The aim of this study is to analyze the increasing need of radiological support in the diagnosis of acute appendicitis (AA), the clinical repercussions associated, and the parameters of diagnostic accuracy of ultrasound and computed tomography (CT) scan for AA.
Materials and methodsObservational and analytical study. Cohort, patients operated on for suspected AA at a tertiary referral hospital. Pregnancy and <14 years were exclusion criteria. Study group: January 2010–December 2011 (n1=419). Control group: set of patients aged 18–65 years old operated between October 2001 and September 2003 (n2=237). Variables analyzed in both groups: (1) percentage of radiological support for diagnosis of acute appendicitis; (2) sensitivity and positive predictive value (PPV) of ultrasound and CT scan; (3) rate of surgical explorations with negative result or with diagnosis other than acute appendicitis. Statistical analysis: SPSS software, χ2 test, statistical significance accepted with P<05, 95% confidence interval (95% CI) for the odds ratio (OR).
ResultsAge, gender, percentage of atypical locations and gangrenous/perforated episodes were similar in both groups. The number of radiological examinations needed for diagnosis was significantly higher in the study group (78.8% vs 30.4%, P<000). Sensitivity was significantly superior for CT than for ultrasound scan (97% vs 86%), but PPV was similar in both tests (92% vs 94%). Surgical exploration percent values with diagnosis of acute appendicitis were significantly higher in the study group (94.5% vs 88.6%; P<006, OR 2.2; 95% CI: 1.25–4).
ConclusionsCT and ultrasound scan are excellent diagnostic tools for acute appendicitis, and have contributed to a significant increase in surgical explorations with correct diagnosis.
Analizar el incremento del apoyo radiológico solicitado para el diagnóstico de la apendicitis aguda (AA), su justificación a partir de su repercusión clínica así como los parámetros de rentabilidad diagnóstica de ECO y TAC para esta enfermedad.
Material y métodoEstudio observacional analítico de cohortes, con pacientes intervenidos por sospecha de AA en un hospital de tercer nivel, excluyendo menores de 14 años y gestantes. Grupo de estudio: enero de 2010-diciembre de 2011 (n1=419). Grupo control: muestra de pacientes entre 18 y 65 años intervenidos entre octubre de 2001 y septiembre de 2003 (n2=237). Variables de estudio en ambas muestras: 1) porcentaje de exploraciones realizadas como apoyo radiológico al diagnóstico de la apendicitis; 2) sensibilidad y valor predictivo positivo (VPP) de ECO y TAC; 3) tasa de cirugías en blanco y con diagnósticos diferentes de AA. Análisis estadístico: software SPSS, con test de la χ2, aceptando como significativos niveles de p<0,05 y calculando la odds ratio (OR) con su intervalo de confianza al 95% (IC95%).
ResultadosAmbas muestras fueron homogéneas en cuanto a edad, género o porcentaje de localizaciones atípicas y formas evolucionadas. El número de exploraciones solicitadas durante el periodo de estudio fue significativamente mayor que en el control (78,8 vs. 30,4%; p<0,000). La sensibilidad de la TAC fue superior a la de la ECO (97 vs. 86%), aunque ambas pruebas presentaron valores similares de VPP (92 vs. 94%). El porcentaje de intervenciones con diagnóstico certero de AA fue significativamente mayor en el grupo de estudio (94,5 vs. 88,6%; p<0,006; OR: 2,2; IC95% 1,25-4).
ConclusiónEl incremento de solicitudes de apoyo radiológico al diagnóstico de AA conlleva un significativo aumento de intervenciones con diagnóstico certero.
Surgery for acute appendicitis (AA) is the most common abdominal emergency surgery, and there is a 7% risk of developing AA symptoms in one's lifetime.1 Classically, diagnosis of AA has been mainly symptoms-based. Even today many authors continue in the belief that the mere support of certain laboratory determinations is sufficient in most cases, and that radiological support should only be used as an exception to establish diagnosis.
