Low back pain is a worldwide prevalent musculoskeletal condition in the general population. In this sense, the pulsed electromagnetic fields (PEMF) therapy has shown significant clinical benefits in several musculoskeletal conditions.
ObjectiveTo assess the effectiveness of the PEMF therapy in reducing pain and clinical symptomatology in patients with low back pathological conditions.
MethodsIt was performed a comprehensive database search using Pubmed, Scopus, Cochrane Library and PEDro databases to assess the effectiveness of the PEMF therapy in reducing pain and clinical symptomatology in patients with low back pathological conditions. The search was performed from January 2005 to August 2015 and conducted by two independent investigators, which scrutinize the reference list of most relevant studies. The methodological quality was assessed by the PEDro scale and the level of evidence was set according Oxford Center for Evidence-Based Medicine scale.
ResultsSix studies were eligible inclusion on the qualitative analysis and five into the quantitative analysis, scoring an overall 6.8 points according the PEDro scale. The studies showed heterogeneity concerning the intervention protocols. Nevertheless, the effect sizes’ indicated a clear tendency to reduction of the pain intensity favoring the PEMF groups, reaching a minimal clinically important difference.
ConclusionPEMF therapy seems to be able to relieve the pain intensity and improve functionality in individuals with low back pain conditions. Further research is needed regarding PEMF effects on the different conditions of low back pain, with standardized protocols, larger samples and adjustment for low back pain confounders in order to achieve stronger conclusions.
Low back pain is a very common health problem in general population and one of the major reasons for medical treatment seeking. It is expected that between 60 and 80% of the world population will experience low back pain during lifetime,1 with 65% being recurrent and longstanding episodes. Low back pain can be caused by different etiologies, such as muscle or ligament strains, herniated discs, arthritis, alteration in the curvature of the spine or osteoporosis related fractures but, the majority of the patients do not have a clinically identified problem.2 Despite the variety of treatments available, no modality or therapeutic approach has stand out as a definitive solution.3 Thus, there is still a demand for new approaches, less invasive and free of side effects.
The risk/benefit ratio in pharmacotherapy for low back pain conditions often does not have strength enough to persist with the drugs usage. Moreover, the risk of pharmacologic addition, potential side-effects and adverse events, as well as long-term toxicity may weaken the potential benefit of the pharmacotherapy approach.4,5 In this sense, the pulsed electromagnetic fields (PEMF) therapy can play an important role in the pain relief since is a drug-free, non-thermal, with low risk that works to enhance cellular activity healing and repair.3 Therefore, it could be an option to the non-steroidal anti-inflammatory drugs (NSAIDs) medication, avoiding several potential side-effects from chronic NSAIDs usage.
The PEMF therapy is based in low frequency signal, with a wide range of frequencies, which will produce membrane disturbances and activation of multiple intracellular pathways.6,7
It has been reported that PEMF therapy yields several benefits into the bone unification, acute pain relief, wound healing, edema and inflammation control, as well as, chronic pain associated with connective tissue (cartilage, tendon, ligaments and bone) injury and joint-associated soft tissue injury, osteoarthritis, fibromyalgia, osteoporosis, skin ulcers and further potential applications.8–11 Along this line, many reviews have been performed to assess the PEMF effectiveness in several conditions. In this sense, the PEMF showed moderate7 or no benefits in knee osteoarthritis,12 a beneficial tendency on the bone growth stimulation in acute fractures13 and efficient in relieving pain and enhancing bone formation in osteoporosis.14
Although the use of PEMF therapy in low back pain is growing and there is substantial investigation on this topic, a systematization of its effects on the low back pain is still lacking. Therefore, this study aims to search for randomized controlled trials that assessed the effectiveness of the PEMF therapy in reducing pain symptomatology in patients with low back pathological conditions.
