 0.54 | |||
| B1 | I have been short of breath | 0.38 | 0.83 | |||
| B2 | I am self-conscious about the way I dress | 0.49 | 0.4 | 0.63 | ||
| B3 | One or both of my arms are swollen or tender | 0.53 | 0.72 | |||
| B4 | I feel sexually attractive | 0.48 | 0.78 | |||
| B5 | I am bothered by hair loss | 0.62 | 0.58 | |||
| B6 | I worry that other members of my family might someday get the same illness I have | 0.57 | 0.64 | |||
| B7 | I worry about the effect of stress on my illness | 0.61 | 0.53 | |||
| B8 | I am bothered by a change in weight | 0.28 | 0.92 | |||
| B9 | I am able to feel like a woman | 0.61 | 0.63 | |||
| P2 | I have certain parts of my body where I experience pain | 0.64 | 0.58 | |||
| H1 | I feel tense or ‘wound up’ | −0.63 | 0.54 | |||
| H2 | I still enjoy the things I used to enjoy | −0.68 | 0.36 | 0.36 | ||
| H3 | I get a sort of frightened feeling as if something awful is about to happen | −0.75 | 0.46 | |||
| H4 | I can laugh and see the funny side of things | −0.6 | 0.48 | |||
| H5 | Worrying thoughts go through my mind | −0.66 | 0.32 | 0.49 | ||
| H6 | I feel cheerful | 0.62 | 0.39 | |||
| H7 | I can sit at ease and feel relaxed | −0.5 | 0.54 | |||
| H8 | I feel as if I am slowed down | −0.48 | 0.65 | |||
| H9 | I get a sort of frightened feeling like ‘butterflies’ in the stomach | 0.3 | 0.47 | −0.34 | 0.63 | |
| H10 | I have lost interest in my appearance | 0.35 | 0.62 | |||
| H11 | I feel restless as I have to be on the move | 0.29 | 0.91 | |||
| H12 | I look forward with enjoyment to things | −0.46 | 0.73 | |||
| H13 | I get sudden feelings of panic | −0.65 | 0.41 | |||
| H14 | I can enjoy a good book or radio or TV programme | 0.29 | 0.72 |
The four domains found can be summarised as follows:
- •
Domain 1: items related to functionality and personal satisfaction.
- •
Domain 2: items related to concern about the disease.
- •
Domain 3: items related to symptoms and physical condition.
- •
Domain 4: items related to family and friendships.
Two of the items (H11: “I feel restless as I have to be on the move” and B8: “I am bothered by a change in weight”) presented high uniqueness values and factor loadings <0.3 in all of the domains.
Multidimensional scalingThe two-dimensional analysis structure had non-metric stress values of 0.071, while the three-dimensional structure was 0.052. For the two-dimensional structure, the items that showed the highest stress values were B8 (“I am bothered by a change in weight”), with 5.48%, and GS7 (“I am satisfied with my sex life”), with 4.63%. As regards the three-dimensional solution, the highest stress percentage also corresponded to item GS7, with 4.48%. Given the difference between the stress values of the two solutions, analysis on the two-dimensional structure was considered appropriate.
Analysis of the two-dimensional structure primarily shows five groups (Fig. 1):
- •
Group 1: items related to general and breast cancer-specific physical symptoms, some emotional symptoms from the FACIT-B scale and two HADS anxiety items. Core symptoms refer to fatigability and pain (GP1: “I have a lack of energy”; GP4: “I have pain”).
- •
Group 2: items from the functional capacity and social/family environment domains of the FACIT-B scale. Core symptoms are related to satisfaction and coping (GE2: “I am satisfied with how I am coping with my illness”; GF2: “My work is fulfilling”; GF3: “I am able to enjoy life”).
- •
Group 3: items related to depression from the HADS.
- •
Group 4: HADS anxiety items.
- •
Group 5: items related to concerns about the disease (GE5: “I worry about dying”; B7: “I worry about the effect of stress on my illness”; GE6: “I worry that my condition will get worse”; B6: “I worry that other members of my family might someday get the same illness I have”).