However, many contributions have suggested that abdominal ultrasound and abdominal computed tomography (CT) are highly valid for the diagnosis of AA. Their performance exceeds an exclusively symptoms-based diagnosis, with or without complementary laboratory tests and with or without the application of scoring systems (Alvarado being the most widespread and accepted), and therefore greatly reduces the number of unnecessary and negative surgical explorations.2–5 Moreover, it can also identify patients with an abscess or phlegmon, who are therefore potential candidates for conservative treatment and deferred appendectomy.6
Although the percentage of negative appendectomy explorations in the literature with an exclusively symptoms-based diagnosis is 10%–20%, rates of up to 40% have been reported. Meanwhile, this fact has always been justified by the low morbidity and mortality of appendectomy when compared with the high rate of complications in cases with delayed diagnosis.3,7,8 Nonetheless, in the present context, this liberalization can and should be questioned even if appendectomy is performed laparoscopically, especially when contemplating the diagnostic yield of certain complementary tests such as CT or ultrasound. These considerations have resulted in a clear evolution in the diagnosis of appendix-related emergencies, with a definite increase in requests for radiological support and even its systemic inclusion in diagnostic protocols. We present a study to evaluate the increased demand for radiological support in the diagnosis of AA, its diagnostic yield (and changes therein) and the clinical implications of this development.
Materials and MethodsAnalytical observational cohort study. Population and setting: patients treated surgically for suspected AA at the Carlos Haya Regional University Hospital in Malaga, Spain (patients under the age of 14 or pregnant were treated at another center). Study group: patients operated on due to suspected AA during a 2-year period (January 2010–December 2011). Control group: sample selected for a previous study based on a perioperative variable that was not related with this present study, likewise consisting of patients operated on for suspected diagnosis of AA during a 2-year period (October 2001–September 2003), although the patients were between the ages of 18 and 65. Study variables in both samples included: (1) percentage of radiological examinations (ultrasound and CT), requested and performed as radiological support of AA diagnosis; (2) sensitivity and positive predictive value (PPV) (only yield parameters analyzable with the study design) of ultrasound and CT scan; (3) rate of negative explorations and those with diagnoses other than AA. Statistical analysis: prospective data collection in both groups and subsequent analysis with SPSS software.
We carried out descriptive and homogeneity analyses of both groups with common estimators according to the nature of the variable. The statistical comparison was done with the χ2 test (P<.05 was considered significant) and the odds ratio (OR) was calculated with 95% confidence intervals (95% CI).
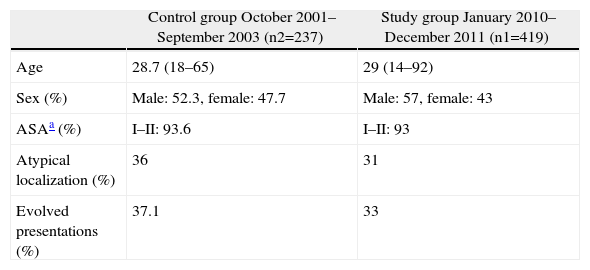
ResultsThe study group included 419 (n1) patients and the control group consisted of 237 (n2). Table 1 summarizes the data of the overall descriptive and homogeneity analyses. Age, gender distribution, the predominance of the American Society of Anaesthesiologists (ASA) index for low risk and the percentages of atypical locations or evolved presentations (gangrenous, perforated or with local or diffuse peritonitis) are consistent with large series of patients with appendicitis, and both groups were homogeneous in all these variables.
Homogeneity and Descriptive Analysis of the Groups.
| Control group October 2001–September 2003 (n2=237) | Study group January 2010–December 2011 (n1=419) | |
| Age | 28.7 (18–65) | 29 (14–92) |
| Sex (%) | Male: 52.3, female: 47.7 | Male: 57, female: 43 |
| ASAa (%) | I–II: 93.6 | I–II: 93 |
| Atypical localization (%) | 36 | 31 |
| Evolved presentations (%) | 37.1 | 33 |
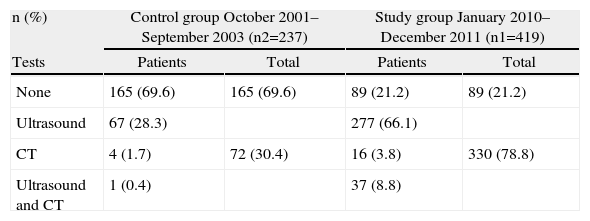
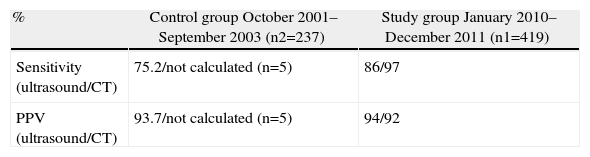
Table 2 shows the number and percentage of examinations performed during both study periods. In the study group, significantly more radiological approaches to diagnosis were observed; physicians were 8 times more likely to have ordered some type of complementary examination in the study group than in the control group (P<.000; OR 8.3; 95% CI: 5.8–12). What is particularly striking is the very low number of CT scans done during the control period (n=5), which prevented our being able to calculate the sensitivity and PPV of CT during that period. The calculation of these parameters for both tests is shown in Table 3. The diagnostic performance parameters of CT (calculated only during the study period) exceeded ultrasound in sensitivity but not in terms of PPV, where both diagnostic tools had equal capability.