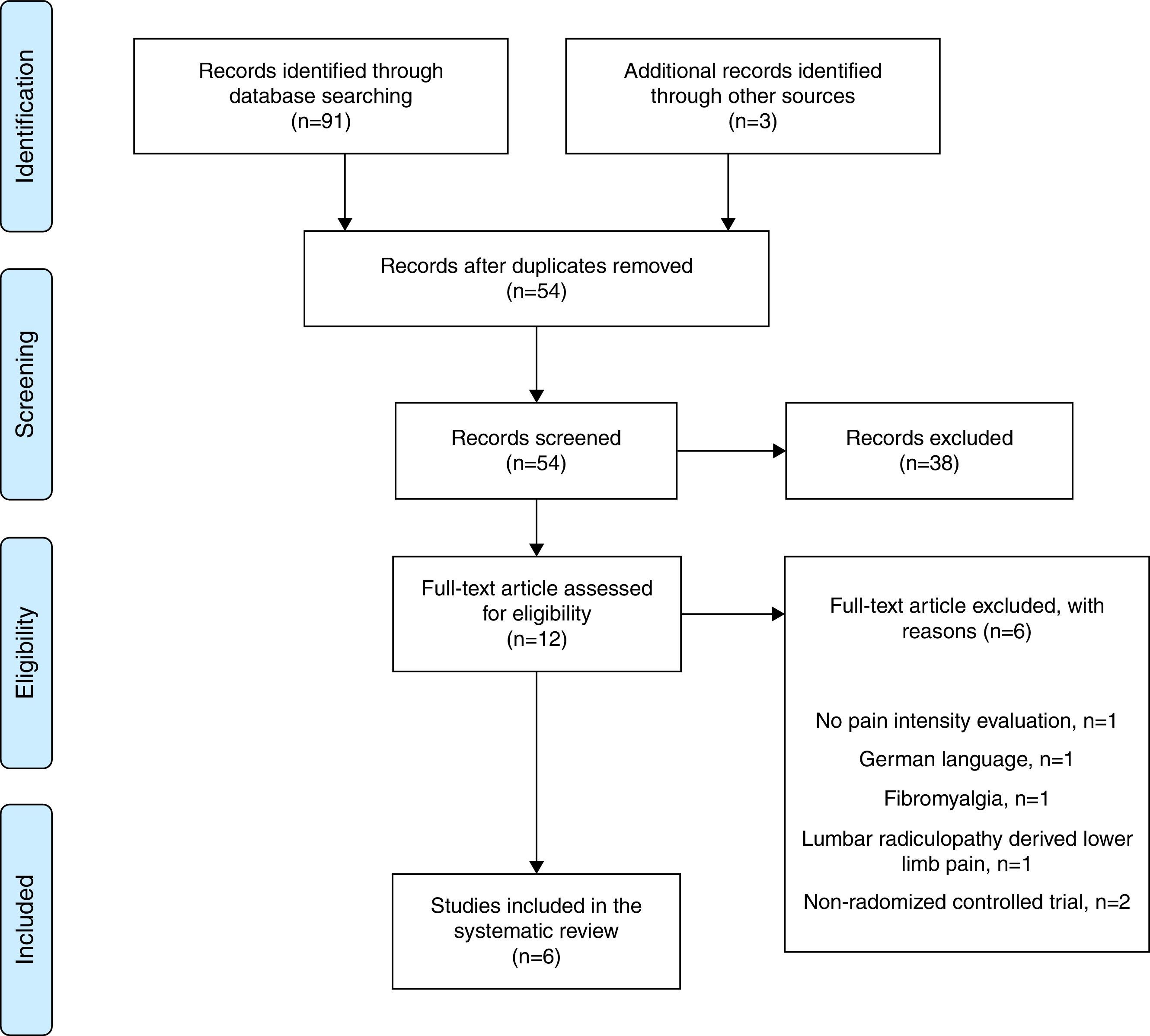
MethodsSearch strategyThe systematic review was conducted according the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, which aims to improve the standard of reporting of systematic reviews and meta-analyses.15 Additionally, the protocol for this review was à priori registered in the International Prospective Register of Systematic Reviews (PROSPERO) (http://www.crd.york.ac.uk/prospero/; ID: CRD42015025308).
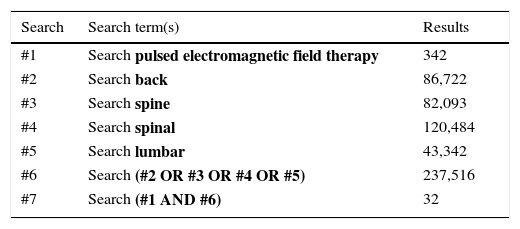
It was conducted a comprehensive database search using Pubmed, Scopus, Cochrane Library and PEDro, searching for relevant studies that assessed the efficacy of the PEMF therapy on reducing pain on individuals with low back pain. The search was performed according the following key-words: pulsed electromagnetic field therapy; back; spine; spinal; lumbar; and further combined with the Boolean operators (AND; OR). An example of the search can be seen in Table 1. The reference list of most relevant studies was scanned for additional studies in order to achieve the greatest number of available studies on the scientific literature. All searches were comprised to the period of January 2005 to August 2015 and were conducted by two independent investigators (R.A., H.D.), which confronted both results to check for overlapping; any disagreements were discussed by until consensus was reached.
Study selectionAll titles and abstracts from the selected databases were screened. After, the potential relevant studies were selected and retrieved, full texts were read in order to apply the eligibility according the following inclusion criteria: (1) assessment of pain outcome; (2) use of pulsed electromagnetic field therapy; (3) prospective design; (4) randomized controlled trials; (5) English language studies. For exclusion criteria it was determined: (i) other reviews or meta-analyses; (ii) clinical commentaries or expert opinions; (iii) case series; (iv) non-randomized controlled trials; (v) animal studies; (vi) skeletally immature population.