On both the two-dimensional and three-dimensional scaling solutions, a proximity was observed between the depressive symptom group and physical breast cancer symptom group. There was also a proximity between the anxious symptom group and functional capacity and social/family environment group. The category gathering concerns about the disease was not specifically related to any of the other four groups, but shows a very clear loading on dimension 2 (Fig. 1).
DiscussionIn this study, we found a greater prevalence of clinical anxiety (84%) and a lower prevalence of depression (25%) than those obtained by other authors in studies with patients at a similar clinical stage of the disease35–38; this difference may be due to a number of reasons: (a) the difference in time since diagnosis and the measurement of these variables, since, as some studies have reported, many patients tend to recover from the shock of diagnosis after the first six months39 and depressive symptoms decrease once they have completed treatment40; (b) the difference in scales used to screen said psychiatric disorders,41 and (c) a potential weakness of the psychometric properties of the instrument used.
Although some authors have proposed that, in similar populations, the youngest patients have the greatest risk of anxiety and depression,35,42 in this study no association was found between age and the presence of clinically significant anxious or depressive symptoms. Other authors have also reported this finding and do not identify age as a risk factor for suffering from these disorders.36
In terms of stage, no significant difference was observed in the clinical anxiety scores, thereby coinciding with other research.36,42 As for depression, one statistically significant difference was found, since it was more common in patients at more advanced stages; this difference had also been reported, especially at the expense of the physical symptom domain.43
The finding regarding the low number of patients (15 [14%]) assessed by the institution's mental health services, in comparison to the quantity that had suspected clinical anxiety or depression taking into account the HADS scores obtained (84% and 25%, respectively), could be due to false positives yielded by the scale, the validation of which was performed on a small sample of cancer patients in Colombia.29 It could also be explained by possible mental health assessments performed outside of the institution, which are not documented in this study, or by the low sensitivity of the treating clinicians regarding the patients’ emotional side, which might prove to be a barrier to the diagnosis of psychiatric disorders.44 This latter aspect has been linked to specific patient attitudes as it has been observed that, when making treatment-related decisions, such as assessment by the mental health services, most patients (61%) prefer to be at the passive end and only a minority (11.0%) prefer to be at the active end.37
In the descriptive analysis, the items that revealed the highest and lowest scores on the FACIT-B scale coincide with those detected in previous studies.30 Likewise, in related studies performed with mean times since diagnosis as diverse as 7 months and 4.6 years, significantly lower scores have been reported in the physical, emotional and general quality of life domains in patients with depression compared to those who are not depressed, indicating that depressive disorder is the variable associated with the greatest decline in HRQoL.38,43 Similarly, other authors have found an association between anxiety and depression and impaired emotional and cognitive aspects of HRQoL,45 and low levels of anxiety and improved depressive symptoms are reported as predictors of improved physical quality of life.37
Patterns of association between anxious and depressive symptoms and elements of the HRQoL construct were studied using complement analysis methods. On the one hand, factor analysis, based on correlation structures, provides information about how the various items measuring different constructs are grouped into a series of observed variables. On the other hand, multidimensional scaling, which is based on calculating the distances between subjects and items, enables the observation of association patterns for groups that summarise the total variability of the construct.46,47
In the factor analysis, the domains found partly reflect the original structure of the FACIT-B scale, particularly those related to physical condition, social/family environment and functionality. However, the items related to the emotional and breast-specific domains, both from the FACIT-B scale, are grouped together into a single structure which we call “concern about the disease”. This may correspond to the presentation of the items in these domains, the majority of which emphasise discomfort or concerns more than the mere presence or absence of symptoms. This is consistent with an instrument that, like the FACIT-B scale, measures HRQoL, hence it seeks to detect the repercussions of the symptoms rather than solely whether they are present.
The HADS anxiety and depression symptoms presented a clinically plausible association: anxious symptoms were related to the concern about the disease domain, while depressive symptoms were related to functionality and personal satisfaction. Concerns are associated with the cognitive component of anxiety disorders, while functionality and related satisfaction are linked to autonomy and self-esteem.