Number (and Percentage) of Radiological Tests (Ultrasound and CT) Done During Both Periods.
| n (%) | Control group October 2001–September 2003 (n2=237) | Study group January 2010–December 2011 (n1=419) | ||
| Tests | Patients | Total | Patients | Total |
| None | 165 (69.6) | 165 (69.6) | 89 (21.2) | 89 (21.2) |
| Ultrasound | 67 (28.3) | 277 (66.1) | ||
| CT | 4 (1.7) | 72 (30.4) | 16 (3.8) | 330 (78.8) |
| Ultrasound and CT | 1 (0.4) | 37 (8.8) | ||
P<.000; OR 8.3; 95% CI: 5.8–12.
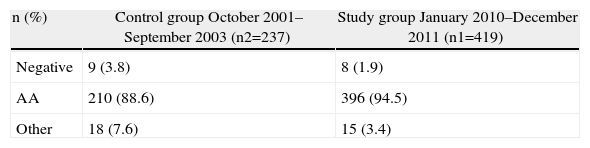
Finally, Table 4 highlights the clinical impact of this change in diagnostic policy. During the study period, a significantly higher percentage of correctly-indicated surgical explorations were done, and the possibility of a patient being treated surgically with an accurate diagnosis had doubled (P<.006; OR 2.2; 95% CI: 1.25–4).
Surgical Explorations and Diagnosis in Both Periods.
| n (%) | Control group October 2001–September 2003 (n2=237) | Study group January 2010–December 2011 (n1=419) |
| Negative | 9 (3.8) | 8 (1.9) |
| AA | 210 (88.6) | 396 (94.5) |
| Other | 18 (7.6) | 15 (3.4) |
Comparison AA vs negative/other groups: P<.006; OR 2.2; 95% CI: 1.25–4.
Classic aphorisms, such as the belief that expert hands can diagnose inflammatory appendicitis with total reliability, lack sufficient scientific basis in the context of modern medicine. Diagnoses based exclusively on symptoms or laboratory AA data continue to be deficient, whether or not scoring systems are used. The most widely used classification system was described by Alvarado, which groups symptoms, signs and laboratory data and assigns patients a score (between 1 and 10) that stratifies their right iliac fossa pain as unlikely, possible, likely or very likely acute appendicitis. The data defending the reliability of this system come from studies with dubious methodological quality that show conflicting results, and publications in the literature suggest the possibility of significant missed diagnoses, even in patient groups with low scores and therefore low clinical probability.9–11
However, several contributions and meta-analyses suggest that the diagnostic efficacy parameters of certain radiological tests, such as ultrasound or CT, are excellent and can impact the percentage of negative surgical explorations. These parameters seem to favor CT over ultrasound in most publications (sensitivity and specificity around 85% for ultrasound and 95% for CT), and reports of erroneous indications have been cut in half (21.5% vs 10%) with systematic preoperative CT.3,12,13 It is also particularly conclusive that studies comparing the negative laparotomy rate in patients with symptoms-based diagnoses vs selected patients with diagnostic radiological support report more favorable results in the latter group, even though (because of the uncertain diagnosis) a higher rate of negative appendectomies is expected.3 This is an inversion of the results of the natural tendency of this bias, which is an overwhelming acceptance of our working hypothesis: undoubtedly, we will significantly reduce the frequency of negative appendectomies by basing the indication for surgery on the combination of clinical and radiological criteria. In this regard, our study is also clear.