Data collection and extractionTwo independent investigators (R.A., H.D.) retrieved all the information and matched for consensus. The main outcome of interest was the quantification of intensity of pain overtime. Thus, after the application of the eligibility criteria and the included studies were determined, the studies were analyzed based on sample demographics, study's aim, statement of conflict of interest, study duration and follow-up (period of time and percentage), PEMF devices used, treatment window, intervention protocol, parameters assessed (clinical and functional) and most significant results.
In addition, the figures of pain intensity and the Oswestry Disability Index were assessed based on their means and standard deviation values and calculated their mean differences, i.e., difference between the study's end-point and baseline values. Additionally, the Cohen's effect size, within the 95% confidence intervals (CI) was calculated. The effect sizes were computed by subtracting the experimental group mean to the control group mean and further divided by the pooled standard deviations of both groups.16,17 Thus, a positive effect reflects a greater decrease on the pain intensity toward the experimental group. The 95% CI provides information concerning the variability of the observed effect size, its precision, as well as the accuracy with which the interval contains the population parameter (i.e., the true value). The standardized Cohen effect sizes were interpreted according to the guidelines established by Cohen17 in which values <0.20 are trivial or not substantial, 0.20 and 0.49 are small but substantial, 0.50 and 0.79 are moderate, and ≥0.80 are large. In case of missing values (means and/or standard deviations), the authors from the respective studies were contacted in order to obtain them.
Methodologic quality assessmentThe PEDro scale in order to assess the methodological quality (external validity, internal validity and statistical reporting) and the level of evidence was set according the Oxford Center for Evidence-Based Medicine (CEBM) scale.18 PEDro scale has been reported to be a valid and reliable tool to measure the methodological quality of interventional clinical trials.19,20 These parameters were independently assessed by two authors (R.A., H.D.) and all disagreement were resolved until consensus was reached.
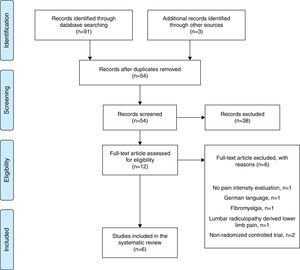
ResultsStudy selectionThe database and hand search yielded 91 titles, which were reduced after duplicates removal and title/abstract reading to 12 full-text articles that were screened for eligibility. After screening, 6 studies were excluded21–26 which the reasons for exclusion are highlighted in the PRISMA flow chart (Fig. 1). The remaining 6 studies were eligible inclusion on the qualitative analysis and 5 into the quantitative analysis.
Description of studiesIn Table 2 are presented the characteristics of the 6 included original studies. Overall, the studies included a total of 210 participants (90 men and 120 women), with an overall mean age of 43.3 years old. All the included participants reported complains of low back pain, however with different etiologies: generalized low back pain27; acute non-specific low back pain3; discogenic lumbar radiculopathy28; failed back surgery syndrome pain26; chronic low back pain.4,29
Characteristics and main results of the included studies.
| References | Demographics | Aim | Duration/follow-up | Intervention protocol | Treatment window | Parameters assessed | Results | Follow-up (%) |