Two items (H11: “I feel restless as I have to be on the move”, and B8: “I am bothered by a change in weight”) have weak loadings on the different factors (<0.3) and high uniqueness values (>0.9); B8 does not seem to have adequate psychometric capacities, as in a previous study it also had the lowest factor loadings in the domain structure.30 As regards item H11, which also appears not to properly fit the detected factor structure, consideration should be given to the possibility that certain particularities relating to the study population (locally advanced or disseminated stage of the disease) may be behind this finding. It would therefore be useful to apply methods to evaluate differential item functioning using the Rasch model, and even more so if we take into account that, in a previous validation in Colombia, said item did not show a poor fit on the factor model.28
One of the HADS items (H8: “I feel as if I am slowed down”), corresponding to depression symptoms, showed an association with domain 3, referring to symptoms and physical condition. In a previous validation of this instrument, item H8 demonstrated inadequate loading on the factor structures analysed29; this may correspond to the fact that the feeling of sluggishness among cancer patients could be perceived as a physical symptom secondary to the disease or its treatment, hence it would not properly evaluate depressive symptoms in this group of patients. A similar drawback has been found in other studies, in which this same item tarnishes the measurement of the HADS depression domain.48
In multidimensional scaling, the relationship found between anxious symptoms and functional capacity and the social/family environment corroborates what has been reported in previous studies, where anxiety contributed significantly to social activity.45 As for the association observed between depressive and physical symptoms, it is noteworthy that, within the conglomeration of physical symptoms, the items occupying the central position are those referring to fatigability and pain—somatic symptoms that have been associated with depression in previous studies39,49; this association between depressive and physical symptoms may reflect the overlap between depression symptoms and cancer symptoms, hindering their differential diagnosis to a great extent.50,51
The fifth group, referring to concerns associated with the disease, where all of the items form part of the FACIT-B scale, shows the importance of measuring concerns as a separate construct that is not clinically associated with symptoms of anxiety and depression, but which plays a significant role when assessing HRQoL in cancer patients. It is worth noting that the HADS evaluates symptoms that are strongly related to psychiatric disorders, while the FACIT-B scale assesses a far broader construct than that of the HRQoL, for which concerns play a significant role in the patient's perceptions thereof.
In multidimensional scaling, the detection of high stress values in FACIT-B scale item B8 (“I am bothered by a change in weight”) coincides with the factor analysis results, thus supporting the previous proposition regarding the psychometric properties of this item.
This study was conducted with just one measurement over time since diagnosis, which could pose a limitation. However, similar studies have observed that there were no significant changes in the measures of depression or anxiety taken at different time points.35,42 Similarly, failing to establish the time between the date of diagnosis and the initiation of treatment could prove to be a limitation in this study, although it has been reported that diagnoses of depression and anxiety are not related to the time since the cancer diagnosis.36
One limitation to bear in mind in this study is that we do not know the history or effective prevalence of anxiety and depression in this group of patients. It is also unknown whether they were receiving psychotropic medication for these disorders, or whether they presented concomitant diagnoses of other non-neoplastic diseases that could be related to anxious or depressive symptoms.
Another limitation relates to the factor analysis, where the sample size used may be insufficient. Moreover, although the HADS has shown adequate psychometric characteristics,41 the validation performed in Colombia has some weaknesses, such as the lack of information provided on the clinical and sociodemographic characteristics of the sample used, as well as the small sample size. An additional limitation is related to the fact that we only evaluated breast cancer patients and excluded those in the early stages. It therefore cannot be ruled out that a broader disease spectrum—not only in terms of stage, but other location types too—could yield different results.
ConclusionsThe high frequency of depressive and anxious symptoms—particularly that detected by the HADS in patients with breast neoplasms—would suggest that it is advisable to re-evaluate the psychometric properties of this instrument in patients with these characteristics. Anxious symptoms were associated with a cognitive component related to concerns and are closer to the social/family and functional domains than to symptoms of the disease. The association found between HADS depressive symptoms and physical symptoms from the quality of life construct demonstrates the difficulty for a differential diagnosis between depression and cancer symptoms. As such, it may be necessary to develop instruments that allow us to pinpoint symptoms or clinical characteristics that facilitate the proper diagnosis of this mood disorder in cancer patients, given the importance of timely treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Valderrama Rios MC, Sánchez Pedraza R. Trastornos de ansiedad y depresión en relación con la calidad de vida de pacientes con cáncer de mama en estadio localmente avanzado o diseminado. Rev Colomb Psiquiat. 2018;47:211–220.