There are two potential diagnostic approaches derived from these data. The first would systematically include radiological support in the diagnosis of AA. Many centers have included ultrasound in the diagnostic process of AA due to its speed and safety, but it should always be kept in mind that its diagnostic performance parameters are lower than those of other studies and that it is operator-dependant. Other protocols have also proposed the systematic inclusion of CT in AA diagnosis.3 In terms of reliability and significant increase in accurate surgeries, the results published have been positive.
Meanwhile, the arguments of its critics are based on the effects of radiation or the potential increase in perforated appendicitis due to a delayed diagnosis, but these opinions have not been confirmed by actual data. In any event, even though the time required for a tomographic scan is becoming shorter each day, the fact is that the inclusion of a diagnostic CT in all patients with pain in the right iliac fossa would overload any Radiology Department.
The other diagnostic option is to stratify the risk and establish the indication for radiological support only for patients with diagnostic uncertainty, while directly operating on patients with a high index of suspicion and maintaining patients with very low probability under observation. To position patients with pain in the RIF in one of these strata, a scoring system can be used, such as the Alvarado classification (with reservations, based on the published series9–11), or the overall criteria of the radiologist is another option. Although with recommendation level B and based on class III studies, this is the most widely recommended policy by clinical practice guidelines for the diagnosis of AA.14,15
Given the previous comments made about ultrasound and CT in the diagnosis of AA, it seems prudent to first perform an ultrasound approach and reserve CT for those cases in which ultrasound is not very informative. What is certain is that, while years ago physicians were required to make purely semi-logical diagnoses and only a small number of radiological examinations were done (especially CT, as also seen in our study), today requests for radiological approaches must be accepted (even CT, if necessary) in cases with uncertain diagnoses. Moreover, appropriate logistical efforts should be made to guarantee the availability of these tests in emergency situations.
Our study is not without limitations. The first is derived from its non-randomized design, although all the information comes from the same type of study and the results are consistent with previous publications. Another limitation is the potential selection bias created by choosing the control group from a sample selected for a previous study with an age limit. While the homogeneity analysis was conducted with the most frequently implicated variables with greater diagnostic difficulty, the bias of not including patients older than 65 in the control group would only contribute to an even higher rate of erroneous laparotomies in this group. This would even more emphatically suggest that radiological support in cases of diagnostic doubt would increase the number of explorations with accurate diagnosis.
Lastly, the PPV can be debated with regard to the estimation of sensitivity and PPV from surgical patients (who therefore have a high suspicion of AA), rather than from patients with RIF pain syndrome who come to the emergency department. This situation may overestimate the prevalence parameters. If we consider that the vast majority of patients with undiagnosed AA (false negatives) will ultimately be operated on due to progression of the inflammatory disease, and that all patients with radiological findings compatible with AA are operated on in our setting even at the risk of not having appendicitis (false positives), the fact is that the calculation of sensitivity and PPV of diagnostic radiological examinations from a sample of surgical patients is acceptable. Nevertheless, what cannot be calculated with this assumption is the specificity and NPV due to the absence of the actual number of patients without AA who were correctly diagnosed and discharged from the ER (true negatives). To do so, it would be necessary to examine the diagnostic approaches in the Emergency Department.
Despite these limitations, we believe that the internal validity of the study is sufficient to give enough reliability to the results, which are in line with other publications. Thus, in conclusion, we can infer that radiological support in the diagnosis of acute appendicular disease presents excellent diagnostic accuracy and avoids unnecessary surgical procedures. With the knowledge of these parameters, we have increased its application in recent years, resulting in proper medical practice, based on the available evidence. Although diagnostic protocols that systematically include these tests must be respected (as they are also supported by evidence), it would seem more logical to accept that the risk should be stratified by clinical and analytical parameters, with or without the use of classification systems, and that the request for radiological support should be restricted to those cases with diagnostic uncertainty.
It is recommended to start first with an ultrasound approach and to reserve CT for cases in which ultrasound provides no conclusive information. Last of all, in today's day and age, exploratory surgery should not be accepted as an exclusive diagnostic tool in cases of right iliac fossa pain syndrome without previous radiological testing.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Aranda-Narváez JM, Montiel-Casado MC, González-Sánchez AJ, Jiménez-Mazure C, Valle-Carbajo M, Sánchez-Pérez B, et al. Empleo, eficacia y repercusión clínica del apoyo radiológico al diagnóstico de la apendicitis aguda. Cir Esp. 2013;91:574–578.