|---|---|---|---|---|---|---|---|---|
| Krammer et al.3 | n=40 20M/20F 33 y.o. | Explore the additional benefits of PEME used as an adjunct to physiotherapy in treatment of acute non-specific low back pain | 1 weeks 4 weeks | Experimental group: physiotherapy and PEME Control group: physiotherapy and placebo 7 days of PEME and physiotherapy 2×/week for 4 weeks | During 7 days | ODI; NPRS; Patient Specific Functional Scale; Level of Function | Both groups showed improvements on ODI, Patient Specific Functional Scale and NPRS scores over both follow-up periods (p<0.05); however, without any significant differences between them (p>0.05) | 100 |
| Park et al.30 | n=38 11M/27F 32 y.o. | Investigate the efficacy of PEMF on the lumbar myalgia | 2 weeks 3 weeks | Experimental group: PEMF Control: sham device 6 times, 3×/week for 2 weeks | 10min day, 3 days a week, during 2 weeks | VASB; VASP; Korean version of: ODI; SF-36; EQ-5D; BDI; RMDQ | Significant decrease of VASB (p<0.007), VASP (p<0.015) and RMDQ in PEMF group in comparison to the control group | 100 |
| Oke et al.27 | n=16 9M/7F 42.8 y.o. | Assess the therapeutic efficacy of PEMF in treatment of back pain | 5–9 days N.R. | Experimental group: analgesics+ NSAIDs and PEMF Control group: analgesics Both groups received soft tissue manipulation with an analgesic gel 4×/day (2h) | 4 times a day during 2h (Min 5 days and Max 9 days of treatment) | NPRS; Modified version of Functional Activity Scale | Significant differences on experimental group on pain rating scores (p>0.061) and functional activity score (p>0.000) | N.R. |
| Omar et al.28 | n=40 11M/29F 38.8 y.o. | Evaluate the effect of PEMF in patients with discogenic lumbar radiculopathy | 3 weeks N.R. | Experimental group: PEMF every day for 3 weeks Control group: standard medical treatment and placebo | 20min day, during 3 weeks | VAS; ODI; Radiological evaluation; Somatosensory evoked potentials | Significant reduction in pain severity (p<0.024) Significant improvement in modified OSW (p<0.001) Improvement of SSEPs (p<0.05) | 100 |
| Harden et al.4 | n=40 20M/20F 40.3 y.o. | Evaluate the TEMF on chronic low back pain | 2 weeks 6 weeks | Experimental group: TEMF Control: sham device | 40min session, 10 sessions in 3 weeks | VAS; MPQ-SF; BDI; STAI; QPDI; Physical performance tests | Although both groups improved over time (p<0.05), the experimental group improved significantly over sham treatment during the 2-week follow-up period (20.5% reduction in pain, p=0.003) | 100 |
| Lee et al.29 | n=36 19M/17F 75 y.o. | Study the effect of PEMT in patients with chronic low back pain | 3 weeks 7 weeks | Experimental group: active PEMT Control group: placebo 3×/week for 3 weeks | The 15-min treatment 3 times a week for 3 weeks | NPRS; Revised ODI | PEMT reduced pain and disability in patients with chronic low back pain (p<0.05) | 100 |
PEME – Pulsed Electromagnetic Energy; PEMF – pulsed electromagnetic fields; TEMF – Therapeutic Electromagnetic Fields; ODI – Oswestry Disability Index; NPRS – Numeric Pain Rating Scale; M – Male; F – Female; y.o. – years old; N.R. – not reported; VAS – visual analogue scale; VASB – visual analogue scale for discomfort for low back pain; VASP – visual analogue scale for pain intensity; SF-36 – Short-Form 36; EQ-5D – EuroQol-5 Dimension (Korean adapted); BDI – Beck's Depression Inventory (Korean adapted); RMDQ – Roland-Morris Disability Questionnaire (Korean adapted); NSAIDs – nonsteroidal anti-inflammatory drugs; IL-4/IL-6 – interleukins 4 and 6; MPQ-SF – McGill Pain Questionnaire – Short Form; BDI – Beck Depression Inventory; STAI – State-Trait Anxiety Inventory; QPDI – Quebec Pain and Disability Index.
The inclusion criteria varied across the studies. Nonetheless, across the included studies some similarities were found. All of the studies were performed in adult populations with clinically evaluated low back pain. A visual analogue scale above 5 points and a numeric rating scale above 4 points were also considered in Park, Sun, Lee, Kang, Lee, Hwang and Cha30 and Lee, Kim, Lim, Lee, Choi, Park, Lee and Lee29 studies, respectively. The presence of a cardiac pacemaker or other electronic implants were the only exclusion criteria enclosed in all studies. Other exclusion criteria were study-specific related comorbidities.
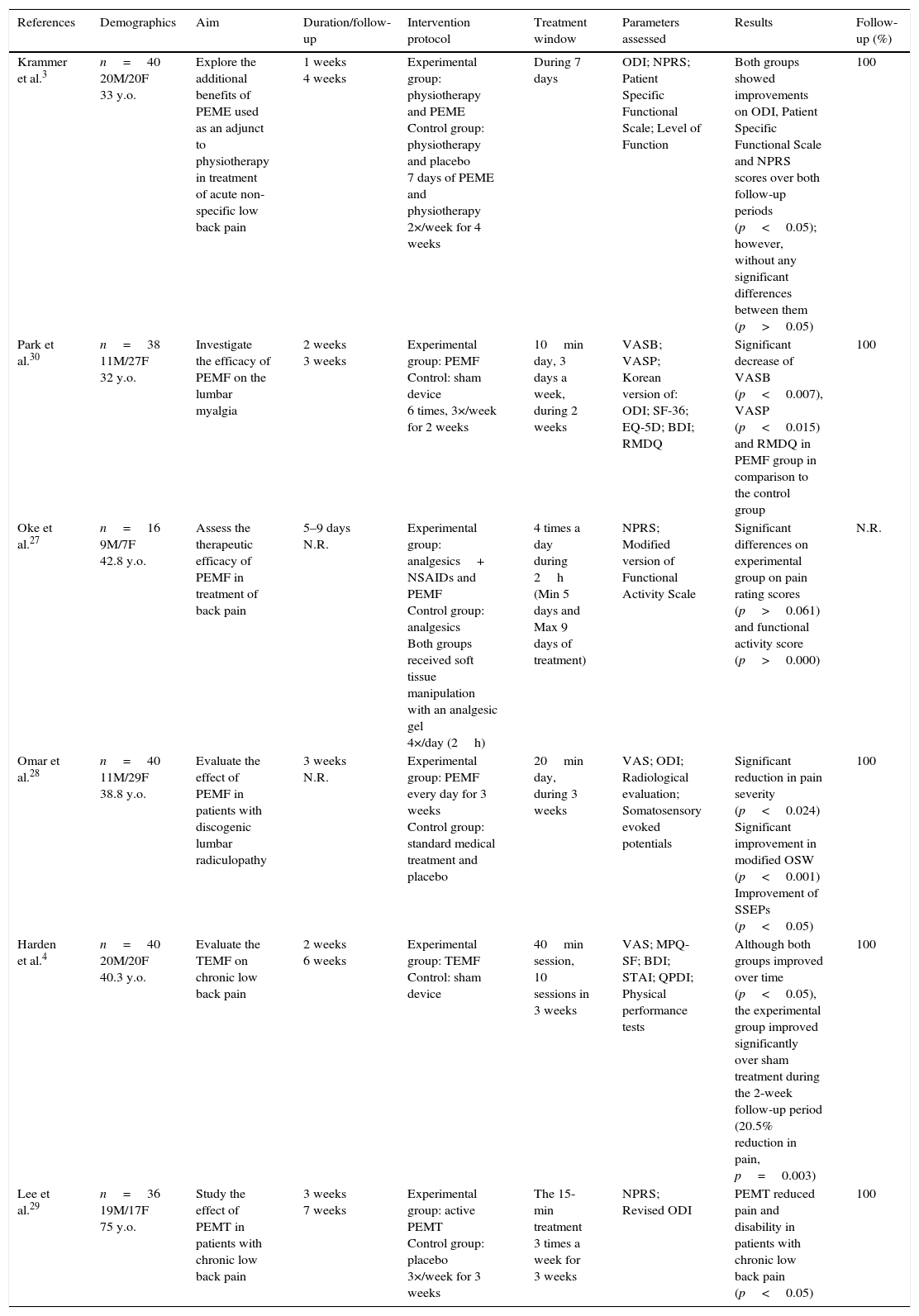
Generally, the studies enrolled the use of different devices, however with the same objectives and principles of PEMF therapy application. Their description can be seen in Table 3. The PEMF therapy was often compared with placebo interventions (comprising sham devices) or analgesic medication. Moreover, the studies showed heterogeneity concerning the PEMF therapy protocols, where the duration of the application ranged from 5 days to 3 weeks, and the frequency of the application from 4 times a day to just twice a week. The follow-up period also showed heterogeneity, ranging from 3 to 7 weeks,3,4,29,30 or in some cases it was not reported.27,28 The follow-up percentage was very satisfactory, being above the 85%, excepting Oke and Umebese27 study which did not report the follow-up.
PEMF devices used across the included original studies and its reported characteristics.
| References | Devices | Additional reported information |
|---|---|---|
| Krammer et al.3 | RecoveryRx (BioElectronics Corp) | Carrier frequency of this device is 27.12MHz. Pulse rate of 1000pulsesp/s and a 100μs burst width. Magnetic flux density or field strength of the device is 0.03mT |
| Harper et al.26 | Provant Therapy System Model 4201 (Regenesis Biomedical Inc., Scottsdale, AZ, USA) | Carrier frequency of this device is 27.12MHz. Pulse durations are 42±4μs repeated every 1000±25μs |
| Park et al.30 | NUGA MRT-II (NUGA MEDICAL, Wonju, Korea) | The maximum strength of PEMF was 820mT with pulse frequency of 8.56kHz |
| Oke et al.27 | EMpulse, Model 301 (EM-Probe Technologies, USA) | Non reported |
| Omar et al.28 | NR | Field strengths ranged from 5 to 15Gauss (G) and the frequency ranged from 7Hz to 4kHz |
| Saggini et al.24 | NR | Electromagnetic fields of low intensity with inferior frequencies at 100kHz |
| Lee et al.29 | CR-3000 system (CR Technology Co., Kyungki-do, Korea) | Carrier frequency of this device range from 1 to 50MHz. The magnetic pulse produced is biphasic and has a pulse width of 270μs. Maximum output amplitude of 2T |
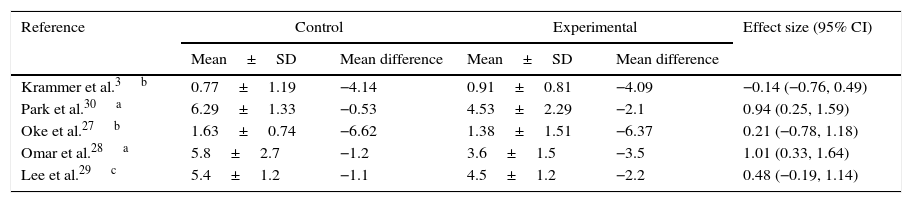
The main outcome of interest was the quantification of the intensity of low back pain. All studies reported reduction on the pain intensity, at least, on the experimental group. When assessing the mean difference on pain intensity from baseline to the end-point, it was found a reduction on the pain intensity from 2.1 to 6.4 points out of 10 on the visual analogue scale or on the numerical rating pain scale (Table 4); however, when analyzing the effect sizes, two studies showed a small effect size27,29 and two studies showed a large effect size.28,30
Quantification of pain intensity and effect sizes by group.
| Reference | Control | Experimental | Effect size (95% CI) | ||
|---|---|---|---|---|---|
| Mean±SD | Mean difference | Mean±SD | Mean difference | ||
| Krammer et al.3b | 0.77±1.19 | −4.14 | 0.91±0.81 | −4.09 | −0.14 (−0.76, 0.49) |
| Park et al.30a | 6.29±1.33 | −0.53 | 4.53±2.29 | −2.1 | 0.94 (0.25, 1.59) |
| Oke et al.27b | 1.63±0.74 | −6.62 | 1.38±1.51 | −6.37 | 0.21 (−0.78, 1.18) |
| Omar et al.28a | 5.8±2.7 | −1.2 | 3.6±1.5 | −3.5 | 1.01 (0.33, 1.64) |
| Lee et al.29c | 5.4±1.2 | −1.1 | 4.5±1.2 | −2.2 | 0.48 (−0.19, 1.14) |
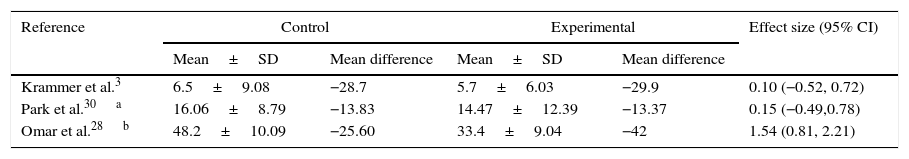
Regarding the functionality assessment, several scales and indexes were used to quantify the participant's function: Oswestry Disability Index3,28–30; Patient Specific Functional Scale3; Korean version of Roland-Morris Disability Questionnaire30; Modified version of Functional Activity Scale27; Quebec Pain and Disability Index.4 When focusing the Oswestry Disability Index alone, which was the most commonly reported scale for measuring the functionality, despite its large mean differences from baseline to end-points (Table 5), the effect sizes were small (<0.20). The study of Omar, Awadalla and El-Latif28 was an exception, achieving a large effect size (>0.80), however using an adapted Oswestry Disability Index.
Oswestry Disability Index and effect sizes by group.
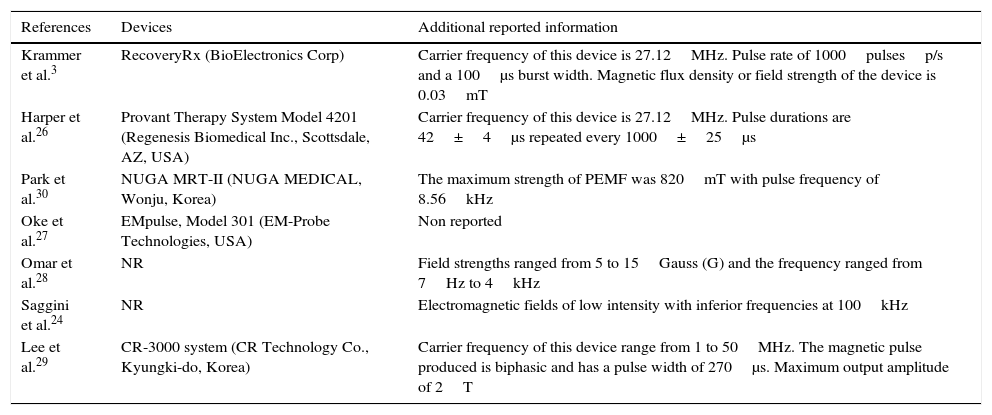
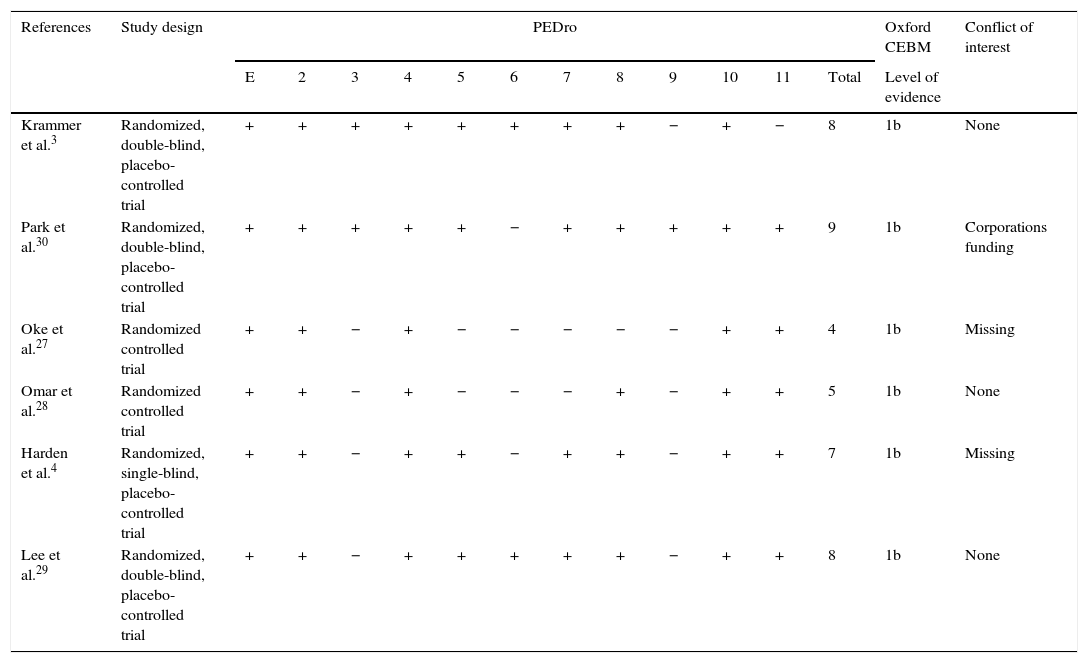
The mean score of methodological quality of the included studies was 6.8±1.9 (range 4–9) out of 10 points according PEDro scale and the level of evidence was 1b in all studies (Table 6).
Methodological quality of the included studies.
| References | Study design | PEDro | Oxford CEBM | Conflict of interest | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| E | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | Level of evidence | |||
| Krammer et al.3 | Randomized, double-blind, placebo-controlled trial | + | + | + | + | + | + | + | + | − | + | − | 8 | 1b | None |
| Park et al.30 | Randomized, double-blind, placebo-controlled trial | + | + | + | + | + | − | + | + | + | + | + | 9 | 1b | Corporations funding |
| Oke et al.27 | Randomized controlled trial | + | + | − | + | − | − | − | − | − | + | + | 4 | 1b | Missing |
| Omar et al.28 | Randomized controlled trial | + | + | − | + | − | − | − | + | − | + | + | 5 | 1b | None |
| Harden et al.4 | Randomized, single-blind, placebo-controlled trial | + | + | − | + | + | − | + | + | − | + | + | 7 | 1b | Missing |
| Lee et al.29 | Randomized, double-blind, placebo-controlled trial | + | + | − | + | + | + | + | + | − | + | + | 8 | 1b | None |
E: eligibility criteria (this item is not used to calculate the total score); 2: random allocation; 3: concealed allocation; 4: baseline comparability; 5: participant blinding; 6: therapist blinding; 7: assessor blinding; 8: <15% dropout; 9: intention-to-treat analysis; 10: between-group statistical comparisons; 11: point estimate and variability statistical measures.
The most common methodological limitation across the studies was the lack of “intention-to-treat” analysis, which was only performed by Park, Sun, Lee, Kang, Lee, Hwang and Cha.30 Another major methodological issue was the concealment of the randomization, which also only performed in two studies.3,30 Lack of subjects and the assessors blinding was also a methodological limitation across the studies, especially when concerning the therapist, once only two studies blinded the therapists.3,29
DiscussionThe main finding of this systematic review is that PEMF therapy seems to reduce the pain intensity and enhance better functionality in individuals with low back pain.
When used alone, the PEMF seem to have great effect in reducing the pain intensity in low back patients, independently of the low back pain condition.28–30 However, when added to other standard therapies (such as, standard physiotherapy3 or analgesic therapy27) seems to do not add additional effect to the standard therapy.
Measuring the intensity of pain related to the different low back conditions plays a key role in following up the patient's recovery. However, because of the subjective nature of pain, clinical importance is not always easy to determine.31 In an effort to overcome this variability, measures of improvement usually adjust for the individual's baseline by calculating raw change or percent change.32
The PEMF therapy has been pointed out as an effective and relatively safe tool for conservatively treat the low back pain.4,27–30 Furthermore, it has a high potential of compliance due to its low risk of side-effects and high tolerance.29 In fact, when analyzing the pain intensity alone, the included studies effect sizes indicate a tendency to a greater reduction on pain intensity for the PEMF groups. Nevertheless, when compared to standard therapies (such as, physiotherapy3 or analgesic therapy27) seemed to produce a low effect or no effect at all. Considering the minimal clinically important difference (MCID) – minimal change in an outcome score that is clinical meaningful for the patients – all studies showed that the PEMF was able to produce a clinical meaningful pain reduction since the mean differences were higher than the minimum 2-point suggested by Childs, Piva and Fritz.33
Several scoring systems are frequently used in the clinical environment in order to measure the disability related to the low back conditions, which should be reliable, valid and sensitive to clinically relevant changes, taken into account both patients’ and physicians’ perspective and is short and practical to use.34–37 Although, impairments such as decreased range of movement or reduced straight leg raise can be clinically observed by physiotherapists, the direct observation of activity restriction is not sufficient. Therefore, the physiotherapists have the need to rely on the patient's self-report assessment to measure the impact of low back pain on daily activities.34
Several studies have been demonstrating the PEMF effectiveness in reducing the disability related to the low back pain.27–30 Regarding the studies included in this systematic review, the disability assessment was mostly made by the Oswestry Disability Index,38 showing improvements after application of PEMF therapy, however with small effect sizes. Nevertheless, the MCID's were above the minimum recommended by Ostelo, Deyo, Stratford, Waddell, Croft, Von Korff, Bouter and de Vet39 – between 6–10 points or 12–20 percent – indicating a meaningful improvement on the patient's functionality. On the other hand, Omar, Awadalla and El-Latif28 showed a large effect size toward the PEMF group (d=1.54, 95% CI: 0.81, 2.21) using the Modified Oswestry Low Back Pain Disability Questionnaire, obtaining a 42% mean reduction after daily applications of PEMF therapy for 3 weeks. Still, some caution should be taken when considered this study since they used an adapted score.
Other usual subjective scores – generic and disease-specific – to evaluate the low back functionality have already been explored during the last decades and are currently available for orthopedic clinical and research practice.35 In this sense, beneficial results were reported in the included studies using different scores: Patient Specific Functional Scale3; Korean version of Roland-Morris Disability Questionnaire30; Modified version of Functional Activity Scale27; Quebec Pain and Disability Index.4 Although the studies showed improvements from the baseline to the study's end-point, two studies did not achieved significant improvements toward the PEMF group when compared to the control group.3,4
Due to the comprehensiveness and complexity within the low back pain umbrella and allied to its associated multiple etiologies, specific attention should be directed to the characteristics of subgroups of responders.4 In this line, the studies included in our systematic review explored the PEMF therapy effectiveness in different conditions of low back pain: generalized low back pain27; acute non-specific low back pain3; discogenic lumbar radiculopathy28; lumbar myalgia30; chronic low back pain.4,29 Due to the high heterogeneity of the different low back pain conditions of the original studies included in this systematic review, and the small sample sizes (ranging from n=16 to n=40), no strong recommendations can be drawn regarding the non-specific low back pain or its several conditions.
Moreover, it was found high heterogeneity between the protocols of PEMF therapy of the different studies, differing in the devices used and its parameters (frequency, pulse rate and width, magnetic flux density, among others), duration and frequency of application (4 times a day until 3 times a week) and type of application. Hence, considerable caution should be taken when comparing the results from the different studies, highlighting the importance in achieve the most effective dosage and standardized protocol parameters. In this line, future studies should shift their focus on analyzing the different mechanisms of action (e.g., myofascial, radiculopathic, among others) and subgrouping (acute or chronic, specific or generalized, mechanical or idiopathic) the individuals with low back pain in order to evaluate the effects of PEMF therapy in these different groups of low back pain and identify the responsiveness of each specific group. Thus, it will be possible to achieve the most effective PEMF protocol to the most suitable subgroup of patients.
Generally, the studies showed a good methodological quality according the PEDro scale, with a mean of 6.3 points out of 10 possible, which is above the recommended by.40 The studies showed a good methodological quality, i.e., good external and internal validity, providing sound interpretation of the data. However, precisely in the internal validity, some limitations were found across the studies that could provide additional bias to the results: lack of “intention-to-treat” analysis; lack of randomization concealment; lack of blinding of subjects, therapists and assessors. Moreover, another important limitation was the statement of conflict of interest, where only three studies stated that had no conflict of interest at all. Two other studies did not make any statement about conflict of interest whatsoever and two studies reported funding upon the study's conduction.
Study limitationsTo the best of our knowledge, no other systematic review has investigated the therapeutic effects of PEMF specifically on low back pain. Moreover, it was used 2 independent reviewers for screening and critical appraisal and registered our protocol which could have reduced the bias within the systematic review. Still, there are some limitations that are needed to be pointed out. Firstly, the low number of studies available on the scientific literature that investigates the effectiveness of PEMF on low back pain is scarce, and even fewer if we consider de low back pain subgroups. Another limitation is the small size of the studies samples, which should be larger in order to provide power to the conclusion taken from the results. Also, the lack of data (means and standard deviation values) was a limitation in some studies, and the wide range of devices and low back pain conditions, precluded the systematization of the quantitative data. The search was restricted to English language studies; however, previous work demonstrated that the restriction to English language studies on systematic reviews does not provide additional bias.41–44 Furthermore, the studies did not made an adjustment for confounders (e.g., volume of analgesic medication consumption or psychosocial variables), which could lead to further biased results. These confounders may mix with the primary exposure or outcome and bias the true relationship of interest.45
ConclusionIn conclusion, the evidence within this systematic review demonstrates that the PEMF therapy seems to be able to relieve the pain and improve functionality in individuals with different low back pain conditions. However, when added to a standard therapy, it seems to do not add any beneficial effect. Nonetheless, due to the low risk associated, it can be a potential alternative to the conventional pharmacological therapy. The lack of studies in this theme warrants further research on PEMF effects on the different conditions of low back pain, with standardized protocols, larger samples and adjustment for low back pain confounders in order to achieve stronger conclusions.
DisclosureWe certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated. All authors have read and approved the final manuscript.
Conflicts of interestThe authors declare no conflicts of interest.